Diseases of the cardiovascular system
With pain in the chest on the right side, almost every doctor will first suspect the presence of cardiac pathologies, especially if the patient is no longer young, and the patient himself leads a sedentary, unhealthy lifestyle and has a history of cardiovascular and endocrine diseases.
Aortic aneurysm
An aneurysm is a weak section of the wall of the main artery in our body. In this place the wall stretches, bulges, and at some point it can either burst or tear. This condition is life-threatening, therefore, at the first suspicion of an aneurysm, the patient will be prescribed an X-ray or MRI, where the pathology will be identified and a decision will be made on the need for surgical treatment.
Angina pectoris
If there is pain in the upper right side of the chest, this may indicate the presence of angina pectoris: it occurs due to impaired blood supply to the myocardium and is often a consequence of atherosclerosis (the formation of plaques on the inner walls of blood vessels).
Pericarditis
The pathology is caused by the accumulation of fluid in the cavity of the heart muscle (pericardium), as a result of which its function is impaired. This condition is most often observed in men, and at a young age - from 20 to 50 years.
Myocardial infarction
Sudden acute pain in the chest on the right, more often in women and less often in men, which does not go away even after taking strong painkillers, indicates myocardial infarction. This is a deadly condition caused by impaired blood supply to the heart muscle.
Substernal pain
General information
Substernal chest pain is a common complaint in the emergency department; its diagnosis presents certain difficulties for a number of reasons:
- when complaining of chest pain or pain in the upper abdominal cavity, there is always the possibility of heart disease;
- pain associated with visceral organs can always radiate to various places in the chest or abdominal wall;
- accurate diagnosis requires interpretation of the patient's subjective perception of pain;
- the diagnosis is based primarily on anamnestic data, the collection of which depends, of course, on the experience and erudition of the doctor;
- assessment of physical signs and data from additional tests are not often helpful in the emergency department.
to assess acute chest pain . However, their widespread use in clinical practice is limited by a number of factors:
- studies are aimed at identifying patients with acute myocardial infarction and, as a rule, ignore other diagnoses, many of which are potentially fatal and require urgent hospitalization of the patient;
- Based on statistical data, these algorithms are based on the probability of diagnosis, but the probability of a particular diagnosis is difficult to apply to a specific patient;
- even if the likelihood of a serious complication (such as acute myocardial infarction) is low, local diagnostic standards and potential liability often force hospitalization of the patient;
- Absolute sensitivity of the system is impossible with any diagnostic scheme. Modern research helps to clarify the role of physical diagnostic methods in the assessment of chest pain.
In case of acute chest pain , the emergency department physician should first think about its potentially life-threatening causes:
- unstable angina,
- acute myocardial infarction,
- aortic dissection,
- pulmonary embolism,
- spontaneous pneumothorax
- esophageal rupture.
If serious or potentially life-threatening causes of chest pain are excluded, the patient can be released for follow-up outpatient observation (if necessary).
Onset and duration of pain
Typical angina pectoris (angina) is episodic, lasts 5-15 minutes, occurs during physical activity and goes away after 3-5 minutes at rest or with sublingual nitroglycerin. Unstable angina can also occur at rest, lasts longer and does not go away as easily. Variant angina (Prinzmetal's angina) occurs without provocation, often at rest or at night, but usually resolves after taking nitroglycerin. Patients with variant angina usually tolerate moderate physical activity without any particular difficulty. Pain during acute myocardial infarction usually lasts more than 15-30 minutes. Pain from myocardial ischemia in typical cases has an increasing character until reaching maximum intensity, while pain from aortic dissection or pulmonary embolism is usually severe at the very beginning. Pain of esophageal origin is described by patients as either heartburn , pain when swallowing (odynophagia) and/or spasm-like pain. Heartburn is a burning sensation in the sternum, often with an epigastric component. It usually occurs 15-60 minutes after eating, more often after a heavy meal. It can be triggered by certain body positions, such as bending or lying on your back or left side. Odynophagia is a sensation of pain in the esophagus during the passage of a bolus.
