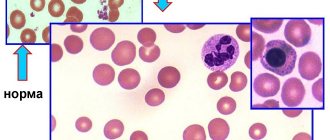
Normoblasts (normocytes) are the last, still nuclear, stage of red blood cells (erythrocytes) on the way to an adult, full-fledged state.
At this stage, normoblasts have a nucleus, so that, having lost it, they can turn into a young, nuclear-free cell containing hemoglobin and already capable of performing the main task of red blood cells (participation in respiration).
Before becoming normoblasts, future red blood cells go through a certain path.
As is known, all blood elements originate from a stem cell - it is the ancestor of future leukocytes, platelets, erythrocytes, etc., since it gives rise to several sprouts, among which is the erythrocyte (from it will come the cells of the erythroid series, including, and those of interest to us are normoblasts).
The youngest, morphologically distinguishable cell of the red row is the erythroblast,
which was formerly called proerythroblast. This is a fairly large cell (14 - 20 microns), containing an equally large nucleus, but does not even have signs of what an adult red blood cell is so valued for - it does not contain hemoglobin.
Detailed description of the study
Anemias are conditions that occur when the number of red blood cells - red blood cells - and the concentration of hemoglobin in a person's blood are significantly reduced.
Hemoglobin is a complex iron-containing protein found in red blood cells and is essential for transporting oxygen from the lungs to the tissues.
The main causes of anemia include:
- Impaired or decreased production of red blood cells, which may be associated with deficiency of iron or B vitamins, the presence of certain cancers, inhibition of the hematopoietic function of the bone marrow;
- Significant loss of red blood cells after massive bleeding (posthemorrhagic anemia);
- Increased breakdown (hemolysis) of red blood cells (hemolytic anemia).
Anemia can be acute or chronic. Chronic anemia, as a rule, accompanies other diseases (diabetes mellitus, cancer, chronic renal failure) and in most cases is asymptomatic or with minimal clinical manifestations.
The main clinical symptoms of anemia:
- Increased fatigue;
- Dyspnea;
- Dizziness;
- Tachycardia - rapid heartbeat;
- Pale skin.
Anemia is a fairly common condition diagnosed in both men and women. However, some factors increase the risk of developing pathology:
- Diet low in iron source foods (vegetarianism);
- Acute and chronic kidney diseases;
- Some autoimmune diseases (diabetes mellitus);
- Oncological diseases;
- Inflammatory bowel diseases;
- Genetic predisposition;
- Chronic infectious diseases (tuberculosis);
- Conditions after injuries and surgical interventions;
- Chronic bleeding.
To diagnose anemia, a number of laboratory parameters are determined. This comprehensive laboratory test includes all the necessary tests to diagnose anemia and determine the causes of its development.
General blood test extended with leukocyte formula and reticulocytes.
The analysis allows you to determine the concentration of hemoglobin, estimate the number of blood cells, as well as a number of other important indicators (color index, normoblasts).
This test evaluates three types of blood cells:
- Red blood cells (erythrocytes and reticulocytes) Erythrocytes are the most numerous group of all the formed elements of blood. They contain iron-containing protein - hemoglobin and together with it transport oxygen throughout the body. A decrease in hemoglobin concentration is the main indicator of anemia. Reticulocytes are immature red blood cells. The number of reticulocytes reflects their production by the bone marrow. The study of this parameter allows us to assess the hematopoietic function of the bone marrow.
- White blood cells (leukocytes) Leukocytes are cells that are constantly present in the blood, lymphatic system and tissues, and are an important part of the body's natural defense (immune) system. They provide protection against infections and also participate in the formation of inflammation and allergies. The number of leukocytes in the blood is relatively stable. A change in the number of leukocytes occurs in response to a change in the state of the body (infectious disease, inflammation, etc.).
- Platelets Platelets are blood cells that circulate in the blood and are necessary for its normal clotting. When a vessel wall is damaged, platelets help stop bleeding by adhering to the site of injury and forming a temporary plug. Diseases or conditions that are associated with low platelet levels (thrombocytopenia) or decreased platelet function increase the risk of developing anemia.
