Characteristics of normal heart sounds.
The first sound occurs during systole after a long pause.
It is best heard at the apex of the heart, since the systolic tension of the left ventricle is greater than that of the right. By nature, the first tone is longer and lower than the second.
The second tone is formed during diastole after a short pause. It is best heard at the base of the heart, as it occurs when the semilunar leaflets of the aortic valves and pulmonary trunk close. Unlike the first tone, it is shorter and higher pitched.
In pathology, when the sonority of tones can change, it helps to distinguish the first and second tones by the fact that the first tone coincides with the apical impulse (if the latter is palpated) and with the pulse of the aorta and carotid artery.
Changes in heart sounds can be expressed as:
v weakening or enhancing the sonority of one or both tones,
v in changing their timbre, duration,
v in the appearance of bifurcation or splitting of fundamental tones,
v the appearance of additional tones.
Heart sounds are amplified when large air cavities are located near it (large pulmonary cavity, large gas bubble of the stomach) - due to resonance. The sonority of the tones also depends on the composition of the blood flowing through the heart: when the viscosity of the blood decreases, as is observed with anemia, the sonority of the tones increases.
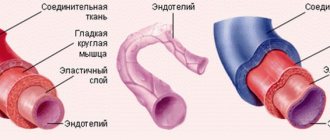
Fig. 8. Valve projection locations
on the anterior chest wall
In the diagnosis of heart diseases
It is of great importance to identify changes in tones caused by damage to the heart itself, i.e. caused by cardiac causes.
A weakening of both tones can be observed with a decrease in the contractility of the heart muscle in patients with myocarditis, myocardial dystrophy, cardiosclerosis, with collapse, or accumulation of fluid in the pericardial cavity.
An increase in both tones occurs due to an increase in the influence of the sympathetic nervous system on the heart. This is observed during heavy physical work, anxiety, and in people suffering from Graves' disease.
More often than a change in both heart sounds, there is a change in one of them, which is especially important in the diagnosis of heart disease.
Weakening of the first sound at the apex of the heart is observed:
· Insufficiency of the mitral and aortic valves.
With mitral valve insufficiency during systole, the valve leaflets do not completely cover the left atrioventricular orifice.
Strengthening of the first sound at the apex of the heart is observed:
· with narrowing of the mitral orifice.
Weakening of the first tone at the base of the xiphoid process of the sternum
· with insufficiency of the tricuspid valve and the pulmonary valve.
Strengthening of the first tone at the base of the xiphoid process of the sternum is heard:
· with stenosis of the right atrioventricular orifice.
An increase in the first tone is also observed with extrasystole - premature contraction of the heart - due to low diastolic filling of the ventricles.
Normally, the strength of the second tone over the aorta and pulmonary trunk is the same.
Weakening of the second tone over the aorta is observed:
· in case of aortic valve insufficiency, or due to their cicatricial compaction;
· with large destruction of the aortic valve leaflets, the second sound above it may not be heard at all;
· with a significant decrease in blood pressure;
Weakening of the second tone above the pulmonary trunk is observed:
· in case of insufficiency of its valve (which is extremely rare);
· with a decrease in pressure in the pulmonary circulation.
Strengthening of the second tone can be observed either above the aorta or above the pulmonary trunk.
In cases where the second tone is more sonorous above the aorta, they speak of the accent of the second tone on the aorta, but if it is more sonorous above the pulmonary trunk, they speak of the accent of the second tone on the pulmonary artery.
The emphasis of the second tone on the aorta is observed:
· when the pressure in it increases (hypertension, nephritis, heavy physical work, mental agitation), since at the beginning of diastole the blood hits the valve flaps with greater force.
The emphasis of the second tone on the pulmonary artery appears:
· with increased pressure in the pulmonary circulation, blood overflow of the pulmonary vessels (for example, with mitral heart defects),
· obstruction of blood circulation in the lungs and narrowing of the pulmonary artery bed (with emphysema, pneumosclerosis, etc.)
