Many people have heard about the features and terrible consequences of myocardial infarction, including death, and most of us have had relatives or friends suffer from this disease. Speaking about the attack itself, the mind immediately associates with its main symptoms: pain in the chest (stabbing, burning, aching, cutting nature), which radiates to the shoulder or under the shoulder blade, shortness of breath, rapid heartbeat, dizziness, profuse sweating, loss of consciousness.
But as it turned out, doctors repeatedly record cases where these characteristic symptoms do not appear and a person, without realizing it, suffers a heart attack on his legs.
This phenomenon is also called an atypical form of the disease. As a rule, it is revealed that the patient suffered a heart attack on his legs - randomly, for example, in a cardiogram during an annual medical examination.
Sign up for a consultation
Mechanism of development of acute coronary syndrome
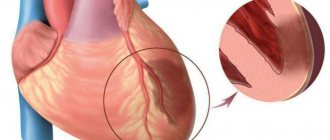
Myocardial infarction, which, along with an episode of unstable angina, is included in the concept of acute coronary syndrome, is an exacerbation of coronary heart disease. During myocardial infarction, necrosis of the heart muscle develops due to acute disruption of the blood supply. In most cases, this occurs as a result of atherothrombosis, in which the coronary vessels are partially or completely blocked by a blood clot. The disease is manifested by sudden intense pain in the chest, tachycardia, “cold sweat”, pallor of the skin and a number of other symptoms.
The goal of treating an acute heart attack is to quickly restore blood supply. However, even after blood flow is established, therapy cannot be stopped, since coronary atherosclerosis, which became the foundation for the development of acute coronary syndrome, is chronic.
How to identify?
Reliable detection of a previous heart attack with minimal clinical manifestations is possible using objective diagnostic techniques, which include:
- ECG - cardiogram is a functional research method that makes it possible to determine the nature and location of ischemia (insufficient tissue nutrition) or myocardial infarction.
- “Holter” monitoring is the recording of a cardiogram using a portable device for a long period of time (usually about a day), during which the patient leads a normal lifestyle.
- Echocardioscopy is an ultrasound examination of the heart, which makes it possible to visualize affected tissue. It will show the severity of the pathological process, as well as its localization.
- Biochemical blood test - determination of the activity of certain enzymes in the plasma, which increases with the death of a large number of myocardial cells (myocardiocytes).
- A clinical blood test is the determination of a number of indicators that make it possible to assess the functional state of many organs and systems, as well as to identify the inflammatory process that often develops against the background of a heart attack.
If necessary, the doctor prescribes other research methods that help establish or exclude the presence of complications, as well as other concomitant pathologies.
Timely diagnosis of a heart attack suffered “on your feet” is an important measure that helps prevent the development of complications and negative health consequences.
Early consequences of myocardial infarction1
Starting from the first hours after a heart attack and up to 3-4 days, early consequences of a heart attack may develop, including:
- acute left ventricular failure, which occurs when the contractility of the heart decreases. When it occurs, shortness of breath, tachycardia, and cough appear;
- cardiogenic shock. This is a severe complication of acute coronary syndrome, developing as a result of a significant deterioration in the contractility of the heart muscle due to extensive necrosis;
- disturbances of cardiac rhythm and conduction are observed in 90% of patients with acute MI.
- Attacks of early post-infarction angina (PSA). PSC is the occurrence or increase in frequency of angina attacks 24 hours and up to 8 weeks after the development of MI.
- pericarditis is an inflammatory process that develops in the outer lining of the heart, the pericardium. It occurs in the first or third day of the disease and can manifest itself as pain in the heart area, which changes with a change in body position, and an increase in body temperature.
In 15-20% of heart attack cases, thinning and bulging of the heart wall occurs, most often of the left ventricle. This condition is called cardiac aneurysm. As a rule, it develops with extensive damage to the heart muscle. Factors predisposing to the development of cardiac aneurysm also include violation of the regime from the first days of the disease, concomitant arterial hypertension and some others.
A special group consists of thromboembolic consequences, in which the lumen of the vessels is completely or partially blocked by blood clots. This often occurs against the background of concomitant varicose veins, blood coagulation disorders and prolonged bed rest.