Also, with anemia, normoblasts, the precursors of reticulocytes, can be found in the blood. Normally, these cells can only be found in the bone marrow; their appearance in the bloodstream is a sign of pathology.
- ESR according to Westergren (venous blood) Erythrocyte sedimentation rate (ESR) is an indicator that depends on the ratio of protein fractions in the blood and the number of red blood cells. A change in ESR may indicate the presence of an inflammatory, autoimmune or oncological disease, which may cause the development of anemia. An increase in ESR is normally observed in any acute or chronic inflammatory process.
- Transferrin, ferritin and THC These indicators reflect the metabolism of iron in the body. This trace element is mainly included in the hemoglobin of red blood cells and is necessary for their normal production by the bone marrow. A person gets iron from foods (liver, red meat, spinach, legumes). When iron is absorbed in the intestine, it is transported by transferrin. Determining the level of transferrin reflects the total “reserves” of iron in the body. TIBC (total iron-binding capacity of serum) is an indicator that reflects the amount of iron that can be bound by transferrin. In healthy people, part of the iron entering the body is contained in hemoglobin. The other part is stored in tissues in combination with ferritin or hemosiderin. Ferritin is a protein complex that acts as the main “storage” of iron in the body. A small portion of ferritin is present in the blood; by measuring this indicator, iron reserves can also be assessed. These studies allow us to indirectly assess the amount of iron in the body in order to diagnose its deficiency and determine the cause of anemia.
- Folates and vitamin B12 Vitamin B12 and folic acid (vitamin B9) are representatives of the B vitamins, which are necessary for the body to produce red blood cells, white blood cells, and the synthesis of nucleic acids. Vitamin B12 also ensures the functional activity of cells in the central nervous system. Folates are salts of folic acid, a natural form of vitamin B9.
Vitamin B12 and/or folic acid deficiency reflects a chronic lack of one or both of these vitamins. Long-term deficiency of vitamin B12 or folic acid can lead to macrocytic anemia. In this case, the production of red blood cells by the bone marrow decreases, while they increase in size, and their ability to transport oxygen is significantly reduced, which causes hypoxia (oxygen deficiency in tissues).
Characteristic clinical signs of B12 deficiency anemia include:
- Constantly increasing weakness, apathy;
- Rapid heartbeat, heart pain;
- Weakness in the legs, “numbness” of the limbs;
- Swelling and pale complexion.
The most common cause of vitamin B12 deficiency is impaired absorption in the intestine. This may be due to chronic inflammatory diseases of the intestinal mucosa (atrophic gastritis), surgical removal of part of the organ, or some hereditary absorption pathologies.
Most anemia is a complication of other diseases, so in order to choose the right treatment tactics, it is necessary to find out the cause of the anemia. The studies included in this complex make it possible to assess the qualitative and quantitative composition of cells and biochemical parameters of the blood system, as well as to identify disturbances in its functioning. Based on the test results, it is possible to carry out a primary diagnosis of anemia, as well as a differential diagnosis of the types of disease.
A detailed description of the studies and reference values are presented on the pages with descriptions of individual studies.
Normal blood level is zero
Normally, these cells are not found in the blood,
therefore, there can be no talk of increased values of normoblasts when studying preparations (norm – 0).
They may or may not exist, and then it’s time to count if they can be detected. The exception to these rules is newborn children.
In a child in the first days of life, their presence in a general blood test should not be surprising: the increased content in the bone marrow and the appearance of normoblasts in the blood is explained by the increased production of erythropoietin during this period, which leads to an increase in red blood cells and hemoglobin. A few days later, when erythropoietin production decreases, the values of these indicators also drop down.
After some time from birth, more precisely, between 2 and 3 months of life, the child again has an increased level of
normoblasts and reticulocytes and again due to increased synthesis of erythropoietin, which does not cause concern for pediatricians, because this process is physiological.
