Pulmonary stenosis
Pulmonary artery stenosis (narrowing) can be caused by isolated valvular, subvalvular or peripheral obstruction, and also occurs in combination with more severe congenital heart defects.
Pulmonary stenosis with an isolated valve occurs in 8-12% of cases of congenital heart defects in children. Subvalvular stenosis can result in a funnel-shaped appearance of the artery and is often found in children with a normal pulmonary valve. This condition may be caused by tetralogy of Fallot.
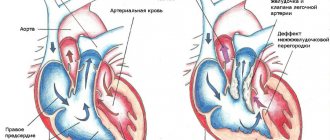
Peripheral narrowing of the pulmonary artery can lead to obstruction at the level of the main pulmonary artery, at the bifurcation, or in more distal branches. In some places, there is difficult patency, but stenosis can be caused by other congenital cardiac anomalies, for example, a ventricular septal defect or patent ductus arteriosus, etc.
Stenosis can be diagnosed in utero or shortly after birth. Critical narrowing of the pulmonary artery is considered potentially dangerous for newborns.
Ultrasound imaging of the heart during pregnancy may show isolated valve stenosis due to abnormal thickening or bicuspidity of the valve. Also, with the help of ultrasound, the doctor can detect stenosis caused by rubella infection during fetal development or accompanied by other congenital anomalies, such as tetralogy of Fallot or Noonan syndrome.
In infants, the condition is usually diagnosed by the presence of systolic murmurs while listening to the lungs with a phonendoscope.
Symptoms and diagnosis of pulmonary artery stenosis
Symptoms of stenosis depend on the severity of the pathology. The mild form may be asymptomatic; a more severe form of the pathology may cause the following symptoms:
- dyspnea
- chest pain
- fainting during exercise
- causeless fainting
Soft pulmonary systolic murmurs are heard when the child is lying down, but such murmurs can also be heard in healthy children and may be associated with physiological changes in the respiratory system.
Diagnosis of pulmonary artery stenosis may consist of the following procedures:
- echocardiography – allows you to confirm the presence of a valve defect;
- ECG - shows the presence of ventricular hypertrophy, right atrium and other abnormalities in the physiology of the heart;
- angiography allows you to confirm the diagnosis and is often prescribed to children with multiple cardiac anomalies;
- A chest x-ray allows the doctor to determine the enlargement of the right ventricle and atrium.
Treatment of pulmonary stenosis
Initial treatment of critical heart disease in a newborn includes general resuscitation and medications to dilate the ductus arteriosus. In the absence of pathological symptoms and the blood pressure in the right ventricle is less than 60 mm Hg. Art. The child is seen by a cardiologist every 1-2 years. These routine examinations include ECG, echocardiography and chest x-ray.
For infective endocarditis, surgical treatment is performed:
- in case of symptoms and blood pressure in the ventricle more than 60 mm Hg. Art. Cardiac catheterization is performed using valvotomy, which leads to the elimination of pulmonary valve insufficiency. If the procedure does not correct the problem, the pulmonary valve may need to be replaced;
- Percutaneous pulmonary valve implantation is an alternative to surgical valve correction and replacement of right ventricular dysfunction;
- Pulmonary artery balloon angioplasty, with or without placement of an expandable metal stent, can be used to treat the disease.
What is the pulmonary valve and where is it located?
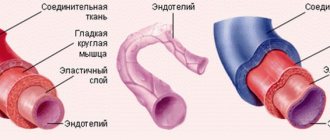
Pulmonary (PV) or pulmonary valve (PA) is an anatomical structure that separates the cavity of the right ventricle from the pulmonary trunk. The latter takes part in the formation of the pulmonary circulation, delivering venous blood to the lungs through a system of small arteries and capillaries.
In relation to external landmarks, the pulmonary valve is located in the area of attachment of the cartilage of the 3rd rib to the sternum on the left (auscultation point of the PC).
Structural components:
- 3 semilunar valves (flaps): anterior, left, right;
- 3 sinuses (“sinuses”);
- fibrous ring, the main function of which is the supporting frame for the valves.
The flaps are shaped like pockets attached to the fibrous ring, the free edges of which are directed towards the lumen of the vessel. The closure lines of the valves are called commissures. Thickenings in the central part of the valve are Morgagni's nodes.
The valves are formed by three layers:
- ventricular (ventricular);
- median (spongy);
- sinus (fibrous).
The valves are thickest at the point of attachment to the fibrous ring, tapering in the central direction. The valve structures are supplied with blood through separate arteries arising from the pulmonary trunk.