Due to impaired blood supply, acute coronary syndrome can be complicated by gastrointestinal problems, such as erosions and acute ulcers of the gastrointestinal tract. Mental disorders may also occur - depression, psychosis. They are facilitated by old age and concomitant diseases of the nervous system.
Types and symptoms of their manifestation
There are six types of atypical forms of the disease:
- arrhythmic;
- asthmatic;
- abdominal;
- collaptoid;
- erased;
- cerebral.
Each of these varieties manifests itself differently, and the symptoms of the attack often do not even resemble such a serious disease, which results in a heart attack on the legs.
In the event of an arrhythmic attack, a disturbance in the rhythm of the heartbeat occurs, and cases of cardiac arrest are common.
The asthmatic form is manifested by a strong attack of coughing, reaching the point of suffocation, and no pain in the cardiac region (or radiating under the shoulder blade) is observed.
An abdominal attack is characterized by sharp pain in the abdomen, which intensifies with slight pressure on the pancreas. Very often the attack is accompanied by bloating, as well as nausea and vomiting.
A collaptoid attack is characterized by a sharp decrease in blood pressure, accompanied by dizziness and often fainting.
The most asymptomatic type is the erased type (the most common case of a heart attack on the legs). In this case, there is only mild weakness or sweating, and less often – discomfort in the chest (in the form of mild pain of an undetermined nature).
call me back
The cerebral variety is distinguished by symptoms characteristic of cerebrovascular accident: speech becomes slurred, nausea and vomiting appear, some clouding of consciousness appears, and weakness in the limbs.
Considering the obvious insidiousness of the disease, it should be treated with great caution, avoiding the consequences that a heart attack on the legs may bring; any symptoms - characteristic or uncharacteristic (characteristic of the atypical form) - should be a signal to consult a doctor.
Important! Every 5th of those who suffered a heart attack does not know about it, and in every 4th patient this disease is not recognized.
Late consequences of a heart attack
At the end of the acute period of the disease, so-called late consequences may develop. These include complications that appear 10 days after the manifestation of MI and later:
- post-infarction Dressler syndrome occurs 2-6 weeks after the manifestation of myocardial infarction and is manifested by inflammation of the pericardium, pleura, alveoli, joints and other pathological changes;
- thromboendocarditis with thromboembolic syndrome (the appearance of a wall thrombus in the heart cavity, on the heart valves);
- late post-infarction angina, which is characterized by the occurrence or increase in frequency of angina attacks. Its frequency ranges from 20 to 60%.
Some patients who have suffered an acute myocardial infarction are at high risk for developing repeated complications of coronary heart disease and, above all, recurrent myocardial infarction and unstable angina. This is due to the fact that in patients with acute coronary syndrome, along with the presence of an atherosclerotic plaque, which was complicated by a rupture and blocked the lumen of the coronary artery, there are plaques in other arteries. They can be the cause of repeated episodes of cardiovascular events, the probability of which is very high.
Tatyana Raush: “Myocardial infarction is dangerous due to its diversity and suddenness”
Heart and vascular diseases remain the leading cause of death and disability worldwide. According to the World Health Organization, cardiovascular diseases (CVDs) cause nearly 17 million deaths per year. In Russia, over the past ten years, mortality and disability indicators have exceeded the corresponding indicators of economically developed countries by 4-5 or more times and amount to 56 percent of the total number of deaths. In Komi, the prevalence of CVD among the adult population has increased by 17 percent in recent years. How to influence these bleak statistics and what doctors themselves think about this, Tatyana Raush, head of the emergency cardiology department of the cardiology clinic, told Respublika in an interview.
– What is myocardial infarction?
– Myocardial infarction (MI) is a lesion of the heart muscle caused by an acute disruption of its blood supply due to blockage (thrombosis) of one of the arteries of the heart by an atherosclerotic plaque. In this case, the affected part of the muscle dies, that is, its necrosis develops. Cell death begins within 20-40 minutes from the moment blood flow in the vessel stops.
-What happens to the heart?