Heart murmurs.
When auscultating the heart, in some cases, in addition to tones, sound phenomena called heart murmurs are heard.
Murmurs can occur: inside the heart itself - intracardial, outside of it, extracardiac.
Organic murmurs occur due to anatomical changes in the structure of the heart valves.
Functional noises appear:
in case of dysfunction of unchanged valves
· with an increase in blood flow speed or a decrease in blood viscosity.
The most common cause of intracardial murmur is heart defects.
Based on the time the noise appears during systole or diastole, systolic and diastolic murmurs are distinguished.
Systolic murmur appears:
· when, during systole, blood, moving from one part of the heart to another or from the heart to large vessels, encounters a narrowing on its way.
· with stenosis of the aortic mouth or pulmonary trunk, since with these defects, during the expulsion of blood from the ventricles, an obstacle arises in the path of blood flow - narrowing of the vessel.
· listened to insufficiency of the mitral and tricuspid valves.
Its occurrence is explained by the fact that during ventricular systole, blood flows not only into the aorta and pulmonary trunk, but also back into the atrium through an incompletely covered mitral or tricuspid opening. Since this not completely covered hole is a narrow gap, noise occurs when blood passes through it.
Diastolic murmur appears in cases where there is a narrowing in the path of blood flow in the diastole phase:
· with narrowing of the left or right atrioventricular orifice, since with these defects during diastole there is a narrowing in the path of blood flow from the atria to the ventricles.
· in case of insufficiency of the aortic valve, pulmonary trunk - due to reverse blood flow from the vessels into the ventricles through the gap formed when the leaflets of the altered valve are not completely closed.
During auscultation it is necessary to determine:
1) the ratio of noise to the phase of cardiac activity (to systole or diastole);
2) properties of noise, its nature, strength, duration;
3) noise localization, i.e. best place to listen;
4) direction of noise conduction.
The ratio of noise to systole or diastole is determined by the same criteria by which we distinguish between the first and second sounds.
Date added: 2015-03-03; ; ORDER A WORK WRITING
Question 4. Reasons for weakening and strengthening (emphasis) of tone II.
A weakening of
the second tone
is recognized in the presence of a symptom such as a decrease in the sound of the second tone in comparison with the first tone or when the degree of sonority of both tones is the same at the base of the heart (the place of auscultation of the aorta and pulmonary artery).
Weakening of the second sound over the aorta is very characteristic of heart disease - aortic valve insufficiency. The cause of aortic regurgitation syndrome is the complete or partial destruction of the valve leaflets, their scarring and reduction in area. In the absence of the obturator function of the valve, blood flows back through the gap (regurgitates) from the aorta into the left ventricle. A decrease in the area of the valve leaflets and the absence of a push of blood onto the leaflets leads to a decrease in the sonority of the second sound in the aorta. If the valves are completely destroyed, the second sound in the aorta may not be heard at all.
Weakening of the second tone in the pulmonary artery occurs with rather rare valvular heart defects: pulmonary valve insufficiency and narrowing of its mouth. The mechanism for weakening the tone in these cases is the same conditions as for similar aortic defects.
Strengthening, accent
of tone
II . Normally, in adults, when listening and comparing the second tone on the aorta and on the pulmonary artery, it is noted that their volume is the same. This is explained by the fact that the pulmonary valve is located closer to the chest than the aortic valve, due to which the transmission of sound phenomena from them is equalized, although the greater blood pressure in the aorta also gives a greater push force on the aortic valve leaflets when they close.
Question 5. Splitting, splitting of heart sounds.
Double tone is a condition when, during auscultation of the heart, instead of one continuous sound, two sounds are heard following each other after a short period of time. If the time interval between these two sounds is very small and there is no complete impression of the separateness of the sounds, then they talk about splitting the tone. This condition can occur in both I and II.