The pain may be described by the patient as burning. It occurs when a bolus of food comes into contact with an inflamed mucous membrane, or is noted as very strong, but short-term pain when the bolus passes through a narrowing of the esophagus. Esophageal spasm is perceived by the patient as a dull pain in the center of the chest, which lasts from several seconds to several minutes. However, it is often almost impossible to distinguish between esophageal and cardiac pain. Almost one third of patients with acute myocardial infarction or unstable angina have heartburn as their main complaint. Chest wall pain may last only a few seconds or continue for hours. The key points for differentiating such pain are their connection with a certain body position and local pain upon palpation of the chest wall.
Characteristics of chest pain
Sharp, piercing and cutting pain in the chest is usually of musculoskeletal origin. In one large study, 74% of patients with documented PE had pleuritic chest pain , and another 14% of patients had non-pleuritic pain. In the differential diagnosis of the etiology of visceral retrosternal pain, the quality of pain is not sufficiently informative: in patients with acute myocardial infarction the pain can be burning, and in patients with esophageal reflux it is usually pressing. Angina pain almost always has a retrosternal component, as with many other causative factors of deep visceral pain. With angina, pain often radiates to the neck, shoulders and down the inside of the left arm or both arms. In patients with aortic dissection, pain typically radiates to the back and upper abdomen as the dissection progresses. In patients with esophageal reflux, pain always has both retrosternal and epigastric components and radiates infrequently; in approximately 20% of cases in the back, much less often in the upper extremities (with severe exacerbations).
The main causes of chest pain
There are several groups of patients admitted to intensive care with chest pain, so knowledge of the most common diagnoses in such cases can be very useful. Chest pain in childhood and adolescence rarely has a cardiac origin and is most often associated with pathology of the chest wall, respiratory tract, with feelings of fear and anxiety, or with some idiopathic causes. Patients with numerous unexplained symptoms often complain of pain in the region of the heart, but they can usually be recognized by the unusual abundance of these “symptoms” without any convincing data, negative examination results, or anamnesis from numerous visits to doctors.
Elderly patients who develop acute myocardial infarction are more likely to present with either nonretrosternal chest pain or no pain (compared with younger individuals). In addition, older adults with confirmed acute myocardial infarction are more likely to have nonspecific symptoms, such as:
- fainting;
- stroke;
- weakness;
- confusion;
- nausea.
In typical cases angina is paroxysmal in nature, lasts 5-15 minutes (rarely more than 20 minutes), is caused and reproduced by physical activity and goes away with rest or with sublingual administration of nitroglycerin, usually within 3 minutes. In more than 90% of patients, pain is localized retrosternally. In almost 70%, the pain usually radiates to the neck, shoulders or upper limbs. For each patient, the nature of repeated attacks changes very slightly. In a lying position, patients usually do not feel better, although they lie down to rest at the beginning of an attack: most often it is better for them to sit quietly. Only 50% of patients with spontaneous angina have ECG changes during an acute and painful attack. Variant angina occurs without provocation, often during rest or during normal daily activities. During an acute attack, the ECG increases the ST segment, which indicates transmural myocardial ischemia. Variant angina is presumably caused by spasm of the epicardial coronary arteries , either in normal vessels (about 1/3 of such patients) or in vessels affected by atherosclerosis (about 2/3 of patients). Attacks may be complicated by tachyarrhythmias , bundle branch block, or block in the AV node. Variant angina usually resolves with sublingual nitroglycerin.
Unstable angina
Unstable angina is a syndrome intermediate between ordinary angina and acute myocardial infarction. If left untreated, it often leads to early heart attack and death. Modern treatment methods significantly reduce this risk, so timely recognition of the disease and hospitalization of the patient are very important. Depending on the course of the disease, three subgroups are distinguished:
- angina pectoris with recent onset – 4-8 weeks;
- angina with a variable pattern, becoming more frequent, severe, or resistant to nitroglycerin;
- resting angina.
