High-sensitivity cardiac troponins
The emergence in clinical practice of various highly sensitive methods for determining cardiac troponin has become a new tool for clinicians diagnosing acute coronary syndrome. These tests also pose a challenge for laboratories and clinicians who are not yet familiar with sex-specific cutoff values. Healthy men and women studied in different age groups and geographic regions have marked differences in baseline values of high-sensitivity cardiac troponins I and T, leading to the establishment of sex-specific upper reference limits and cut-off values. Several differences in cardiac physiology, size, and structure may explain baseline differences in high-sensitivity cardiac troponins and outcomes between sexes. The clinical utility of using sex-specific cutoff values for the diagnosis and treatment of acute coronary syndrome remains unclear. To date, the only prospective study has failed to show improved outcomes for men or women when using sex-specific cutoffs; however, a major limitation is the frequent lack of diagnostic, therapeutic, and preventive interventions provided to women with low troponin levels. Based on the current literature, we argue that there may nevertheless be clinical value in using sex-specific cut-off values to assess suspected acute coronary syndrome, particularly in selected patient groups such as young women, who typically have lower baseline values high-sensitivity cardiac troponin. Future studies should prospectively evaluate differences in diagnostic, pharmacologic, and interventional treatment between men and women with myocardial infarction classified using sex-specific cutoff values for high-sensitivity cardiac troponin assays. Measurement of cardiac troponins—troponin T and troponin I—first appeared in clinical practice in the 1990s. Even with these earliest iterations of the analysis
However, they were more specific for myocardial damage than previous biomarkers, including when used in patients with reduced kidney function. Compared with creatinine kinase and myoglobin, cardiac troponins I and T are expressed only in cardiac myocytes, and cardiac troponins are expressed only in cardiac myocytes. detected in serum or plasma within several hours after myocardial injury. An increase in cardiac troponin levels above the 99th percentile of the upper reference limit (URL) is an indicator of myocardial damage. In addition to symptoms, electrocardiographic changes, and imaging findings, acute changes in cardiac troponins are a key component in the diagnosis of acute myocardial infarction (MI).
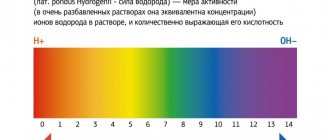
The limit of detection (LOD) of cardiac troponin T and I assays has historically been above the 99th percentile URL and has generally been undetectable in healthy populations. The first highly sensitive cardiac troponin assay (Elecsys Troponin T Gen 5 Short Turnaround Time [STAT] immunoassay from Roche Diagnostics) was approved by the US Food and Drug Administration (FDA) in early 2021. 14 ng/L for women and 22 ng/L for men or a single cut-off value of 19 ng/L with recommended use in combination with other signs and symptoms to diagnose MI. 7 hs-cTnI tests from Beckman Coulter and now also joins the latest FDA-cleared ARCHITECT STAT hs-cTnI assay from Abbott Laboratories, which also has 99th percentile sex-specific cutoff values.
As the various hs-cTnT and hs-cTnI assays gain widespread acceptance and adoption into clinical practice, evaluation of the data underlying the development of clinical decision values (uniform and sex-specific) for each assay is imperative. There is a lack of consistency in the definition of “healthy” cohorts across different statements and studies, which has led to the development of biologically non-equivalent clinical decision values that may influence the diagnostic outcome of each hs-cTnT and hs-cTnI assay. .8 In light of the widespread identification of sex cutoffs for high-sensitivity cardiac troponins, the purpose of this review is to examine sex differences in the pathophysiology of coronary artery disease, evaluate the evidence supporting the use of specific cutoff values for various assays, and assess the implications for the diagnosis and treatment of acute coronary syndrome (ACS) for each gender.