The histological structure of the fibrous ring and leaflets is similar to the structures of the endocardium - the inner connective tissue membrane of the heart. The top layer is represented by a thin epithelium, which protects the surface of the PC from the formation of blood clots. Elastic and collagen fibers of the lower layer provide density and extensibility.
Sinuses (or sinuses) are the space between the valves and the wall of the vessel, the name of each corresponds to the forming valve. The section of the artery wall that forms the sinus has a developed middle layer of smooth muscle cells and connective tissue elements. The latter becomes thinner towards the base of the sinus due to a decrease in the number of myocytes.
The fibrous ring is a triangular strand of dense connective tissue, which consists of collagen (the main component), elastin and a small amount of cartilaginous elements. The structures of the ring continue into the middle layer of the valves.
During embryogenesis, the PC develops from the mesenchyme, being part of the “ventricular outflow tract”.
Hemodynamics
The main function of the pulmonary valve of the heart is to ensure one-way blood flow in the pulmonary circulation system and prevent return (regurgitation) from the pulmonary trunk to the right ventricle.
During systole (the moment the heart contracts), the pressure in the pancreas exceeds that in the arteries, so the valve is in the open state, the valves are pressed against the wall of the vessel. When diastole (relaxation) occurs, blood rushes in the opposite direction, flows into the sinuses, as a result of which the valves close.
Pulmonary valve insufficiency
Pulmonary insufficiency occurs extremely rarely as a congenital anomaly. However, pathology often occurs as a complication after surgery or percutaneous angioplasty for pulmonary stenosis, as well as treatment for tetralogy of Fallot. Also, pulmonary valve insufficiency can develop as a result of a dilated pulmonary valve ring due to pulmonary hypertension or Marfan syndrome.
Significant pulmonary insufficiency can be caused by primary pulmonary hypertension, secondary pulmonary hypertension, infective endocarditis, rheumatic heart disease, carcinoid heart disease, Marfan syndrome and certain drugs, for example, methysergide, pergolide.
Pulmonary valve insufficiency is a serious pathology that is usually asymptomatic and is not accompanied by signs of right ventricular failure. With this pathology, a soft diastolic murmur is heard in the left upper region of the sternum and hypertrophy of the right ventricle is observed.
When diagnosing this pathology, the following studies are carried out:
- ECG;
- chest x-ray;
- color Doppler echocardiography;
- cardiac catheterization.
Treatment of pulmonary valve insufficiency
Pulmonary insufficiency usually does not require special treatment, but to monitor the pathology, it is necessary to conduct cardiograms every 1-3 years, depending on the severity and cause of the pathology. If symptoms or right ventricular dilatation are present, surgical pulmonary valve replacement is necessary. If severe right ventricular failure and pulmonary hypertension are detected, a heart transplant may be required.
Pulmonary insufficiency is usually well tolerated in childhood. Long-term studies have shown that pulmonary valve regurgitation can lead over time to progressive right ventricular dilatation, right ventricular dysfunction, exercise intolerance, gastric tachycardia, and, in extreme cases, sudden death.
Normal performance
To study the functioning of the CPA at the primary stage, a general clinical examination of the patient is used. Characteristic signs of violations:
- dyspnea;
- pulsation of the neck veins;
- pallor or cyanosis of the upper part of the body;
- during auscultation – additional noise at the point of valve projection.
Making a final diagnosis and choosing adequate treatment tactics depends on the results of instrumental methods that objectively assess the condition of this structure. The most common tests are electrocardiography (ECG) and echocardiography (echoCG).
ECG
There are no specific electrocardiographic signs of PC defects. Changes in the ECG occur when symptoms of heart failure due to a valve defect appear.
With regurgitation or stenosis of the pulmonary valve, hypertrophy of the right ventricle develops, which is established on the ECG in comparison with the state of the left sections.
Severe pancreatic hypertrophy (mass larger than left):
- the ventricular QRS complex is represented by qR or simply R in precordial lead V1;
- in V6 the QRS complex is deformed in rS, RS (occasionally – Rs);
- the degree of hypertrophy is reflected by the height of the R wave in V1 and the depth of S in V6 - the greater the difference between them, the more significant the increase in the myocardium;
- the ST segment in V1 is under the isoline, the T wave is negative;
- in V6 ST is located above the isoline, T-positive.
Moderate hypertrophy (the mass of the pancreas is less than the left one, but impulse conduction is slow):
- The QRS complex in V1 is observed as rsR or rSR;
- V6 deformation in qRS.
Moderate hypertrophy is represented by deformation of the QRS complex:
- in V1 – rS, RS, Rs;
- in V6 – qR;
- the amplitude of the R wave in V1 is increased;
- the S waves in V1 and R waves in V6 are reduced.
A shift of the electrical axis of the heart to the right is noted at each stage of hypertrophy.