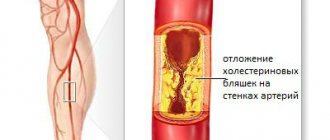
– The heart is a muscular organ whose main function is to “pump” blood throughout the body. The heart muscle (myocardium) is constantly subjected to very serious stress (on average, at rest, the heart “pumps” five liters of blood per minute, and under intense stress - 15 liters or more). In order to effectively perform such work, the myocardium must be very well supplied with nutrients and oxygen. In the wall of the vessels that supply blood to the heart (coronary arteries), over time, cholesterol-containing thickenings, called atherosclerotic plaques, appear from the inside. Plaques gradually grow and cause a narrowing of the artery (stenosis), which naturally reduces blood flow to the heart. This process is commonly called atherosclerosis. Currently, there are two main reasons for the development of atherosclerosis: a violation of cholesterol metabolism and damage to the inner lining of the vessel, where this cholesterol is deposited. More often this is a gradual process: the heart muscle adapts to it for quite a long time, a person can feel normal for a long time, unaware of what is happening in his blood vessels. But as the process progresses, a person begins to show signs of the disease - paroxysmal pain, which is often localized in the chest, can be burning, squeezing, may be accompanied by a feeling of lack of air, and usually occurs during physical and emotional stress. This is a signal that the heart muscle (myocardium) in the area of vessel narrowing is experiencing a lack of blood supply (ischemia). In this case, it is customary to talk about coronary heart disease. Coronary heart disease can suddenly manifest itself as a heart attack, which is based on the formation of a blood clot - a thrombus. A thrombus forms at the site of damage to an atherosclerotic plaque, to which platelets from the blood flowing through the vessel begin to “stick.” A thrombus causes blockage of a vessel. In this case, blood flow to the corresponding part of the heart suddenly and abruptly stops. If the supply of blood to a section of the heart muscle is stopped for a sufficiently long time, its death develops - a heart attack.
– When should you start sounding the alarm?
– One of the main symptoms of myocardial infarction is chest pain. Intense (sometimes unbearably strong) pressing, squeezing or burning pain behind the sternum is typical. Pain can also be felt on the left of the sternum, rarely on the right. The pain can radiate to the jaw, throat, back under the left shoulder blade or between the shoulder blades, to the upper abdomen. The pain is usually not localized, but widespread. They can occur in waves, sometimes growing, sometimes weakening, stopping and then resuming again. The duration of pain can be from 20 minutes to several hours. There may be accompanying symptoms such as severe weakness, cold sticky sweat, trembling, a feeling of shortness of breath, difficulty breathing, cough, dizziness, fainting. A person may experience emotional agitation, and behavioral disturbances may also occur, including the development of psychosis. Also, a heart attack or pre-infarction condition may be accompanied by nausea, vomiting, and bloating. All of the listed symptoms can occur in various combinations with each other; it is not necessary that all the described signs will be present. There may also be no chest pain (the absence of pain syndrome occurs in 20-30 percent of cases of myocardial infarction). There may be few symptoms, they may not be too pronounced. Myocardial infarction is often asymptomatic in people with diabetes and in elderly patients. Quite often, the symptoms of myocardial infarction are atypical, for example, stabbing pain in the chest. The condition can imitate an exacerbation of osteochondrosis, gastric ulcer, etc. I repeat, if you have sensations that are unfamiliar to you before and it seems to you, for example, that it is radiculitis, which was not there before, call an ambulance. In some patients, acute coronary syndrome occurs against the background of pre-existing stable angina, when the patient is well familiar with the nature of the sensations in the chest that occur during physical activity. Symptoms of acute coronary syndrome may resemble normal human pain, but much more intense, prolonged, and do not stop after taking nitroglycerin. Thus, if you have any sensations in the chest (from mild to strong) or any new symptoms in your health, you should consult a doctor and follow medical recommendations.
– What forms of heart attack exist?
