Medical editor: Strokina O.A. - therapist, functional diagnostics doctor. September, 2021.
ICD-10 code: I35.0, I06.8, I35.8.
Aortic insufficiency is a malfunction of the aortic valve with the formation of reverse blood flow from the aorta into the cavity of the left ventricle. Symptoms directly depend on the amount of blood entering the ventricle. Diagnosis of pathology is possible only with the help of echocardiographic examination (ultrasound of the heart). Treatment also depends on the degree of deficiency and may involve both conservative and surgical techniques.
Aortic insufficiency is a heart defect that is characterized by the development of regurgitation (backflow of blood) on the aortic valve during the relaxation phase of the heart muscle. As a result, blood from the aorta flows back into the ventricle. There is an overflow of its volume, which in the future may threaten the expansion of the cavity of the left chambers of the heart with the development of heart failure.
During the contraction phase, the left ventricle ejects blood into the aorta, after which the ventricular relaxation phase begins. At this moment, the blood tends to return back. Her path is blocked by 3 leaflets of the aortic valve, which are “sacs”. As they fill with blood, the valves straighten, close with each other and completely close the aortic opening.
On the mitral and tricuspid valves, a small discharge of blood in the opposite direction is normally allowed, and the term “insufficiency” is not used here. In the case of the aortic valve, even minimal regurgitation is a pathology that needs to be monitored.
Causes and risk factors
Aortic valve insufficiency develops due to loose closure of the valves during the relaxation phase of the ventricles, which can develop for a number of reasons:
- idiopathic (unknown cause) dilation of the aorta;
- congenital defects of the aortic valve (usually bicuspid aortic valve);
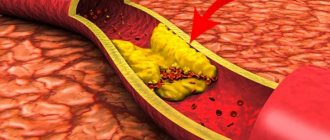
- sclerosis of the valves (due to atherosclerosis);
- rheumatism;
- infective endocarditis;
- arterial hypertension;
- myxomatous degeneration (disorder of connective tissue development);
- dissection of the ascending aorta;
- Marfan syndrome;
- aortic valve injuries;
- ankylosing spondylitis;
- syphilitic aortitis;
- rheumatoid arthritis.
Most of these causes lead to chronic aortic insufficiency, which can be asymptomatic for a long time. Others, in particular infective endocarditis, aortic dissection, and trauma are often accompanied by a sudden development of severe aortic insufficiency. This leads to serious hemodynamic disturbances. As a result, much less blood reaches vital organs: the brain, kidneys, liver, heart.
Causes
The pathology develops during the period of intrauterine development, therefore it is a congenital heart defect. This happens between 6 and 8 weeks. During this period of time, the active process of formation of internal organs in children begins. The two doors are fused together, forming only two moving parts. They take on the functions of the missing component of the heart muscle. In a child, this pathology develops under the influence of a number of provoking factors. The main reasons for the formation of a bicuspid aortic valve include:
- suffered by the mother during the period of gestation of various infectious diseases;
- the influence of radiation, exposure caused by X-ray examination;
- harmful effects of the environment due to poor ecology;
- severe stress, anxiety, psycho-emotional disorders and shocks;
- abuse of alcohol and tobacco products while carrying a baby;
- a predisposition that is inherited if the baby’s parents have cardiovascular system defects;
- genetic predisposition to pathologies associated with connective tissues.
If parents have a bicuspid aortic valve as a congenital pathology, when planning conception and during gestation, it is necessary to carefully monitor all processes, carry out comprehensive diagnostics and take timely measures to ensure the normal functioning of the baby’s cardiovascular system.
Symptoms
In a child, a congenital pathology may not manifest itself in any way for a long time. Symptoms can intensify as he grows up and gradually increases the load on his body, which is in the stage of active development and formation. There are cases when a congenital valve defect was discovered when the child reached adolescence and adulthood. With such congenital heart disease as a bicuspid aortic valve, symptoms manifest themselves in the form of the following characteristic signs:
- Strong pulsation, which is felt in the neck, head or projection of the heart muscle. The pulsation intensifies when the patient assumes a supine position. Such symptoms manifest themselves due to high myocardial emissions and elevated pulse rates.
- Sinus type tachycardia. Its manifestations are characterized by rapid heartbeat. It can occur for no apparent reason, that is, in a state of rest.
- Fainting, dizziness. They are observed quite often in patients. They can develop with moderate physical activity, or when a person suddenly changes the position of his body. This happens if the patient stands up suddenly. These symptoms are caused by a lack of blood circulation in the brain. Such signs are relevant when serious changes occur in the structure of the valves.