Splitting (incomplete separation) and bifurcation (complete separation) of both I and II tones can be physiological, i.e. found in completely healthy people, and pathological, observed in some heart diseases. Physiological separation of tones is more common in young people and is usually associated with the act of breathing, and therefore is not constant.
Splitting and bifurcation of the first tone is caused by non-simultaneous closure of the mitral and tricuspid valves. In healthy people, this phenomenon can sometimes appear during exhalation, when, due to increased pressure in the chest, more blood flows into the left parts of the heart than into the right, which causes asynchronous closure with faster closure of the mitral valve. Therefore, the sound phenomena of the valve component of the AV valves on exhalation are perceived separately, and on inspiration, the first sound is heard as one sound.
Splitting or bifurcation of the first tone in pathological conditions is especially characteristic of blockade of one of the branches of the His bundle, when excitation to one of the ventricles arrives late, which means that the mechanical process of contraction of the ventricles occurs later. The atrioventricular valve of the “blocked” ventricle is delayed in closing. This separation of the first tone does not depend on the phases of breathing - it is constant.
The separation of the second tone is heard more often on the pulmonary artery. It is explained by the non-simultaneous closure of the aortic and pulmonary valves. Under physiological conditions, this phenomenon occurs and is more pronounced during inspiration, when, with a decrease in intrathoracic pressure, the suction effect of the chest causes a slightly larger volume of blood to pass through the right than the left parts of the heart. In such a situation, systolic emptying of the right ventricle requires more time than the left. Therefore, the pulmonary component of the second tone is significantly behind the aortic one. This is the mechanism of splitting and bifurcation of the second tone, which is heard during inspiration, especially with deep breathing.
In patients with increased blood pressure in the pulmonary circulation (mitral heart defects, pulmonary hypertension, thromboembolism of the branches of the pulmonary artery), the duration of systole of the right ventricle, in comparison with the left, also increases, which causes a significant lag of the pulmonary component of the second sound from the aortic component. This is the most common mechanism of splitting and bifurcation of the second tone.
In patients with bundle branch block, especially the right bundle branch, splitting of the second sound is also possible due to asynchrony of the end of systole of the right and left ventricles. With right bundle branch block, the onset of right ventricular diastole, manifested by the pulmonary component of the second sound, occurs significantly later than the onset of left ventricular diastole. Moreover, with such a pathology, both heart sounds may be split.
“Tripartite rhythms” associated with the appearance of additional diastolic or systolic sounds should be distinguished from bifurcation of heart sounds.
https://phonocardio.com/wp-content/uploads/2015/01/LG_high_156.mp3
Pregnant woman about 30 years old. Ten years ago, an IVS defect was operated on. Pulmonary hypertension, pulmonary artery systolic pressure just over 50 mm (echocardiographically). Right bundle branch block. Obvious strong emphasis on the second, pulmonary component of the second tone (arrow). The recording was carried out in the supine position; the almost fixed T2 splitting should be checked in the vertical position.
Idiopathic pulmonary hypertension in a pregnant woman. Pulmonary artery systolic pressure greater than 70 mm echocardiographically. T2 is not split on auscultation, clearly accentuated to the left of the sternum. Early diastolic high-frequency decreasing noise of pulmonary regurgitation (phono noise), absolutely identical to the noise of aortic insufficiency. This murmur is strong additional evidence in favor of pulmonary hypertension. With normal pressure in the pulmonary artery, the noise of pulmonary regurgitation cannot be so high-frequency.