– Sometimes myocardial infarction is disguised as other diseases. The gastrological variant is similar to the picture of an “acute abdomen”: abdominal pain, bloating, and with them weakness, drop in blood pressure, tachycardia. Only an electrocardiogram can clarify. The asthmatic variant occurs without severe pain in the heart, the patient begins to choke, he is given drugs to make breathing easier, which do not make him feel better. The cerebral variant resembles a stroke, confusion of consciousness and speech occurs. A “silent” heart attack occurs completely without pain and most often occurs in patients with diabetes mellitus. Severe fatigue and shortness of breath after physical efforts, which were previously given without difficulty, may be its only signs. Angina pectoris is another mask of a heart attack, under which it “hides” in approximately ten percent of patients. They only experience pain when walking. Often such patients come to the clinic on their own, where an ECG shows a heart attack.
– What are the risk factors characteristic for the development of myocardial infarction?
– Among the risk factors for myocardial infarction, there are those that we cannot influence. For example, a person’s gender, age. Men are more often susceptible to heart attacks; women up to a certain age are protected by their sex hormones. Age – over 65 years old, heredity. Although, it must be admitted, in recent decades, heart attacks have become “younger”; people much younger than 65 years of age are increasingly becoming its victims. The second group of risk factors are those that completely depend on our lifestyle and can be reduced. These are smoking, hypertension, elevated cholesterol and glucose levels, physical inactivity, and excess weight. Knowing your cholesterol level is just as important as your blood pressure. If the numbers exceed the norm, it is necessary to do a detailed blood test for a lipid profile to determine what percentage of total cholesterol is low- and high-density lipoproteins. This will help the doctor select modern medications. Let me emphasize: reducing blood cholesterol levels by just ten percent reduces mortality from heart attack by 15 percent. It must be remembered that elevated blood sugar levels contribute to the formation of atherosclerotic plaques. Regarding weight. To find out if your weight is normal, just determine your waist circumference. In women, it should normally be less than 80 cm, in men - less than 94 cm.
– A heart attack, as is known, is very dangerous in a recurrent form. What brings the risk of another heart attack closer?
– The threat of a recurrent heart attack is increased by four main factors: atherosclerosis, high blood pressure, increased blood clotting and carbohydrate metabolism disorders. These risk factors can only be controlled with the help of properly selected drug therapy. To slow down the further development of atherosclerosis, it is important to prevent the formation of fatty plaques in the vessels. For this purpose, modern drugs are prescribed. You cannot change the dosage of medications at your own discretion. If any problems arise, the doctor will adjust the course of treatment.
– What assistance can those who are nearby provide to the patient before the ambulance arrives?
– If you have the slightest suspicion that a person has symptoms of a heart attack, you should immediately call an ambulance. Before the team arrives, the patient should be kept at rest.
If you have chest pain, take nitroglycerin under the tongue in the form of a tablet or spray (if you are not prone to low blood pressure) and an aspirin tablet if there are no contraindications. If there is no effect, taking nitroglycerin can be repeated, but immediately call an ambulance. An ambulance should be called if this is the first attack of angina pectoris in your life, as well as if the chest pain or its equivalent intensifies or lasts more than five minutes, especially if all this is accompanied by deterioration in breathing, weakness, vomiting, if the chest pain does not stop or intensifies in within five minutes after dissolving the nitroglycerin tablet. The first hours of the disease are critical, not to mention the fact that sudden cardiac death can occur in the first minutes. Thus, the prognosis depends primarily on the speed of medical care provided: the sooner it is provided, the greater the chances of saving the heart muscle, as well as on the success of the measures taken and, accordingly, on how much the heart muscle is damaged, as well as the presence and degree risk factors for cardiovascular disease in a particular person.
– How to behave at home after a myocardial infarction?
– For recovery after a heart attack, the right diet is important: a minimum of fat, nothing fried or spicy, more fiber, dairy products, fruits, vegetables, fish. You will have to give up sausages and sausages, ready-made semi-finished products (dumplings, cutlets, etc.) - they contain a lot of hidden fats that increase cholesterol levels. For the same reason, pates, liver dishes, offal, and caviar are prohibited. Milk fat is also dangerous: you will have to sharply limit butter, fatty cottage cheese, cheese, milk, kefir, sour cream, and cream. When cooking chicken or turkey, all fat and skin must be removed from the carcass. And, of course, a minimum of salt. Vodka, cognac and other strong drinks are canceled. But sometimes you can allow a glass of natural dry red wine. You'll have to change some habits too. If you used to smoke, cigarettes are now completely taboo. An indisputable fact: almost 80 percent of people who have had a heart attack can return to normal life.