- Dyspnea. It first appears if the patient has undergone significant physical exertion. But over time, symptoms are observed even in a state of complete rest. If the systolic function assigned to the left ventricle decreases, the person exhibits signs of orthopnea. As the disease progresses, myocardial asthma and pulmonary edema gradually develop. Because of them, the patient faces dangerous attacks of suffocation.
- Increased and excessive fatigue with minimal activity, a feeling of general weakness throughout the body.
- A person’s vision noticeably decreases, even if it was initially 100%.
- In the region of the myocardium, pain is felt behind the chest, which has no emotional or physical provoking factors. Can be observed at rest. If the aortic valve is severely damaged, the pain becomes pressing and squeezing, lasts for a long time and does not go away after taking potent drugs. The most difficult pain for the patient is the attacks of pain that occur at night. At the same time, sweat is actively released. This condition is caused by hypertrophy of the affected ventricles.
Only hardware diagnostics can detect a bicuspid aortic valve in a person as a congenital pathology of the cardiovascular system. Therefore, at the first signs, seek advice from a cardiologist. If symptoms are detected in time, the diagnosis is confirmed and treatment is started, the functional cardiovascular system will suffer minimally. It is often possible to return patients to normal life and restore blood flow. Prediction is made based on the results of the examination and the therapeutic methods prescribed for treatment.
Types and stages
For aortic regurgitation, doctors use a classification based on the severity of regurgitation (backflow of blood). the degree is determined only by a functional diagnostics doctor based on the results of echocardiography:
- Soft (light);
- Moderate;
- Expressed.
There are many ways to define it. But all of them are possible thanks to Doppler research. All echocardiography devices have this function. It allows you to detect pathological flows inside the heart using an ultrasound sensor. One way or another, this is the most objective assessment of the severity of aortic insufficiency.
Acute and chronic deficiency are also distinguished. This is largely a clinical classification based on symptoms and how quickly they develop.
Classification
Several classifications of congenital heart defects have been proposed, common to them is the principle of subdividing defects according to their effect on hemodynamics. The most general systematization of defects is characterized by combining them, mainly according to their effect on pulmonary blood flow, into the following 4 groups. I. Defects with unchanged (or slightly changed) pulmonary blood flow: anomalies in the location of the heart, anomalies of the aortic arch, its coarctation, aortic stenosis; pulmonary valve insufficiency; mitral stenosis, atresia and valve insufficiency; triatrial heart, defects of the coronary arteries and conduction system of the heart.
II. Defects with hypervolemia of the pulmonary circulation: 1) not accompanied by early cyanosis - patent ductus arteriosus, atrial and ventricular septal defects, Lutambashe syndrome, aortopulmonary fistula; 2) accompanied by cyanosis - tricuspid atresia with a large ventricular septal defect, patent ductus arteriosus with severe pulmonary hypertension and blood flow from the pulmonary trunk to the aorta.
III. Defects with hypovolemia of the pulmonary circulation : 1) not accompanied by cyanosis - isolated stenosis of the pulmonary trunk; 2) accompanied by cyanosis - triad, tetralogy and pentade of Fallot, tricuspid atresia with narrowing of the pulmonary trunk or small ventricular septal defect, Ebstein's anomaly (displacement of the tricuspid valve leaflets to the right ventricle), hypoplasia of the right ventricle.
IV. Combined defects with disruption of the relationship between various parts of the heart and large vessels: transposition of the aorta and pulmonary trunk (complete and corrected), their origin from one of the ventricles, Taussig-Bing syndrome, common truncus arteriosus, three-chambered heart with a single ventricle, etc.
Symptoms of aortic insufficiency
The rate at which symptoms develop depends on the cause of aortic insufficiency.
Acute form
Acute aortic insufficiency develops abruptly, literally in a few minutes to hours, less often during the day. The cause is often some acute pathology, such as valve injury or aortic dissection. As a result, severe aortic insufficiency develops with large backflow of blood into the left ventricle. It's overflowing with volume. Mitral valve insufficiency develops quickly and blood stagnates in the pulmonary circulation, which can lead to pulmonary edema. If emergency measures are taken, the heart can recover almost completely.
In the acute form, acute heart failure with pulmonary edema and cardiogenic shock develops:
- severe shortness of breath,
- difficulty breathing,
- cough,
- forced position of the patient sitting,
- wheezing in the lungs,
- the appearance of foamy pink sputum,
- decreased blood pressure until loss of consciousness.
Even with intensive drug therapy, death often occurs from ventricular arrhythmias, cardiogenic shock, and pulmonary edema.
Chronic form
Chronic develops slowly. The clinic has not developed for years. A person may not be aware of the pathology and deficiency often becomes an accidental finding. Or the patient comes in with some symptoms, when the heart is greatly changed. Treatment in this case is mainly symptomatic, although in some cases surgical correction is possible.