Reasons and mechanism for the formation of accent of the II tone, splitting of the II tone
P tone accent. It is assessed by comparing the volume of the second tone in the second intercostal space at the edge of the sternum, respectively, on the right or left. The emphasis is noted where the tone is louder, and may be on the aorta or pulmonary trunk. Acceptance of tone II can be physiological and pathological. The physiological emphasis is age-related. It is heard on the pulmonary trunk in children and adolescents. It is usually explained by the closer location of the pulmonary trunk to the site of auscultation. The emphasis on the aorta appears by the age of 25-30 and somewhat intensifies with age due to the gradual thickening of the aortic wall. We can talk about a pathological accent in two situations:
1) when the accent does not correspond to the proper point of auscultation corresponding to age (for example, loud volume II on the aorta in a young man) and
2) when the volume of the second tone is greater at a point, although corresponding to the age, but it is too high in comparison with a healthy person of this age and physique, or the second tone has a special character (ringing, metallic)
The reason for the pathological acceptance of the second tone in the aorta is an increase in blood pressure and (or) compaction of the valve leaflets and the aortic wall. The emphasis of the second tone on the pulmonary trunk is usually observed in pulmonary arterial hypotension (mitral stenosis, cor pulmonale, left ventricular failure)
Physiological splitting of the second tone is heard exclusively at the base of the heart during inhalation and exhalation or during physical activity. At the end of a deep inhalation, when the chest expands due to a decrease in pressure in it, the blood is somewhat retained in the dilated vessels of the small circle and therefore flows in smaller quantities into the left atrium, and from there into the left ventricle. The latter, due to less blood filling, ends systole earlier than the right one, and the closure of the aortic valve precedes the closure of the pulmonary valve. During exhalation, the opposite conditions are created. In the case of increased pressure in the chest, blood, as if squeezed out of the vessels of the pulmonary circle, enters in large quantities into the left part of the heart, and the systole of the left ventricle, and therefore the beginning of its diastole, occurs later than the right.
At the same time, a split second tone may be a sign of serious pathological changes in the heart and its valves. Thus, a bifurcation of the second sound at the base of the heart (second intercostal space on the left) is heard with mitral stenosis. This is due to the fact that the hypertrophied and blood-filled right ventricle ends systole later than the left. Therefore, the aortic component of the second sound occurs earlier than the pulmonary one. Bifurcation or splitting of the second sound in bicuspid valve insufficiency is associated with greater blood filling of the left ventricle than normal, which leads to prolongation of its systole, and the diastole of the left ventricle begins later than the right. Because of this, the aortic valve closes later than the pulmonary valve.
Quiet pulmonary component of the second tone
The pulmonary component of the second sound may be quite quiet and normal. On inhalation, it may not be heard at all, creating the false impression of a paradoxical splitting of the second tone. This is due to the distance of the heart from the surface of the chest due to an increase in lung volume. However, in most cases the components of the second tone can be distinguished. The pulmonary component of the second tone is weakened in pulmonary stenosis. It is also significantly attenuated, usually to the point of complete absence, in tetralogy of Fallot, pulmonary atresia, and transposition of the great vessels.
Change in heart sounds
A change in heart sounds can primarily be expressed in a weakening or strengthening of the sonority of one or both of them, in a change in timbre, duration, in their splitting or bifurcation, in some cases - in the appearance of additional tones. In this case, determining the place of best listening to pathological sound phenomena is of diagnostic importance. Strengthening of the second tone in the 2nd intercostal space on the left
speaks of its emphasis on the pulmonary artery (determined by comparing its volume and timbre on the pulmonary artery and aorta).
This indicates an increase in pressure in the pulmonary circulation, which can be observed in diseases of the heart, as well as the respiratory system (mitral defects, emphysema, pneumosclerosis, chronic pneumonia). The intensification of the second tone in the second intercostal space on the right
indicates its emphasis on the aorta, which is observed with an increase in blood pressure in the systemic circulation (arterial hypertension), as well as in the case of hardening of the wall and valve of the aorta in atherosclerosis and a number of other diseases.
Strengthening the first sound at the apex of the heart
most often occurs with narrowing of the left atrioventricular orifice (mitral stenosis), tachycardia. This is due to the fact that with this defect, during diastole, less blood flows into the left ventricle than normal, and it contracts more quickly (transition from a relaxed to a tense state). In addition, with mitral stenosis, the timbre of the first tone changes due to vibrations of the sclerotic cusps of the mitral valve. It takes on a crackling tone, reminiscent of the sound of a flag flapping in the wind. This sound at the apex of the heart with mitral stenosis is called “popping”.