– What can you recommend to patients who have had a heart attack?
– To restore the functioning of the heart muscle, it is important to engage in physical therapy. Walking is a great restorative. After just one and a half to two months of training, you can walk at a pace of up to 80 steps per minute without shortness of breath or weakness. And over time, switch to very fast walking - up to 120 steps per minute. Climbing stairs, cycling, and swimming are also useful. Dancing two or three times a week for 30-40 minutes, which will also give a person additional positive emotions. However, make sure that your heart rate during exercise does not exceed more than 70 percent of your threshold.
- How to calculate this?
– From 220 you need to subtract your own age - this is the maximum heart rate. Then we calculate the percentages. For example, for a 60-year-old person, the threshold load is calculated as follows: 220–60 = 160 heart beats per minute, and 70 percent will be 112. This figure should be a guideline. But if unpleasant sensations appear at this frequency, the load needs to be reduced. And most importantly: after a heart attack, lifting heavy objects is strictly contraindicated.
– What means are used to treat myocardial infarction today?
– People who have had a myocardial infarction have a very high risk of having another heart attack, stroke, and death from cardiovascular disease. It is especially important for them to follow all recommendations that will help reduce this risk. Long-term care of patients after hospital discharge is aimed at achieving two main goals. The first is the prevention of the development of recurrent myocardial infarction and death from it (the so-called “secondary prevention”). The second is the correction of complications of myocardial infarction. Secondary prevention includes the maximum possible impact primarily on the risk factors for myocardial infarction, which we have already discussed. As well as drug therapy. In the absence of contraindications, patients after myocardial infarction are prescribed the following groups of medications. These are drugs that thin the blood by preventing platelets (blood cells) from sticking (aggregating) to each other and to the walls of blood vessels. Taking these drugs reduces the likelihood of a thrombus (a blood clot in the lumen of a blood vessel or in the cavity of the heart) forming in the arteries, thereby blocking the main mechanism for the development of myocardial infarction. When treated with these drugs, there is a risk of bleeding, most often gastrointestinal bleeding. Therefore, you should pay attention to the presence of black stools, blood in the stool, or other signs of bleeding. If alarming symptoms occur, you should immediately consult a doctor. Drugs that lower blood cholesterol levels have a direct beneficial effect on arterial walls, “stabilizing” atherosclerotic plaques and preventing their rupture. Because rupture of atherosclerotic plaque is the mechanism that triggers blood clotting and artery blockage, taking these drugs reduces the risk of another heart attack. The doctor selects the dose in such a way as to achieve the target level of cholesterol, and especially low-density lipoprotein cholesterol (LDL), the target numbers are less than 2.6 mmol/L (preferably less than 1.8 mmol/L). The drugs are prescribed for an indefinite period. Only a doctor prescribes medications. In addition, there is a set of mandatory medications after myocardial infarction, which are indicated in the patient’s discharge document after treatment in the hospital, and the duration of their use.
– What are the complications of myocardial infarction?
– Arrhythmia is considered the most serious. It is the most common complication of myocardial infarction. The greatest danger is ventricular tachycardia (a type of arrhythmia in which the ventricles of the heart take on the role of pacemaker) and ventricular fibrillation (chaotic contraction of the walls of the ventricles). In addition to arrhythmia, heart failure (decreased contractility of the heart). It happens quite often with myocardial infarction. The decrease in contractile function occurs in proportion to the size of the infarction. As well as mechanical complications (cardiac aneurysm, rupture of the interventricular septum). They most often develop in the first week of myocardial infarction and are clinically manifested by a sudden deterioration in hemodynamics. The mortality rate in such patients is very high, and only urgent surgery can save their lives. Recurrent (constantly recurring) pain syndrome occurs in approximately one third of patients with myocardial infarction; dissolution of the thrombus does not affect its prevalence. Post-infarction symptom complex. It manifests itself as inflammation of the heart sac, lung sac, or inflammatory changes in the lungs themselves. The occurrence of this syndrome is associated with the formation of antibodies.