Chronic aortic insufficiency can be asymptomatic for years. The first symptoms may be lethargy, decreased performance, fainting and presyncope. The clinical picture of heart failure is gradually developing due to volume overload of the left ventricle:
- shortness of breath during exercise, then over time at rest;
- attacks of suffocation;
- pain in the heart area of a pressing, squeezing nature, which goes away after taking nitroglycerin;
- swelling of the lower extremities, and subsequently, in the absence of adequate treatment, fluid appears in the abdominal, pleural and even pericardial cavities;
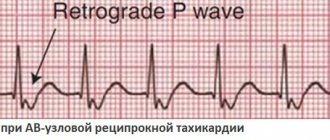
- heart rhythm disturbances - from atrial fibrillation to ventricular tachycardia. life-threatening.
Aortic valve defects in adults: modern pathology and indications for surgery
S.L. Dzemeshkevich
Dr. honey. Sciences, Professor, Cardiac Surgeon, Department of Cardiovascular Surgery, RKNPK
In developed countries, calcified aortic disease is the third most common nosological form after arterial hypertension and coronary heart disease [1].
Knowledge of the etiology of the process that led to aortic disease can significantly influence both surgical tactics and the postoperative treatment protocol for patients and, ultimately, the long-term prognosis. Therefore, at all stages of treatment, one should strive to answer the question of the etiology of the primary process that caused valve dysfunction. Sometimes this answer can only be given by a surgeon who visually assesses the nature of the valve damage already during surgery. In any case, elucidation of the etiology, even with a presumptive conclusion, is extremely important.
Etiology
Assessing our own experience and published data from colleagues from other Russian clinics, it is necessary to emphasize that even today aortic malformations of rheumatic etiology dominate in cardiac surgery hospitals, although not as clearly as in the statistics half a century ago. This figure does not exceed 30-40%. However, if we take into account that only during the period from 1993 to 1998 in Russia the frequency of the cardiac form of rheumatism increased 7 times [2], then in the future we should again expect an increase in the number of patients with rheumatic valve defects.
The increase in surgical interventions on the aortic valve in the group of patients over 60 years of age has significantly increased the number of atherosclerotic “degenerative” (age-related) aortic valve defects. If aortic disease is moderately expressed and combined with widespread atherosclerosis of the coronary arteries, aorta and its branches in combination with distinct specific disorders in lipid metabolism (total cholesterol, low-density lipoproteins, triglycerides), then the atherosclerotic origin of the process on the valve is beyond doubt. This is a special and prognostically most severe group of patients. It is to this category of patients that the point of view of some authors extends that aortic stenosis is a special form of manifestation of atherosclerosis with risk factors identical to this systemic disease.
In a real clinical situation, no more than 50% of elderly patients with signs of aortic stenosis have changes in the coronary vessels [3-5]. Such patients have another degenerative process in the valve with a reduced level of metabolic reactions due to age-related changes: atherosclerosis as such can only play the role of an accelerating factor, especially if it is accompanied by inflammatory changes in the aortic valve leaflets, specific to many atheromas, due to the invasion of Chlamydia pneumoniae [6, 7 ]. Age-related involutional calcium degeneration is, in our opinion, the most appropriate definition for this pathology of the aortic valve. As a special form, it is often found in elderly patients and, as a rule, when analyzed, falls into the group of atherosclerotic defects. The diagnostic line between these two groups of patients (atherosclerosis and age-related dystrophy) is very thin, but it is quite possible to draw it with a certain amount of experience. The practical significance of such a diagnosis can be expressed not only in a different prognosis, but also in the amount of drug therapy after surgery (use of antiplatelet agents, lipid-lowering drugs).
The same type of “degenerative” defects with severe calcification includes a group of patients with a congenital bicuspid aortic valve configuration. This was unexpected for us, but the number of such patients increases as the number of elderly patients operated on increases.
Actually, the three main causes of aortic heart defects that we have already noted together account for at least 90% of the causes of aortic valve stenosis [5, 8-13]. All these reasons lead to different pathomorphological, but similar functional changes in the aortic valve leaflets, limiting their mobility. This process (fibrosis, thickening, formation of adhesions in the commissure area, calcification) always takes a long time - years, or even decades. Other, more rare causes of aortic stenosis include previous and active infective endocarditis, systemic lupus erythematosus (verrucous aseptic endocarditis of Libman-Sachs), hereditary metabolic disorders such as homozygous hyperlipoproteinemia type II and alkaptonuria (ochronosis), metastatic calcification of the aortic valve in patients with chronic renal failure [14-16].