Intensity of tone I (English):
Weakening of the first sound at the apex of the heart
can be observed during inflammatory processes of its muscles (myocarditis), cardiosclerosis (scar changes in the heart muscle), and damage to the valve apparatus (bicuspid and tricuspid, as well as aortic).
Weakening of the second sound on the aorta
possible with aortic defects (aortic valve insufficiency or stenosis of its mouth).
Weakening of the second tone on the pulmonary artery
occurs when the valve is insufficient or its opening is narrowed (stenosis).
If during auscultation of the heart, instead of one of the tones, two short ones are heard, following each other after a short period of time, then this indicates a split tone
.
If the difference in the time of occurrence of these components is insignificant and the impression of splitting is not created, we are talking about tone splitting
. Thus, there is no fundamental qualitative difference between bifurcation and splitting of tones. There is only some quantitative difference: splitting is the initial phase, and bifurcation is a more pronounced degree of disruption of the unity of tones.
Bifurcation and splitting of tones can be physiological and pathological. For example, the bifurcation of the first tone may depend on the non-simultaneous closure of the bicuspid and tricuspid valves as a result of changes in pressure in the chest during different phases of breathing. But more often, a split in the first tone indicates pathological changes in the heart. It occurs, as a rule, when one of the legs of the atrioventricular bundle (bundle of His) is blocked, which leads to non-simultaneous contraction of the right and left ventricles of the heart. This can occur with significant blockade of the atrioventricular (atrioventricular) node, with sclerosis of the initial part of the aorta.
Physiologically split I tone (English):
Forked I tone (English):
In case of severe heart damage, a three-part rhythm can be heard. It is caused by weakening of the myocardium (inflammation, degenerative changes, toxic lesions) of the left ventricle and occurs as a result of rapid stretching of its walls under the pressure of blood flowing from the atrium. This creates the melody of a three-part rhythm (first, second and additional third tones), reminiscent of the clatter of a galloping horse - the “ gallop rhythm.”
" It is also figuratively called the “cry of the heart for help,” since it is a sign of severe heart damage. The rhythm of the gallop is best heard directly by the ear (along with the sound, a slight impulse is perceived, transmitted from the heart to the chest in the diastole phase) in the area of the apex of the heart or the third-fourth intercostal space on the left. It can be heard especially clearly when the patient is lying on his left side. But this creates inconvenience for direct listening with the ear. In such cases, a phonendoscope is used.
There are protodiastolic, mesodiastolic and presystolic gallop rhythms (depending on the diastole phase, during which the pathological third sound appears).
Translation: gallop rhythm
heard as a three-membered or four-membered rhythm. Additional sounds appear in diastole and are caused either by atrial contraction, or early rapid filling of the ventricle, or a combination of both mechanisms (summation gallop).
Quadruple rhythm (English):
Much more common are bifurcation and splitting of the second tone, caused by non-simultaneous closure of the pulmonary artery and aortic valves due to increased pressure in the pulmonary or systemic circulation. Bifurcation and splitting of the second tone can also be physiological and pathological.
Physiological splitting of the second tone is heard exclusively at the base of the heart during inhalation and exhalation or during physical activity. At the end of a deep inhalation, when the chest expands due to a decrease in pressure in it, the blood is somewhat retained in the dilated vessels of the small circle and therefore flows in smaller quantities into the left atrium, and from there into the left ventricle. The latter, due to less blood filling, ends systole earlier than the right one, and the closure of the aortic valve precedes the closure of the pulmonary valve. During exhalation, the opposite conditions are created. In the case of increased pressure in the chest, blood, as if squeezed out of the vessels of the pulmonary circle, enters in large quantities into the left part of the heart, and the systole of the left ventricle, and therefore the beginning of its diastole, occurs later than the right.