– Is it possible for a person who has had a heart attack to use dietary supplements? Or, on the contrary, use them for preventive purposes?
– Biologically active food additives (dietary supplements) are not drugs, although they may have an external resemblance to drugs, for example, they contain some active substances (vitamins, minerals, etc.) that are part of the drugs, and are produced in the same dosage forms ( tablets, capsules, syrups, etc.), but in much smaller doses. In all approved documents, dietary supplements are defined as food products, so they cannot be used for the prevention, diagnosis, or treatment of disease. Remember that not a single dietary supplement has been seriously studied in terms of prevention, much less treatment of patients with myocardial infarction and heart failure. The safety of dietary supplements as food products is regulated by sanitary rules and regulations. Their side effects are often not studied, although they are possible, therefore the instructions for their use may not contain sections “Side effects”, “Contraindications”, “Precautions”. This allows manufacturers of dietary supplements to advertise them as absolutely safe products that can be used without consulting a doctor. Unfortunately, the practice of using dietary supplements around the world does not confirm this. It must be remembered: self-medication is life-threatening; you should consult a doctor for advice on the use of any medications.
– What modern methods of treating acute myocardial infarction exist?
– Treatment of myocardial infarction aims, first of all, to ensure the viability of the heart muscle. This is possible if coronary blood flow is restored in the first hours after the attack. This is the only method of treating myocardial infarction that can save a person’s life. Blood flow through the coronary arteries can be restored only in two ways, which are included in the standards of treatment for myocardial infarction. These are thrombolytic therapy (dissolution of a blood clot with the help of drugs) and surgical treatment: percutaneous transluminal angioplasty, most often with stenting of a coronary vessel, sometimes emergency coronary artery bypass grafting. Thrombolytic therapy with modern medications should ideally be carried out by an ambulance team. Angioplasty and stenting of the coronary arteries are performed in the cardiology clinic on an emergency basis for those patients who promptly sought medical help; For those patients who sought help late, these procedures are carried out delayed or as planned and do not always help save the dead area of the heart muscle.
– What is a stent?
– A stent is a thin metal tube consisting of wire cells, inflated with a special balloon. It is injected into the affected vessel and, expanding, is pressed into the walls of the vessel, increasing its lumen. This improves the blood supply to the heart, quickly relieves pain, limits the size of the infarction, improves contractility in the area of the infarction, reduces the severity of heart failure, reduces the likelihood of developing complications and, as a result, reduces mortality. It should be borne in mind that the earlier treatment for myocardial infarction is started, the higher the effectiveness of treatment and the lower the likelihood of adverse outcomes. It must be remembered that only after a regular high-quality medical examination can you consider yourself healthy or having a disease in a state of stable remission. As well as the fact that early detection of the disease in the initial stages will allow timely and high-quality treatment to be carried out, maintaining efficiency and quality of life. Remember also that only a doctor can diagnose and treat, and the patient must conscientiously follow his instructions and have a firm conviction in the need to maintain a healthy lifestyle.
Cerebral signs
Headache is the most common but nonspecific manifestation. Occurs when there is a malnutrition of the brain.
This is a negative prognostic sign, since with progression, a stroke (acute ischemia of cerebral structures) is possible. It manifests itself as intense stabbing, shooting sensations in the occipital region, crown of the head, and temples.
Physical activity leads to an increase in the syndrome; taking antispasmodics and other pain-relieving drugs has no effect. Changing body position also aggravates the course.
The development of a stroke is indicated by an unbearable intensity syndrome occurring in the system with other signs: paresis, paralysis, trembling of the limbs, disturbances in the functioning of the sensory organs.
Dizziness
Vertigo forms for an identical reason. In this case, the vestibular apparatus is involved. At the level of cerebral structures, it is represented by the cerebellum.
The impossibility of normal nutrition ends with chaotic signals. The patient cannot navigate in space, sways, and her gait is unsteady. Falls are possible. The body position is forced, sitting or lying down.