Pure or dominant aortic insufficiency is much less common than stenosis. With combined lesions, the most common cause is rheumatic valvulitis, which leads to wrinkling and shortening of the aortic valve leaflets. Infectious endocarditis plays a significant role, forming aortic insufficiency either on the native valve or by altering the natural history of such anomalies as a bicuspid or prolapsed aortic valve. And yet, despite the fact that rheumatism is the most common cause of aortic insufficiency and in this nosology is not an absolutely dominant process, other causes of aortic insufficiency in the aggregate are much more diverse than with aortic stenosis. All this diversity can be divided into three pathomorphological groups:
• aortic insufficiency with changes only in the semilunar cusps (rheumatism, infective endocarditis, bicuspid valve, cusp prolapse);
• aortic insufficiency as a result of pathology of the ascending aorta with anatomically unchanged leaflets (Marfan syndrome, Ehlers-Danlos syndrome, syphilitic aortitis, ankylosing spondylitis, dissecting aneurysm of the ascending aorta);
• aortic insufficiency with anatomically preserved aorta and aortic cusps (secondary prolapse with a ventricular septal defect, hypertension).
Indications for surgery
The symptom complexes characteristic of a particular valve defect determine modern treatment tactics to a much greater extent than the actual nature of the damage to the aortic valves. Therefore, any attempt to identify a diagnosis of the condition, justify indications for surgical intervention and surgical tactics only on topical diagnostic data (orifice diameter, the amount of valve prolapse, the amount of pressure drop across the valve, the presence or absence of signs of calcification, etc.) does not indicate the benefit of a comprehensive clinical analysis of the condition of a particular patient.
Cardiologists today reliably diagnose this pathology and promptly send such patients to cardiac surgeons. And yet, when deciding on surgery in patients over 70 years of age, we sometimes encounter some resistance from our fellow cardiologists. Their doubts are based on both an objective factor - the higher risk of surgery, and a subjective one - the unknown of the individually “programmed” life expectancy of such elderly patients.
Therefore, in this publication we specifically report data from O'Keefe et al., [17] who were able to follow a group of 50 patients awaiting balloon dilatation of a stenotic aortic valve. The average age of patients exceeded 70 years, survival without surgery by the 3rd year of observation was only 25%. At the same time, in the randomized group of patients without aortic pathology, the survival rate was 77%. Considering that today mortality in aortic replacement is minimal, then these data should convincingly prove to cardiologists the need for surgical treatment of such patients.
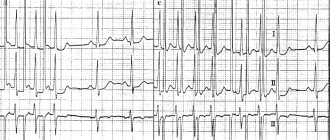
In classic situations, the question “when to operate?” does not present any difficulties: digital radiography from the screen of an electron-optical converter, ECG, echocardiography, MRI with contrast are sufficient methods for making a topical diagnosis and assessing the condition of the left ventricle of the heart. Performing sounding of the heart cavities in patients with aortic defects in order to determine the pressure drop, the volume of regurgitation, end-diastolic pressure in the left ventricle or pulmonary capillary wedge pressure today can already be regarded as a diagnostic anachronism.
In our practice, we are naturally especially wary of choosing a solution in patients with “minor” symptoms and, even more so, in asymptomatic patients. It is known that clinical manifestations and complaints may be absent even with severe severe aortic stenosis with an orifice area of less than 0.8 cm3 and with a decrease in the ejection fraction to 25-30% [18].
Enlargement of the left ventricle of the heart to 6 cm or more (in patients with aortic insufficiency), as well as hypertrophy with overload of the left ventricle (in patients with aortic stenosis), are sufficient instrumental criteria for the need for surgery in the presence of a topical diagnosis.
Doppler echocardiography makes it possible to determine the magnitude of the pressure drop with almost the same accuracy as probing of the left ventricle. Understanding the conventions and multifactorial dependence of this indicator, we consider its value to be 40-50 mm Hg. Art. sufficient grounds for a more detailed examination of the patient and search for arguments in favor of surgery.
Calculation of the size of the effective opening is less dependent on the characteristics of blood flow through the section “left ventricle-aortic valve-ascending aorta”, but this indicator is quite conditional and “semi-quantitative”. And yet, we definitely take into account the instructions of ultrasound diagnostic specialists to limit the opening of the valve leaflets to less than 1.5 cm, and when the opening size is less than 1 cm, the indications for surgery are almost absolute. An even more accurate expression of the degree of stenosis is the ratio of the size of the stenosis to the total body surface area - a value of less than 0.6 cm/m2 is critical [19]. If there is information about valve calcification, then you should not postpone the operation, since progression of the process is inevitable.