Paradoxical splitting of the second tone (English):
Pathological bifurcation of the second tone (English):
Fixed splitting of the 2nd tone (English):
At the same time, a split second tone may be a sign of serious pathological changes in the heart and its valves. Thus, a bifurcation of the second sound at the base of the heart (second intercostal space on the left) is heard with mitral stenosis. This is due to the fact that the hypertrophied and blood-filled right ventricle ends systole later than the left. Therefore, the aortic component of the second sound occurs earlier than the pulmonary one. Bifurcation or splitting of the second sound in bicuspid valve insufficiency is associated with greater blood filling of the left ventricle than normal, which leads to prolongation of its systole, and the diastole of the left ventricle begins later than the right. Because of this, the aortic valve closes later than the pulmonary valve.
One should distinguish from the true splitting of the second tone its sound melody, which only superficially resembles splitting. An example is the additional tone that occurs during the opening of the bicuspid (mitral) valve with mitral stenosis. It has a high-pitched clicking tone and is perceived as a loud echo following the second tone. The additional tone, together with the clapping first and second, form a peculiar melody, reminiscent of the cry of a quail. Hence the name of this sound phenomenon, heard with mitral stenosis at the apex of the heart - “ quail rhythm”
" Its distribution area is extensive - from the apex of the heart up and into the axillary fossa.
Sometimes, when listening to the heart, against the background of rare and dull tones, a lonely, very loud tone appears, the so-called “gun tone” Strazhesko
. It is caused by the simultaneous contraction of the atria and ventricles, which is observed with complete atrioventricular block, i.e. when impulses from the atria do not reach the ventricles and they each contract in their own rhythm (the atria contract more often), but in some cycle their contractions coincide.
Publications in the media
Aortic valve insufficiency is a pathological condition characterized by retrograde blood flow from the aorta into the left ventricular cavity through a defective aortic valve.
Frequency. Among those who died from various heart pathologies, aortic valve insufficiency was detected in 14% of cases, of which in 3.7% - in isolated form, and in 10.3% - in combination with other defects. Since 1999, more than 80% of heart valve surgeries have involved aortic valve replacement.
Etiology • Rheumatism, including cases of secondary infective endocarditis (46.5%) • Medionecrosis (18%) • Primary infective endocarditis (12.8%) • Congenital anomalies (flapping cusp syndrome, isolated aortic valve insufficiency, annuloaortic ectasia , abnormalities in the number of aortic valve cusps), including cases of secondary infective endocarditis - 13.5% • Syphilis (2.1%) • Aortitis in Reiter's disease, ankylosing spondylitis, rheumatoid arthritis (2.1%) • Connective tissue diseases, such as syndrome Marfana et al. (1.9%) • Traumatic and spontaneous rupture of aortic valves (1.3%) • Atherosclerosis (0.9%) • Arterial hypertension (0.9%).
Pathophysiology • Hemodynamic disturbances are caused by regurgitation of blood from the aorta into the left ventricle during diastole. The volume of regurgitation depends on the area of the defect, the magnitude of the diastolic pressure gradient between the aorta and the left ventricle, the duration of diastole • An increase in the diastolic volume of the left ventricle leads to its tonogenic dilatation • According to the Frank-Starling law, the left ventricle ejects an increased volume of blood into the aorta, which, together with regurgitation, leads to a decrease in diastolic blood pressure, an increase in systolic and pulse blood pressure • As myogenic dilatation develops, the end-diastolic volume and end-diastolic pressure of the left ventricle increase, which leads to stagnation of blood in the pulmonary circulation • Congestion in the pulmonary circulation increases with the development of relative insufficiency mitral valve due to dilatation of the left ventricle • Compensation mechanisms: decreased peripheral vascular resistance, tachycardia, left ventricular hypertrophy.