Sex differences in cardiac anatomy and pathophysiology are well known. Structurally, among individuals without cardiovascular disease, men have greater cardiac mass compared with women based on cardiac magnetic resonance imaging and echocardiography. Echocardiography shows that this difference in cardiac mass is present in the young. Healthy adults (aged 20–29 years) and older healthy adults (aged 60–70 years), even after adjusting for body surface area. Men also have higher left ventricular end-diastolic and end-systolic volumes, despite similar higher left ventricular ejection fractions in both sexes. These differences in heart mass and geometry between the sexes may be caused by sex hormones and are weakly related to differences in blood viscosity by sex.
The type and distribution of coronary heart disease also differs between sexes. Women with ACS are more likely to develop non-obstructive coronary disease than men. Non-ST-segment elevation myocardial infarction (NSTEMI) and unstable angina (UA) (as opposed to ST-segment elevation MI (STEMI)) are more commonly diagnosed in women compared to men with ACS (82% vs. 77%, respectively). Among patients with ACS, women also tend to have more comorbidities but fewer high-risk angiographic features. with more focal non-critical lesions and fewer plaque ruptures and necrotic core. Comorbidities that are more common in women compared to men with ACS include diabetes mellitus, hypertension, and a history of heart failure. cerebrovascular disease. Myocardial infarction with non-obstructive coronary arteries (MINOCA) is another clinical condition that is more commonly diagnosed in women compared to men. Smilowitz et al specifically note that MINOCA accounts for 10.5% of all MI diagnoses in women compared with 3.4% in men. MINOCA is currently recognized in the Fourth Universal Definition MI4 and is defined as MI with <50% stenosis of all epicardial vessels. Coronary microvascular dysfunction, as evidenced by the high prevalence of abnormal vasomotion following acetylcholine or adenosine administration, is one of several likely etiologies of infarction in women with MINOCA and is associated with adverse cardiovascular events in these women. MINOCA includes coronary thromboembolism, coronary spasm, plaque disruption, and coronary artery dissection in addition to myocardial diseases such as myocarditis and Takotsubo cardiomyopathy.
Conclusions.
Cardiac structural differences between men and women may explain sex differences in high-sensitivity cardiac troponins in healthy individuals. At any age, the prevalence and distribution of coronary heart disease also differs between sexes. While ACS with obstructive coronary artery disease has developed diagnostic approaches, other types of coronary artery disease, including MINOCA, have recently been recognized as clinically relevant. Given the variability in the types of coronary artery disease and the extent of comorbidity between sexes, developing therapeutic approaches and improving outcomes in both men and women remains a clinical challenge. Numerous studies have shown that normal or non-obstructive coronary angiography does not exclude coronary artery disease and does not completely predict cardiovascular morbidity and mortality. Thus, the use of sex-specific, highly sensitive troponin assays to detect small MIs (including MINOCA) in women may be a way to significantly eliminate disparities in clinical outcomes, especially if appropriate therapeutic and prophylactic measures can be taken in cases that may occur. were considered "false positives" in the past.
Reflecting differences in cardiac structure and mass, sex-specific 99th percentile URLs have now been identified in healthy men and women. This has led to the establishment of sex-specific clinical decision thresholds for the various hs-cTnT and hs-cTnI assays. It remains to be determined whether the discovery and exploitation of this underlying difference in cardiac troponin circulation between the sexes results in improved clinical performance of high-sensitivity cardiac troponin assays. Current literature indicates that sex-specific cut-off values may result in the identification of more women with positive biomarkers indicative of myocardial injury,
but studies have not yet demonstrated improved outcomes when patients with suspected ACS are followed for up to 1 year.
The discrepancy in potential diagnostic benefit and the paucity of data suggesting improved outcomes with the introduction of sex-specific cutoffs compared with a single cutoff exists for several different reasons. First, most studies to date are retrospective or observational studies that reclassify patients diagnosed with ACS using sex-specific cutoffs. Retrospective reclassification may not lead to changes in clinical practice and may not influence further studies (angiography rates) or therapeutic approaches (revascularization or medical therapy) in such studies. Thus, results measured at follow-up do not reflect clinical decisions made using high-sensitivity cardiac troponin assays and do not reflect any potential shifts in treatment that may occur in patients reclassified as having ACS using cutoff values depending on gender.