If the arguments in favor of the operation are not absolute, then for aortic stenosis we calculate the pressure loss across the valve (mm Hg/ml stroke volume) - the value is 1 mm Hg. Art./ml and more significant and weighty. If necessary, repeat these calculations under load. In aortic insufficiency, a decrease in the ejection fraction of less than 55% and its further decrease (or unchanged) under stress test conditions also indicate the limit of compensatory reserves of the left ventricular myocardium and serve as a more than convincing criterion in favor of surgery.
In the presence of concomitant coronary pathology requiring surgical correction, or concomitant mitral valve defects, the criteria for revision and intervention on the aortic valve can be much more liberal and are often determined by the individual decision of the operating surgeon.
It should be remembered that aortic stenosis progresses regardless of any patterns. However, with degenerative defects this process occurs faster than with rheumatic defects or in the presence of a bicuspid valve. With slow progression, the opening of the aortic valve narrows by 0.02 cm2 per year, and with rapid progression - more than 0.3 cm2 per year. When the peak velocity of blood flow through the valve reaches about 4 m/s, the two-year survival rate without surgery is only 21%. Thus, calcification, the rapid progression of stenosis over the course of a year and positive stress tests (a slight increase or even a decrease in blood pressure during exercise) are real factors for deciding on surgery for asymptomatic aortic stenosis.
In asymptomatic aortic insufficiency, the prognosis is based on assessment of left ventricular function and the degree of dilatation of the ascending aorta. Threatening signs are an increase in end-diastolic pressure of the left ventricle more than 70 mm, end-systolic pressure more than 50 mm (index more than 25 mm/m2 of the patient’s body surface), a decrease in the ejection fraction to 50%. If the ascending aorta is dilated more than 55 mm, surgery should be offered regardless of the degree of aortic regurgitation and left ventricular function. In patients with a bicuspid valve or Marfan syndrome, the indications for surgery are even more stringent - the threshold for making a decision is the diameter of the ascending aorta is 50 mm.
Continuous planned monitoring of the condition is necessary for all patients with symptoms of aortic disease and is mandatory every 12 months so as not to miss the time for possible surgical interventions.
Bibliography
1. Jund B. et al. //Eur. Heart J. 2002. V. 23. P. 1253.
2. Diseases of the heart and blood vessels // Pathological anatomy / Ed. Paltse-va M.A., Anichkova N.M. T. 2.Ch. 1. Ch. 11. M., 2001. P. 8.
3. Lindroos M. et al. //J. Amer. Coll. Cardiol. 1993. V. 21. P. 1220.
4. Iivanainen AM et al. // Amer. J. Cardiol. 1996. V. 78. P. 97.
5. Stewart BF et al. //J. Amer. Coll. Cardiol. 1997. V. 29. P. 630.
6. Nystrom-Rosander C et al. // Scand. J. Infect. Dis. 1997. V. 29. P. 361.
7. Juvonen J. et al. // J. Amer. Coll. Cardiol. 1997. V. 29. P. 1054.
8. Passik CS et al. // Mayo Clin. Proc. 1987. V. 62. P. 119.
9. Davies MI Butterworths. L., 1980.
10. Subramanian R. et al. // Mayo Clin. Proc. 1984. V. 59. P. 683.
11. Subramanian R. et al. // Mayo Clin. Proc. 1985. V. 60. P. 247.
12. Peterson MD et al. //Arch. Pathol. Lab. Med. 1985. V. 109. P. 829.
13. David TE//J. Heart Valve Dis. 1999. V. 8. P. 495.
14. Roberts WC et al. // Amer. J. Cardiol. 1973. V. 31. P. 557.
15. Roberts WC et al. // Circulation. 1967. V. 36. P. 449.
16. Pritzker MR et al. //Ann. Intern. Med. 1980. V. 93. P. 434.
17. O'Keefe JH et al. // Mayo Clin. Proc. 1987. V. 62. P. 986.
18. Corabello B. // J. Heart Valve Dis. 1995. V. 4. Suppl. 11. P. 132.
19. Rahimtoola SH //J. Amer. Coll. Cardiol. 1989. V. 14. P. 1.
The article was published in Atmosfera magazine. Cardiology
Surveys
Examination of a patient always begins with examining and listening to the heart. Already at this stage, the doctor is able to suspect a valve defect by the presence of a heart murmur. It is also possible to decrease diastolic (lower limit) blood pressure and, as a result, increase pulse pressure (the difference between the upper and lower limits of blood pressure). However, such signs of aortic insufficiency are detected only in chronic pathology, when the clinical picture of heart failure described above is already clearly manifested.
Instrumental methods are the only way to detect regurgitation on the aortic valve.