Clinical picture and diagnosis • Complaints •• No complaints - 4.5% •• Episodes of angina - 20.1% •• Syncope episodes - 1.0% •• Dyspnea on exertion - 31.4% •• Orthopnea - 2.8 % •• Symptoms of systemic venous hypertension - 25.6% •• Paroxysmal nocturnal dyspnea (cardiac asthma) or pulmonary edema - 32.4% •• Combination of dyspnea with syncope and episodes of angina - 0.8% •• Other symptoms - 1 .3%.
• Peripheral symptoms are caused by low diastolic and high pulse blood pressure. It should be borne in mind that all peripheral symptoms are nonspecific and are possible with neuroses, anemia, thyrotoxicosis, arteriovenous malformations, etc. •• Corrigen's sign (carotid dance) - pronounced pulsation of the carotid arteries •• High and fast pulse •• Musset's sign - shaking of the head with each pulse wave •• Müller's sign - pulsating uvula •• Pulsation of retinal arterioles •• Quincke's sign - pulsating color change lips or nail bed, synchronous with pulse; determined by pressing on them with a glass slide •• Hill's symptom - the difference between blood pressure in the arms and legs is more than 20 mm Hg •• Double Traube tone - listening to loud (similar to a pistol shot) tones on the femoral arteries •• Durosier's symptom - systolic murmur on the femoral artery when it is clamped proximal to the site of auscultation and diastolic murmur when the femoral artery is clamped distal to the site of auscultation •• Listening to heart sounds on the palmar surface of the hand •• Listening to heart sounds on the palmar surface of the hand when raising the hand up •• Listening to the pulse above the superficial palmar arch .
• Valve symptoms •• Soft (flowing) diastolic decreasing murmur, following immediately after the aortic component of the second sound (best heard in the second intercostal space to the right of the sternum during exhalation when the patient’s torso is tilted forward), carried out to Botkin’s point •• Rough musical murmur (murmur “cooing pigeon”) occurs when the valve flaps or perforates the valve •• With decompensation and a pronounced increase in end-diastolic pressure of the left ventricle, the intensity of the murmur of aortic regurgitation weakens •• Austin Flint murmur is a mesodiastolic low-frequency murmur of relative mitral stenosis, arising in connection with the covering of the anterolateral mitral leaflet valve with a stream of regurgitation in severe aortic insufficiency. The degree of attenuation of the first tone reflects the severity of decompensation of the defect for the same reason. •• Systolic murmur over the aorta, caused by an increase in the volume of ejection from the left ventricle, can be heard in the absence of aortic stenosis.
• Left ventricular symptoms are caused by hypertrophy, dilatation and insufficiency of the pumping and contractile functions of the left ventricle •• Diffuse, prolonged apical impulse, shifted to the left and down •• Palpation detectable III tone •• Increase in the area of relative dullness of the heart to the left •• Auscultatory signs of congestion in the lungs - diffuse moist rales of various sizes, best heard in the basal regions.
• Symptoms of an underlying disease , such as Marfan syndrome, aortic aneurysm, syphilis, infective endocarditis.
Special studies • ECG: signs of hypertrophy and overload of the left parts of the heart, primarily the left ventricle. • X-ray examination of the chest organs: bulging of the left ventricular arch and aorta, enrichment of the pulmonary pattern in pulmonary hypertension.
• EchoCG •• Dilation of the cavity and hypertrophy of the left ventricular myocardium •• Violation of local and global systolic, as well as diastolic functions of the left ventricle •• Dilation of the ascending aorta •• Damage to the aortic valve leaflets (defects, vegetations, abnormalities in the number of leaflets, expansion of the fibrous ring, leaflet prolapse) •• In Doppler mode - pathological flow from the aorta to the left ventricle during diastole, the volume of which (recorded in color mapping mode) corresponds to the severity of the defect •• Increased systolic pressure of the right ventricle with stagnation of blood in the pulmonary circulation •• Signs lesions of other heart valves with combined defects •• In order to determine the size of the prosthesis, it is necessary to measure the diameter of the aorta at the level of the fibrous ring, sinuses and ascending limb ••
Transesophageal echocardiography is performed for the purpose of detailed diagnosis of the condition of the thoracic aorta, more accurate identification of vegetations on the valves, thrombosis of the left atrium in the presence of atrial fibrillation, as well as for patients in whom transthoracic visualization turned out to be difficult (due to obesity, emphysema, etc.).