Two study designs included a cohort of patients who were diagnosed and treated based on sex-specific hs-cTnI assay cutoff values. Although the use of sex-specific cutoffs identified more men and women with myocardial injury, women in these studies were still less likely than men with a similar diagnosis to undergo coronary angiography, revascularization, and prescribed curative therapy despite a similar diagnosis. This finding highlights the possibility that clinicians may view the modest increase in cardiac troponin, defined by the lower sex-specific cutoff in women, as unimportant in influencing clinical decisions. A diagnostic test alone cannot lead to improved outcomes unless it is accompanied by a change in provider behavior.
In addition, most of these studies included patients with typical ACS symptoms. Women with typical ACS symptoms tend to be older and have more comorbidities compared to their male peers. Although this cohort represents the most common type of patient who would use and benefit from cardiac troponin measurement to diagnose MI, there may be special populations (eg, younger women) and diseases other than type I MI that are underrepresented in existing literature. Finally, serial monitoring of cardiac biomarkers assessing dynamic changes may attenuate the effect of a lower sex-specific threshold.
It is worth noting that the potential diagnostic and prognostic value of incorporating sex-specific cutoffs into clinical practice may be partially offset by the ease of using a single cutoff. Clinical practice has historically used a single cardiac biomarker threshold for both sexes, so clinicians at all levels of training and specialty may be more comfortable performing and interpreting a single clinical decision.
shutdown of high-sensitivity cardiac troponins for both sexes. However, many other assays and tests currently used in practice use sex-specific cutoffs, so any learning curve should be relatively rapid. However, finding differences in hs-cTnT and hs-cTnI in healthy men and women is a new tool and opportunity for assessing less common and less severe cardiovascular diseases that may disproportionately affect men and women. As mentioned previously, there is growing evidence for the diagnostic performance of sex-specific cutoff values of hs-cTnT and hs-cTnI assays; however, clinicians should be cautious in extrapolating these findings to other hs-cTnI assays as they may not be equivalent. The use of sex cutoffs has also been proposed as a prognostic tool in disease states other than ACS, as well as in primary prevention and risk stratification, which remain areas of active research.
general characteristics
High-sensitivity troponin I (hs-cTnI) is a sensitive early biomarker of myocardial infarction and an independent predictor of adverse outcomes in any symptomatic and positive patient with acute coronary syndrome (ACS). hs-cTnI have better diagnostic accuracy and the potential to detect myocardial damage earlier than current cTn tests. Low concentrations of hs-cTn can completely exclude acute myocardial infarction. In patients with congestive heart failure, high serum hs-cTn concentrations are a useful prognostic predictor independent of either reduced LV ejection fraction or BNP levels, suggesting that elevated hs-cTnI concentrations sensitively reflect developing myocardial injury.
Introduction
Despite clinical trial results showing benefits of statin therapy in asymptomatic patients at high cardiovascular risk, debate continues about the balance between the benefits and harms of therapy for primary prevention.
Importantly, high troponin levels may reflect subclinical coronary artery disease (CAD) and may help identify high-risk individuals who are candidates for targeted preventive therapy. The purpose of the WOSCOPS analysis was to evaluate the ability of cardiac troponin I, measured at baseline and 1 year after statin treatment, to predict coronary events.
Indications for use
1. The presence of symptoms indicating myocardial ischemia, incl. without any changes on the ECG. 2. Diagnosis of myocardial infarction in patients with chronic renal failure who have symptoms of myocardial ischemia (regardless of the severity of kidney damage). 3. Diagnosis of myocardial damage in patients receiving chemotherapy. 4. Patients with heart failure with or without preserved ejection fraction to assess the risk of mortality or hospitalization. Troponin levels greater than the 99th percentile are associated with a high likelihood of poor outcome. 5. All patients with signs of acute heart failure to exclude acute myocardial infarction.