Echocardiography (ultrasound of the heart)
First line diagnostic method. It detects backflow of blood through the aortic valve. The doctor determines the degree of its severity and the possible cause - for example, trauma, vegetations on the valve (accumulations of bacteria on the valves - a sign of infective endocarditis), volumes of the left chambers of the heart, left ventricular ejection fraction and many other morpho-functional indicators.
Magnetic resonance imaging (MRI)
Used only if echocardiography is not available or visualization of the heart and its structures is extremely difficult.
Multislice computed tomography angiography and magnetic resonance imaging angiography (both contrast-enhanced procedures) are used in patients with a bicuspid aortic valve to evaluate the initial aorta to its arch, but only if echocardiographic findings are unsatisfactory.
X-ray of the chest organs
Used to assess the size of the heart and ascending aorta.
Electrocardiogram (ECG)
Allows you to identify rhythm disturbances, conduction disorders in the heart and signs of myocardial hypertrophy.
The methods listed are more than enough to make an accurate diagnosis of aortic insufficiency and begin treatment on time.
Clinic for bicuspid aortic valve and treatment methods
Bicuspid aortic valve is the most common heart defect formed in utero. Pathology is diagnosed in 20 out of 100 people who consult a cardiologist. In healthy people, the valve has three leaflets. They open and close at a certain moment. The valves allow blood to move in one direction. The bicuspid valve develops before birth in the womb. Considered a deviation from the norm. Over a long period of time it may not manifest itself in any way.
Bicuspid aortic valve is a pathology that develops in utero
Root causes
Aortic defect “bicuspid aortic valve” occurs against the background of:
- a pregnant woman suffering from one or another infectious pathology;
- exposure to radiation;
- frequent stressful situations in a pregnant woman;
- smoking and drinking alcohol-containing drinks by a girl while carrying a child;
- genetic predisposition;
- the presence of any serious hereditary disease in one of the parents.
A 2-leaf aortic valve is a pathology that develops in utero. As a rule, this occurs at 5-9 weeks of pregnancy. This period is considered the most critical. When negative factors interact with the body of a woman carrying a child, the risk of abnormalities in the functioning of the heart and vascular system of the fetus increases.
Heart disease can be a consequence of a pregnant woman suffering from influenza and rubella.
Most often, the formation of two valves is associated with a hereditary predisposition. There is a high risk of a child developing a disorder if one of his parents has encountered a disorder.
Women who have had viral diseases during pregnancy are at risk of giving birth to a baby with a bicuspid valve.
Symptoms of pathology
Congenital heart disease “Bivalve aortic valve” can occur for a long time without obvious signs. Patients often find out about the presence of a disorder at an older age.
Usually, up to 10-20 years, the valve functions as expected and does not provoke the occurrence of any negative signs. Symptoms appear gradually. The patient begins to worry:
- My Heart Valve Replacement Story
- a feeling of pulsation in the head (its intensity may vary);
- feeling of strong heartbeat;
- sinus tachycardia;
- fainting and periodic loss of consciousness;
- regular and obvious dizziness;
- disturbance in the functioning of the visual organs;
- difficulty breathing even with the most minor physical exertion;
- pain syndrome in the chest.
Fatigue and fainting may be signs of heart disease
With pathology, the patient's blood flow is significantly impaired. Symptoms can vary in intensity. The bicuspid aortic valve in children does not cause discomfort for a long time. Gradually, intolerance to any type of physical stress may appear. From time to time, a small patient may complain of aching headaches.
A bicuspid aortic valve in a child provokes memory impairment.
In infancy, pathology can manifest itself as a weak sucking reflex, excessive tearfulness and lethargy. The baby is not gaining weight well and is constantly spitting up.
If left untreated, the pathology becomes chronic. The deviation is characterized by the following symptoms:
- heart rhythm disturbances;
- constant presence of difficulty breathing;
- night cough;
- swelling.
Coughing is one of the signs of chronic disease
Patients are at high risk of developing additional pathologies. When they appear, all symptoms become more pronounced.
Diagnostic measures
CHD - bicuspid aortic valve can be diagnosed using:
- Ultrasound;
- standard ECG and daily monitoring;
- radiographs of the lungs.
First of all, the cardiologist questions the patient and identifies complaints. The doctor determines the possible root causes of the development of the disorder.
Particular attention to the initial examination. Children with heart defects are significantly behind their peers in physical development. When diagnosing a disorder in an infant, a doctor may notice bluish skin, muscle hypotonicity, and slow weight gain.
- Why is aortic valve stenosis dangerous?
If a bicuspid valve is suspected, an ECG of the heart is mandatory.
Laboratory tests are necessary to determine the general condition and identify associated abnormalities.