Spontaneous regression of symptoms is uncommon, but this is not an indication of relief. An instrumental assessment of the effectiveness of cardiac activity puts an end to the issue.
Nausea
It is the result of ischemia of cerebral structures, as before. Special centers of the brain are involved. The symptom lasts indefinitely. Possibly throughout the entire period of microinfarction.
Vomit
Walks in the system with dizziness. This is the body's standard reaction to cerebral ischemia. The reflex leads to emptying of the stomach, even if there has been no food intake before.
The urge persists for 20-120 minutes or a little more. There is no relief even after repeated episodes. As in case of poisoning or toxic lesions.
Why? Because we are talking about a reflex process, the result of irritation of special centers of the brain.
Loss of consciousness
Occurs in critical cases. Indicates a worsening of the overall prognosis for the course of a microinfarction. It is relatively rare.
Syncope is a reason for hospitalization. Fainting develops rapidly, but has a pronounced preceding period.
Before the onset, there is tinnitus, painful perception of sound stimuli, burning in the scalp, darkening in the eyes, nausea, weakness in the legs and the whole body. Feeling of failure.
Repeated repetitions of this symptom are possible. In female patients especially, males are less prone to such an aggressive, combined course of microinfarction.
Disturbance of the senses
Various plans.
- From the point of view. Flashing of flies before the eyes (small flickering dots in the field of vision), photopsia (lightning flashes, simple hallucinations, resulting from irritation of the visual cortex of the brain), fog, darkening, changing the shape of objects, inability to determine the distance to them.
- From the hearing point of view. Tinnitus, humming, ringing. Decreased sharpness, complete lack of perception on one side. Distortions and illusions are possible. Indicates damage to special cranial nerves.
- Smell. Hallucinations. False, phantom odors. Usually unpleasant. Hydrogen sulfide (stale eggs), rotten meat, burning and others.
- The sense of touch is also impaired. The patient perceives non-existent tactile influences. There is a feeling of goose bumps running through the body.
The symptoms are not persistent. They go away after treatment and restoration of blood circulation to the brain, activation of cardiac activity.
Paralysis, paresis, innervation disorders
Almost 100% indicate a current stroke or transient ischemic attack (a transient deviation, no less dangerous, but short-lived).
Accompanied by a lack of sensitivity on one side. When the left side of the cerebral structures is damaged, the right side suffers and vice versa. Hands and feet don't obey. Facial muscles too.
Possible disturbances in speech, thinking, cognitive activity, loss of consciousness.
Within 1-2 hours, a patient with ischemia should be taken to a neurological hospital for diagnostics.
At the same time, the degree of functional disorders of the heart is determined. If necessary, a cardiologist is involved.
Factors influencing the development of heart attack
A heart attack is a multifactorial pathology, that is, it is caused by the action of many causes at once. There are also risk factors that are likely to increase the incidence. These factors need to be known in order to eliminate and thereby reduce the risk of developing a heart attack or, if it has already developed, a second attack.
It is impossible to suffer a heart attack on your legs; strict bed rest is necessary
Risk factors are:
- atherosclerotic changes in blood vessels - a cholesterol plaque in atherosclerosis can increase, blocking the lumen of the vessel so much that the tissue starves, first under load conditions, and over time at rest. It can also break off and cause an embolism;
- thromboembolism - dense blood clots can break off, enter the systemic circulation, and then clog the coronary vessels. An embolus can be fat, a foreign body, or an air bubble;
- high blood pressure – contributes to damage to the vascular wall;
- poor nutrition – abuse of foods high in trans fats and cholesterol;
- excess body weight;
- smoking and alcohol abuse;
- sedentary lifestyle;
- congenital deformation of the vessel wall.
Clinical manifestations in men are more pronounced, manifest earlier and persist longer; in women they are weaker, often completely absent; a heart attack is more easily tolerated, but this complicates its diagnosis.
Based on this list, disease prevention is built. For example, if an increased content of lipids (fats) is detected in the blood, then the menu should be adjusted. The same should be done for patients who are overweight. It is important to quit smoking and minimize alcohol intake. There should be no restriction on physical activity - refusal of heavy, exhausting work should not exclude walks in the fresh air and moderate physical activity. Patients at risk should carefully monitor their blood pressure and overall health.