• Catheterization of the left and right ventricles and aorta •• In case of left ventricular failure - increase in end-diastolic pressure of the left ventricle •• In case of congestion in the pulmonary circle - increase in pressure in the right ventricle, pulmonary artery wedge pressure •• Tests are performed to determine the prognosis for pulmonary hypertension with aminophylline and oxygen inhalation •• Depending on the volume of regurgitation as a percentage of the stroke volume of blood, four degrees of aortic valve insufficiency are distinguished ••• I degree - 15% ••• II degree - 15–30% ••• III degree - 30–50%, ••• IV degree - more than 50%.
• Left ventriculography , ascending aortography •• The presence and degree of regurgitation is determined by the number of contractions required to completely expel the contrast agent from the cavity of the left ventricle •• The presence of zones of hypo- and akinesia of the left ventricle indicates myocardial ischemia •• Combined valvular lesions are also diagnosed.
• Coronary angiography •• Performed in the presence of episodes of angina and positive results of stress testing, as well as in all women over 45 years of age, men over 40 years of age and all candidates for aortic valve replacement to exclude concomitant coronary artery disease.
TREATMENT • Drug therapy •• For asymptomatic mild aortic insufficiency, only annual dynamic monitoring (examination, echocardiography, ECG) and limitation of isometric physical activity are indicated (an increase in aortic regurgitation and damage to the aortic root is possible) •• For moderate asymptomatic aortic insufficiency, ACE inhibitors and conduct a clinical examination every 6 months •• In case of severe asymptomatic aortic insufficiency, constant use of peripheral vasodilators and clinical examination every 6 months (or immediately in case of decompensation) are necessary •• Treatment of decompensated aortic insufficiency is carried out according to the general principles of treatment of circulatory failure (vasodilators, cardiac glycosides, diuretics ).
• Surgical treatment •• Indications: aortic regurgitation grade III–IV or grade II in the presence of at least one of the following conditions: heart failure functional class III–IV (according to the New York Heart Association classification), angina pectoris, syncope, acute left ventricular failure (cardiac asthma or pulmonary edema), end-diastolic pressure in the left ventricle above 15 mm Hg •• Contraindications: severe concomitant pathology that threatens the patient’s life; terminal stage of circulatory failure •• Methods of surgical treatment ••• Aortic valve replacement with a mechanical artificial heart valve under artificial circulation ••• Biological prostheses are used in children ••• In the presence of an aneurysm of the ascending aorta - simultaneous replacement of the aortic valve and ascending aorta with a valve-containing conduit according Bentall or Cabrol method.
Specific postoperative complications • Thromboembolism • Secondary infective endocarditis of prostheses • Degenerative changes in biological valves and the need for re-prosthesis • Aneurysms of the ascending aorta when using disc prostheses with a small opening angle.
Prognosis • In the natural course, the 5-year survival rate does not exceed 45%, and the 10-year survival rate does not exceed 38% • After identifying symptoms of the disease, the average life expectancy is 2–5 years • After identifying left ventricular dilatation, the 10-year survival rate does not exceed 56% • With acute development of the defect (usually infective endocarditis), the average life expectancy is 7 months •• With surgical treatment, hospital mortality is 1–3%, 12-year survival exceeds 70% (with initial heart failure of functional class III according to the New York Heart Association classification ). Synonym. Aortic valve insufficiency
ICD-10 • I06.1 Rheumatic aortic valve insufficiency • I06.2 Rheumatic aortic stenosis with insufficiency • I35.1 Aortic (valvular) insufficiency • I35.2 Aortic (valvular) stenosis with insufficiency • Q23.1 Congenital aortic valve insufficiency