After this surge, the child’s norms for these indicators will begin to approach the adult norms more and more every month, therefore, normoblasts will also not be found in children’s blood products, but will begin to be detected, as they should be, only in the myelogram.
normoblasts released from the bone marrow into the blood
Their absence in the blood, however, does not exclude their diagnostic significance, because they do not appear just like that, but due to some pathological changes, one way or another, affecting the main hematopoietic organ - the bone marrow.
Since the word “blast” means “sprout,” all descendants of blast can no longer be considered sprouts, so it would be more correct not to apply this name to further forms, but to attach the ending “cyt” to them. In this regard, the outdated word “normoblasts” is present in the vocabulary of specialists with extensive experience only out of habit, while young doctors already call this cell a normocyte.
From birth to great achievements
However, by focusing on the names, we have deviated somewhat from the topic. So, the events take place in the bone marrow:
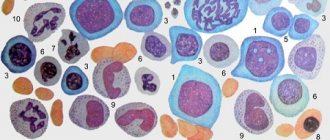
Stage 1: erythroblast
Erythroblast
- the first cell that can be identified under a microscope in a bone marrow preparation. A rounded nucleus, a delicate mesh structure of chromatin, several small nucleoli (usually 2 - 4), no clearing around the nucleus yet - this is the morphology of the ancestor of cells that will later become erythrocytes. In a general analysis of the blood of a healthy person, you don’t even need to look for it, since it simply cannot be there, because it has only just arisen and, before it goes “out into the world,” it must acquire new features and qualities in order to become workable in the peripheral blood, and, therefore, useful.
Stage 2: pronormocyte
Having passed the erythroblast stage, a very young cell slightly reduces its size (10 - 15 microns) and begins to change the structure of the nucleus, so that later it is easier to get rid of it (the nucleus becomes smaller and coarser, the nucleoli disappear, a slight perinuclear clearing appears around the nucleus) - this is no longer erythroblast. The new cell is called a pronormocyte
, although some continue to call it in the old way -
pronormoblast
. At this stage, the cell of the erythroid series is very poorly differentiated in the myelogram, because it has not yet completely lost the features of its predecessor, and has not yet acquired new ones.
Stage 3: normoblast (normocyte)
However, very little time passes before the “hero of our story” appears from an unrecognizable cellular structure - the normoblast
or
normocyte
.
It begins to be saturated with hemoglobin, which first concentrates around the nucleus ( basophilic
normocyte), and then spreads to the entire cytoplasm, turning the cell into
a polychromatophilic
normoblast, that is, the cell is clearly preparing to perform its responsible function.
As normoblasts accumulate complex chromoprotein (Hb), the need for the nucleus disappears; it only prevents the accumulation of hemoglobin by its presence. Having received a sufficient amount of Hb, the normocyte becomes oxyphilic
: the cytoplasm spreads over almost the entire territory, the nucleus loses its significance, therefore it becomes very small (pyknotic), coarsened with a structure changed beyond recognition, reminiscent of a cherry pit.
Stage 4: birth of a red blood cell
A normoblast, which is about to get rid of a nucleus that is no longer needed, remains a normoblast for some time, but in small numbers. Having finally pushed out the nucleus, the cell turns into a “newborn” polychromatophilic erythrocyte
, preserving a small amount of hereditary information (RNA), which will finally leave the cell within 24 hours, although it is difficult to call the “newly formed” form a cell (more likely, also out of habit).
Young red blood cells, saturated with hemoglobin and having lost their last connection with their “homeland,” are called reticulocytes
, which very soon, after they arrive in the bloodstream (up to 48 hours), will lose the last thing that emphasizes their young age - the reticulum, and turn into full-fledged adult blood cells -
erythrocytes
. A special stain helps detect reticulocytes in the blood. The entire path traveled by an erythrocyte from an erythroblast to a cell that has lost its nucleus takes at least 100 hours.
It is obvious that normally red cells at the normoblast level (before it becomes a reticulocyte) do not appear in the blood of a healthy person of all ages.