ECHO
Ultrasound examination of the heart is considered the gold standard for diagnosing PC defects. The method allows you to study the anatomical features and functional state of the valves. To visualize internal hemodynamics, Doppler echocardiography is used.
The pulmonary valve on ECHO is depicted in the form of a three-lamellar formation, the elements of which bend into the lumen of the vessel during RV systole.
Standard PC indicators:
- structure – normoechoic, homogeneous;
- peak blood flow velocity – 0.5-1.0 m/s;
- average pressure gradient – up to 9 mm Hg. Art.;
- lumen diameter – 11-22 mm.
During ultrasound, the structure of the coronary artery and the presence of pathological formations are studied. The main changes for various defects are presented in the table.
| PA stenosis | Insufficiency (regurgitation) of the coronary arteries |
|
|
General information about heart defects in children
Heart disease
- a violation of the anatomical structure of the walls or valves of the heart, as well as the blood vessels that enter or exit it. Cardiac function and hemodynamics in the entire circulatory system are impaired.
Depending on the reasons for development, there are congenital
and
acquired vices
.
It is believed that congenital ones appear during the first weeks of pregnancy during the “initial formation” of future life. The reasons for the development of defects have not been studied reliably, but they predispose to them:
- genetic diseases (50% of children with Down syndrome suffer from this disorder);
- diabetes mellitus in a pregnant woman;
- bad habits of the expectant mother (half of children with fetal alcohol syndrome (FAS) have heart defects);
- infections (a mother who has had rubella in the first trimester will almost always have a child with severe pathology);
- taking medications prohibited for pregnant women;
- phenylketonuria in an expectant mother.
However, heart disease does not always develop from birth. It can manifest itself as a complication of diseases suffered in childhood (rheumatism, influenza, tonsillitis) in severe forms. This disorder is called an acquired defect.
hearts.
Diagnosis of heart defects in children
During the initial examination, a pediatrician, neonatologist or pediatric cardiologist conducts an examination and auscultation of possible heart murmurs. The presence of swelling, shortness of breath, heart rhythm disturbances, and problems with physical or intellectual development are checked. Based on the results of the inspection, the question of the necessary examination is decided.
Cardiac echocardiography (EchoCG) – combines cardiac ultrasound and cardiogram. The method determines the rhythmogram and structural changes in the heart. EchoCG is an informative method.
Radiology shows the actual size of the heart, its chambers and the relationship of the organ to the size of the chest.
Coronary angiography – a catheter is inserted through the veins or arteries in the arm, groin, or neck (vein only) and reaches the heart. Then a contrast agent is passed through it. This method determines the contractile function of the heart.
Medical equipment uses expert-class equipment from world-famous manufacturers.
The task of the Children's Medical Department is to provide a full range of medical care from prevention to treatment, when symptoms of a defect appear from birth to 18 years.
In our children's department, appointments are conducted by doctors who have undergone special training to identify health problems in children and infants, taking into account all age-related characteristics.
Pediatric doctors at the Paracelsus Clinic work according to the principles of evidence-based medicine (international protocols drawn up on the basis of clinical trials). This minimizes the likelihood of a false diagnosis.
Parents play a big role in the early diagnosis of heart defects in children. The direction in which the preliminary examination will be carried out depends on how closely the parents monitor the health of their child and how correctly they can describe his condition to the doctor.
Symptoms of heart defects in newborns and children
Usually the pathology is detected by a neonatologist in the first days of a baby’s life:
- cyanosis (blue discoloration) or grayness of the skin;
- tachypnea - rapid shallow breathing;
- widening of the nostrils when inhaling;
- grunting while inhaling;
- swelling of the legs, abdomen, face;
- breathing problems when feeding.
In a less severe form, it manifests itself at a growing age:
- fatigue during exertion;
- shortness of breath, pain in the heart area when playing sports;
- swelling of the hands, ankles, feet.
The earlier the clinical manifestations appear, the more difficult the process.
Important! Note to parents
Regardless of whether a child has a heart pathology or not, it is necessary to undergo regular medical examinations.
It is especially important to make an appointment with a pediatric cardiologist before starting sports. There are disorders in which the cardiovascular system can cope with them through compensatory force. Diseases go undetected for years.
When playing sports, the load on the cardiovascular system increases many times over. Compensatory mechanisms in this mode are often insufficient, which is manifested by dizziness, loss of consciousness, and can cause a life-threatening condition for the child.
This does not mean that playing sports is strictly contraindicated. The type of sport and load must be determined by a doctor.
If a child is diagnosed with a heart defect, medical supervision when playing sports is mandatory. A medical examination by a pediatric cardiologist, pediatrician, or cardiac surgeon is required.