The latter two subgroups are associated with a higher risk of early myocardial infarction and death. In unstable angina, the ECG may show nonspecific changes in the ST segment; increases in serum levels of CK and CK-MB are also minimal and have no diagnostic significance.
Acute myocardial infarction
Anginal pain lasting more than 15 minutes that is not relieved by nitroglycerin or is accompanied by profuse sweat, shortness of breath, nausea, or vomiting suggests acute myocardial infarction. Long-term population-based studies indicate that approximately 20% of acute myocardial infarctions are clinically unrecognized. It is assumed (although there is no consensus on this issue) that patients with diabetes are more prone to silent myocardial infarction.
Due to the possibility of missing the diagnosis of myocardial infarction, most doctors are quite conservative and hospitalize patients who have any episode suggesting myocardial ischemia ; This is why the sensitivity of clinical tests for acute myocardial infarction reaches 87-98%, but at the same time this means that their specificity is low, and therefore the diagnosis of acute myocardial infarction is confirmed in less than 1/3 of such patients. However, the value of hospitalization in such patients cannot be assessed by these data alone, since they do not include patients with unstable angina, in whom the development of acute myocardial infarction is prevented by hospitalization and aggressive treatment.
Aortic dissection
The incidence of aortic dissection is approximately 1000 times lower than the incidence of myocardial infarction, so, unfortunately, the initial diagnosis of this disease in patients with chest pain is rarely considered. Approximately 80% of patients are hypertensive between the ages of 50 and 70 years. The most common symptom of aortic dissection is the sudden onset of tearing pain in the chest or interscapular area. About 30% of patients have focal or generalized neurological signs .
The incidence of other symptoms and signs varies depending on the location of the dissection: in the ascending and/or descending aorta. Treatment in the acute period requires careful monitoring of blood pressure to prevent further dissection and rupture. After relative normalization of pressure, angiography is recommended to clarify the diagnosis and plan possible surgical intervention.
Pericarditis
Pain from pericarditis is often sharp, persistent and severe, localized behind the sternum and radiating to the back, neck or lower jaw. The pain may increase with each contraction of the heart, movement of the chest or breathing and is relieved by sitting and bending forward. If there is a connection with damage to the pleura (pleuropericarditis), then the pain may be predominantly pleuritic.
The diagnosis of pericarditis is confirmed by the presence of a pericardial friction rub, which can have from one to three components:
- presystolic;
- systolic;
- early diastolic.
However, a pericardial friction rub is heard only periodically. The ECG shows an increase in the ST segment or T wave inversion, depending on the stage of the disease; these changes are best determined on serial ECGs. in the pericardial , but this can only be detected by echocardiography.
Other causes of chest pain
Anginal pain can be caused by hypertrophic cardiomyopathy (idiopathic hypertrophic subaortic stenosis) and aortic valve stenosis, which is presumably associated with insufficient blood supply to the hypertrophied myocardium. Substernal pain can sometimes occur with mitral valve prolapse or mitral stenosis . Nitroglycerin, as a rule, does not help. With pulmonary embolism, the most common symptoms are pleuritic chest pain, as well as:
- dyspnea;
- tachypnea;
- tachycardia.
In some patients, the pain is not pleuritic in nature; a musculoskeletal component is often present. Most patients with documented PE experience the following:
- factors (in history) predisposing to venous thrombosis (immobilization, cancer, obesity, pregnancy, taking contraceptives);
- history of congestive heart failure, venous thrombosis, or pulmonary embolism;
- physical signs of deep vein thrombosis.
There is a significant difference between acute viral idiopathic pleurisy and acute PE; the former disease is usually self-limiting and benign, whereas the latter can be recurrent and fatal. While most patients with PE have some radiographic abnormality , patients with pleurisy have normal chest radiographs, and only 10-15% have pleural effusion. Mediastinitis usually occurs after spontaneous or traumatic rupture (perforation) of the esophagus and is characterized by retrosternal pain, fever, and peripheral blood leukocytosis. An X-ray examination of the chest may reveal widening of the mediastinum or emphysema due to infection with gas-forming microorganisms. Mediastinal emphysema can also result from rupture of pulmonary alveoli or bronchioles, which is most often observed during acute attacks of bronchial asthma . Severe chest pain and mediastinal crackling on auscultation suggest a diagnosis of mediastinitis. Substernal pain can be caused by a variety of diseases of the lungs or pleura. Spontaneous pneumothorax usually involves the sudden onset of acute pleuritic chest pain and shortness of breath, but a small pneumothorax may have few symptoms or signs. Spontaneous pneumomediastinum usually causes severe precordial pain, dyspnea, dysphagia, neck pain, and subcutaneous crepitus.