The main diagnostic method is ultrasound. This is the only way to confirm the presence of a bicuspid aortic valve. Other studies are required to clarify the extent of damage and select therapeutic measures.
Features of therapy and life activity
Bicuspid aortic valve does not always require treatment. Therapy is selected on an individual basis, so the patient needs to be diagnosed annually for prevention.
Surgery is considered difficult, so it is performed only if there are negative symptoms
Treatment is not necessary if the patient does not have negative symptoms. The condition is normal. At an advanced stage of deviation, surgical intervention is prescribed - installation of a prosthesis. After the procedure, you will need to take medications. The types of implants are described in the table.
>Type of prosthesis Description Biological Made from tissues of animal origin. Mechanical Made from metal compounds.
The operation is considered difficult. Can lead to:
- severe disruption of blood flow;
- destruction of biological processes;
- arterial thromboembolism.
The patient must take medications in courses. The cardiologist prescribes:
A bicuspid aortic valve cannot be treated on its own. Medicines should only be prescribed by a doctor.
Proper nutrition, frequent walks and giving up bad habits are the main recommendations when pathology is detected.
- Flat feet with arthrosis - symptoms and treatment
If the heart valve has 2 leaflets, the patient must completely change his lifestyle. You should give preference to a balanced diet. Special formulas are recommended for infants. Regular walks outside are required.
The patient is recommended to sign up for swimming. Therapeutic exercises are indicated daily. Physical activity should be moderate. The patient may be referred for dissection of the bicuspid aortic valve.
The patient should not deny himself sports. However, its type is selected on an individual basis. Maximum loads are contraindicated. People with a bicuspid aortic valve are most often not accepted into the army.
The doctor can make a decision about surgery only after a thorough examination.
Prognosis and life expectancy
The prognosis for the future with bicuspid aortic valve in children is individual. In the absence of a clinical picture of deviation and deterioration of the condition, the pathology may not cause any discomfort. The patient will live a normal life.
After surgery, people live 12-17 years. This directly depends on the way of life and the individual characteristics of the body. If all doctor's instructions are followed, life expectancy will be long.
In other words, the prognosis for life with a bicuspid aortic valve is often favorable. The main thing is moderate physical activity and regular diagnostic testing.
Most patients with bicuspid valve lead normal lives.
Prevention of deviation
Preventative measures are necessary to maintain good health and reduce the risk of complications. These include:
- maintaining a correct lifestyle;
- eating healthy foods with plenty of essential vitamins;
- outdoor sports;
- regular walks outside;
- alternating physical activity with mental activity.
The patient should avoid stress. You should absolutely not overwork yourself. It is important that the load alternates with rest. You need to give up bad habits. The diet should include as many fruits and vegetables as possible. The 2-leaf aortic valve is not dangerous and if the doctor’s recommendations are followed, the patient will not experience any discomfort.
The video talks about the role of the aortic valve and what happens if its operation malfunctions:
Treatment
Aortic insufficiency is treated by a cardiologist and cardiovascular surgeon.
Drug treatment
Drug treatment is prescribed depending on the cause of aortic insufficiency. It is considered as an option in preparation for surgery or to reduce the symptoms of heart failure and alleviate the condition of patients who have contraindications to surgical treatment.
For rheumatism and infective endocarditis, a course of antibacterial therapy is prescribed. In the first case, penicillin antibiotics (benzathine benzylpenicillin) are used to prevent exacerbation of the disease. For infective endocarditis, amoxicillin, ceftriaxone, gentamicin, and, less commonly, vancomycin are usually prescribed for a long course of 2 weeks. Drugs are prescribed based on the clinic and the resistance of bacteria to them. Can be used as a single drug or in combination.
Treatment of arterial hypertension consists of prescribing ACE inhibitors (perindopril, enalapril, lisinopril) or sartans (valsartan, losartan) and dihydropyridine calcium antagonists (nifedipine, amlodipine).
Beta blockers (bisoprolol, metoprolol, nebivolol) are added to treatment in the case of reduced cardiac ejection fraction as determined by echocardiography.
Surgery
Aortic valve replacement is the only possible method of valve correction.
It is recommended for patients with:
- severe aortic regurgitation and the presence of symptoms regardless of ejection fraction;
- asymptomatic chronic severe aortic regurgitation and ejection fraction less than 50%;
- chronic aortic regurgitation in parallel with coronary artery bypass surgery or surgery on the aorta and other heart valves;
- asymptomatic severe aortic regurgitation with normal ejection fraction. on significant expansion of the left ventricle (EDV - more than 75 mm).