Recovery stages
Rehabilitation of patients after myocardial infarction is divided into stages:
- Inpatient
- until the parameters are normalized and the threat to life is eliminated, the patient is in the intensive care unit, then transferred to the cardiology department for up to two weeks. - Post-stationary
– its duration is individual (until the patient’s tissue scarring is completed), the average period is 28 days. - Supportive
– it has no deadline, your health is monitored by a cardiologist.
In order for the rehabilitation of patients with a heart attack to take place without complications, it is necessary:
- take an individual approach to drawing up rehabilitation measures;
- gradually and continuously implement the recommendations received.
Features of the rehabilitation program depend on:
- localization of necrosis;
- the extent of the spread of the process - extensive or small-focal infarction is diagnosed;
- presence of concomitant diseases.
Stationary stage
While in the hospital, the patient:
- comes out of an acute state;
- is undergoing drug therapy;
- receives psychological support;
- gradually recovers, gets used to dosed physical activity.
This stage begins with admission to the hospital. The patient's condition is kept under control by doctors. He is under 24-hour observation, first in the intensive care unit, then in the cardiology department. Normalized physical activity is indicated from the second day.
In the hospital, the patient receives complete information:
- about illness;
- changes that have occurred in the body;
- restrictions necessary to prevent relapse and complications.
He is being psychologically prepared for life after a heart attack.
Post-stationary stage
The patient is ready for discharge after sustained improvement in condition and sufficient physical activity.
He can restore his health:
- at home;
- boarding house for the elderly;
- sanatorium or rehabilitation center.
At this stage, home recovery for patients is only possible if relatives can provide round-the-clock care. If this is not possible, assistance will be provided by specialists working in a boarding house for the elderly. You can accommodate a relative there for the period of rehabilitation. Specialized rehabilitation centers and sanatoriums are indicated for difficult recovery processes.
At this stage of rehabilitation of patients with myocardial infarction, physical activity increases within reasonable limits. The body's reaction must be monitored.
Support stage
After a heart attack, you need to visit a cardiologist every three months (during the first year), then once every six months is enough.
Final steps to full recovery:
- compliance with reasonable dietary restrictions, giving up bad habits;
- gentle physical activity;
- taking medications;
- daily blood pressure measurement.
The maintenance stage has no deadline.
Goals and objectives of rehabilitation
Healed tissue has limited functionality, which leads to circulatory failure. The main goal of recovery after myocardial infarction is to adapt the body to new conditions. Program objectives:
- restoration of the cardiovascular system;
- psychological preparation of the patient, including the mindset for long-term rehabilitation in compliance with all doctor’s recommendations;
- prevention of possible complications - myocarditis, rhythm disturbances, aneurysm;
- general strengthening, preparing the patient’s body for stress, restoring physical indicators;
- return to work and a full life.
Diet
A properly formulated diet helps restore the body after illness and prevents relapse. The daily diet is divided into four to five meals, the last of which is two hours before bedtime. Portion sizes should be small.
The menu is being adjusted step by step. In the first days, light dishes without salt and spices are recommended.
In the future, the range of products is expanded due to:
- croup;
- seafood;
- vegetables, fruits, nuts;
- bran bread;
- vegetable oils;
- kefir and other low-fat fermented milk products;
- lean varieties of meat and fish.
Limit:
- yolks (2 pieces per week);
- sugar and products containing it (no more than 50 g per day);
- cream and butter (10-20 g);
- salt (up to 0.5 tsp per day).
Excludes:
- refractory fats, lard, offal;
- sauces, pickles;
- sausages, canned food, semi-finished products;
- caviar, fatty meats;
- strong broths;
- fatty cheeses;
- chocolate, ice cream, cream;
- coffee, soda;
- fast food.
Products are steamed, boiled, stewed, baked. Fried and smoked foods are prohibited. Fluid intake is 1.5 liters per day. If you are overweight, you can reduce it by following a gentle diet (without fasting).