Mediastinal crackling during auscultation (Hammen's sign) is detected in approximately 50% of cases. Although both spontaneous pneumothorax and pneumomediastinum are often benign and self-limiting. A more liberal approach to obtaining chest radiographs to detect these diseases in small air pockets. Pneumonia or respiratory infection usually presents with a productive cough, fever, shortness of breath, and pleuritic or persistent chest pain. With a sharp exacerbation of obstructive pulmonary disease, the appearance of chest pain is also possible, usually overlapped by the symptom of shortness of breath . If such pain is present, especially in the elderly, an ECG and radiography are performed to exclude myocardial ischemia or pneumothorax.
Pathology of the esophagus
Acute chest pain can be caused by various disorders of the esophagus (observed in combination or in isolation):
- gastroesophageal reflux;
- hiatal hernia;
- achalasia;
- diffuse spasm of the esophagus;
- hypertension in the lower esophageal sphincter;
- nonspecific movement disorders of the esophagus.
When identifying pain of esophageal origin, the following should be noted:
- frequent heartburn;
- symptoms of acid regurgitation (regurgitation);
- odynophagia;
- sensation of a food bolus;
- quick satiety after starting a meal;
- pain that occurs a few minutes after stopping physical activity;
- pain that persists for hours as a background;
- absence of lateral irradiation of pain.
If you have chest pain, you should seek help from a cardiologist, therapist or neurologist. A study of the body will determine the exact cause of pain. Recovery may take from six months to a year.
Digestive diseases
Quite often, a patient’s complaints that he has pain on the right side of the chest can signal problems with the gastrointestinal tract. As a rule, such diseases are accompanied by a number of very characteristic additional symptoms - nausea and vomiting, increased body temperature, and upset stool.
Hepatitis
A dangerous disease that affects the liver develops as a result of transfusion of infected blood into the human body (forms B and C), and is also transmitted through dirty hands (form A). A characteristic symptom of hepatitis is not only pain, but also yellowing of the whites of the eyes, associated with an increase in the amount of bilirubin in the blood.
Stomach ulcer
It may appear as the body’s response to the abuse of spicy, fatty and fried foods, as well as alcohol. Often, peptic ulcer disease is preceded by other gastrointestinal lesions. The pathology is characterized by the formation of a perforation in the wall of the stomach, through which its contents enter the abdominal cavity. As a rule, with an ulcer, the patient complains that the pain is most intense on the right side (including in the chest) during or after eating.
Pancreatitis
Pancreatitis (inflammation of the pancreas) in our country is not treated very responsibly, believing that it is enough to relieve pain symptoms. In fact, such a careless attitude towards the disease can lead to a number of more serious problems that will require urgent surgical intervention.
Methods for diagnosing intercostal neuralgia
If you suspect intercostal neuralgia, you should consult a neurologist.
In most cases, the diagnosis is established based on the patient’s complaints, medical history and examination of the patient directly at the appointment. The doctor pays attention to the patient’s posture: in an effort to reduce pain by reducing pressure on the affected nerve, the patient tilts the body in the opposite direction. The intercostal spaces are palpated in the area where the pain is located. Loss of sensitivity and blanching of the skin is established.
Sometimes instrumental and laboratory diagnostics may be required:
ECG
An ECG is performed in case of pain on the left side. The goal is to rule out heart problems. In combination with an ECG, echocardiography (ultrasound of the heart) may be prescribed. More information about the diagnostic method
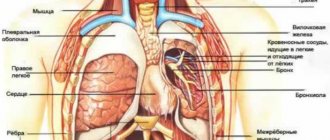
Chest X-ray
A chest x-ray is performed to exclude diseases of the lungs and pleura.