The duration of treatment for patients with aortic insufficiency varies greatly depending on the severity of the condition and the cause of the pathology. After the operation, it is recommended to undergo a course of rehabilitation in a cardiological sanatorium or rehabilitation center. The recovery period is at least 3 months, after which the patient can resume work with the doctor’s permission.
Complications
Complications of aortic insufficiency develop as its severity increases. At the beginning, normal syncope (fainting) may appear due to insufficient blood supply to the brain. Conduction disorders in the form of blocks of the left bundle branch and atrioventricular conduction of impulses can also often occur in patients with aortic insufficiency.
Coronary insufficiency can accompany aortic insufficiency, but more often in combination with aortic valve stenosis. The patient develops attacks of angina (pain in the heart of a pressing, squeezing nature) and even myocardial infarction.
Heart failure is the most common complication of already severe aortic regurgitation. The patient complains of shortness of breath during physical exertion, asthma attacks, and swelling of the lower extremities.
Sudden death often develops as a result of life-threatening arrhythmias - paroxysmal ventricular tachycardia, ventricular fibrillation. In this case, the person does not even have time to call an ambulance - the arrhythmia develops so quickly.
Congenital anomalies [malformations] of the aortic and mitral valves (Q23)
Aortic valve congenital:
- atresia
- stenosis
Excluded:
- congenital subaortic stenosis (Q24.4)
- stenosis in left-sided hypoplastic heart syndrome (Q23.4)
Bicuspid aortic valve
Congenital aortic insufficiency
Congenital mitral atresia
Atresia or severe hypoplasia of the aortic ostium or valve with hypoplasia of the ascending aorta and a defect in the development of the left ventricle (with stenosis or atresia of the mitral valve).
ICD-10 alphabetical indexes
External Causes of Injury - The terms in this section are not medical diagnoses, but rather a description of the circumstances under which the event occurred (Class XX. External Causes of Morbidity and Mortality. Heading Codes V01-Y98).
Medicines and chemicals - table of medicines and chemicals that have caused poisoning or other adverse reactions.
In Russia, the International Classification of Diseases
10th revision (
ICD-10
) was adopted as a single normative document for recording morbidity, reasons for the population’s visits to medical institutions of all departments, and causes of death.
ICD-10
introduced into healthcare practice throughout the Russian Federation in 1999 by order of the Russian Ministry of Health dated May 27, 1997 No. 170
The release of the new revision (ICD-11) is planned by WHO in 2022.
Abbreviations and symbols in the International Classification of Diseases, 10th Revision
NOS
- without further clarification.
NEC
— not classified in other categories.
†
— code of the main disease. The main code in the dual coding system contains information about the underlying generalized disease.
*
- optional code. An additional code in the double coding system contains information about the manifestation of the main generalized disease in a separate organ or area of the body.
Source
Forecast
The prognosis for aortic insufficiency is better, the lower the degree of regurgitation and the earlier treatment is started. Preventive examination by a general practitioner, cardiologist, full antibiotic therapy in case of infective endocarditis and rheumatic fever - all this helps to improve the prognosis. It is very important to listen to yourself, your body, so as not to miss the first symptoms (lethargy, decreased performance, fainting, shortness of breath during physical activity).
Usually, with severe clinical heart failure, the prognosis worsens, since irreversible changes occur in the structure of the heart.
Differential diagnosis
Differential diagnosis and rationale for additional studies
Additional laboratory tests:
- Tests for hepatitis B, C, HIV, microreaction (to exclude infectious pathology).
Additional instrumental studies:
- Daily ECG monitoring (Holter monitoring) Standard Holter ECG monitoring has diagnostic meaning only in the presence of symptoms, probably associated with the presence of arrhythmias (subjective sensations of interruptions, accompanied by dizziness, fainting, history of syncope, etc.).
- Multislice CT angiography/MRI is an additional noninvasive imaging modality if echocardiography results are inconclusive. Direct visualization of the defect and pulmonary veins is possible, RV volume and function can be measured, and shunt volume can be assessed.
- An exercise test may be useful to determine a patient's exercise capacity when symptoms are inconsistent with clinical findings and to document changes in oxygen saturation in patients with pulmonary arterial hypertension.
- Coronary angiography is used to identify coronary anomalies or arterial obstruction, and men 35 years of age and older, premenopausal women 35 years of age and older with risk factors for atherosclerosis, and postmenopausal women should undergo cardiac catheterization and coronary angiography to detect CAD before cardiac surgery.
| Diagnosis | Rationale for differential diagnosis | Surveys | Diagnosis exclusion criteria |
| BEAM | High pulmonary hypertension | angicardiography | |
| Coronary pulmonary fistulas | angicardiography | ||
| Rupture of sinus of Valsalva | ECHOCG |