More information about the diagnostic method
Ultrasound of the abdominal organs
A survey ultrasound examination can exclude diseases of the abdominal organs.
More information about the diagnostic method
Neuromyography
Electroneurography is prescribed, as a rule, if the traumatic nature of intercostal neuralgia is suspected.
X-ray of the spine
X-ray of the thoracic spine allows us to determine the causes of radicular syndrome. A CT scan or MRI may also be ordered to evaluate the condition of the spine.
More information about the diagnostic method
Blood test for antibodies to the herpes virus
It is carried out if there is a suspicion of a viral origin of intercostal neuralgia.
Sign up for diagnostics To accurately diagnose the disease, make an appointment with specialists from the Family Doctor network.
Spinal problems
The back is also often able to “give” under the ribs or into the chest. This occurs if there is an injury, sprain after intense physical activity, and as the main concomitant symptom of some pathological conditions.
Intercostal neuralgia
This term refers to compression of the roots of the intercostal nerves. As a result, the latter become irritated and respond with intense pain in the chest on the right or left, often radiating under the shoulder blade.
Intervertebral hernia
This is a musculoskeletal disease in which there is a gradual thinning of the wall of the fibrous ring and, as a result, its rupture.
Scoliosis
The “sickness” that our parents and school teachers used to scare us as children is not as harmless as it might seem. Deforming over time, the spine often produces more or less intense pain and various pathologies.
Ankylosing spondylitis
A situation in which pain in the back and/or chest on the right is a frequent companion to this pathology, manifested by inflammation of the intervertebral joints. The disease is chronic, limits joint mobility, stunts growth and ultimately leads to disability.
Causes of intercostal neuralgia
All causes of intercostal neuralgia can be reduced either to a pinched nerve root (the nerve is compressed at the point of exit from the spinal canal) or to irritation or compression of a nerve already in the intercostal space.
Intercostal nerve radicular syndrome is usually caused by one of the following:
- osteochondrosis of the thoracic spine;
- intervertebral hernia;
- tumor processes;
- other diseases of the spine.
Much more often, intercostal neuralgia occurs as a result of factors affecting the nerve in the intercostal space. The main reasons here are:
- chest injuries;
- herpes infection (herpes zoster);
- muscular-tonic syndrome due to excessive physical activity or working in an awkward position;
- hypothermia;
- for women - wearing tight underwear (bra). First of all, those who have a poorly developed subcutaneous fat layer should be careful;
- compression of the nerve by a growing tumor (pleura, chest wall) or an aneurysm of the descending thoracic aorta;
- factors affecting the entire nervous system (poisoning, hypovitaminosis).
Factors that increase the risk of intercostal neuralgia are:
- diabetes;
- problems with immunity;
- age-related changes in blood vessels;
- alcoholism;
- hormonal disorders;
- stress, depressed mental state;
- long-term use of potent medications.
Treatment
It can be conservative or surgical, depending on the diagnosis. Some types of pathologies - for example, hepatitis - require long-term use of antibiotics and strong antiviral drugs, others are based on normalizing the diet and maintaining a healthy lifestyle. The specialists of the Energo clinic, who are true professionals in their field, will definitely identify the causes of back and chest pain, select a method that is suitable for you to solve the problem, and give useful recommendations regarding the period of recovery or remission in the case of a chronic illness.
What to do?
The first rule when detecting pain is not to make a diagnosis yourself. If there is pressure, what to do:
- In case of prolonged or acute sensations, call an ambulance.
- While waiting for doctors, lie down with a bolster or pillow under your head.
- Loosen clothing and provide oxygen access.
- If you suspect that the sensations are due to heart disease, take a nitroglycerin tablet.
It is strictly forbidden to leave the patient unattended. If the situation is not critical, then you need to visit a doctor yourself as soon as possible.