Chest pain is a very common symptom that causes great concern. After all, we all know that this is how diseases of the cardiovascular system manifest themselves. But in reality, this symptom may indicate other disorders in the body, in particular pathologies of the gastrointestinal tract, respiratory system and even the spine. In any case, such a sign cannot be ignored, especially with acute pain, since extremely dangerous conditions, for example, pulmonary embolism and myocardial infarction, can manifest themselves in this way. With them, the patient’s life directly depends on the urgency of providing qualified medical care. Let's look at the main causes of chest pain and their distinctive signs.
Diseases of the cardiovascular system
Pathologies of the heart and blood vessels still remain among the most common, which is largely due to the lifestyle of modern people. The most common causes of chest pain are:
- angina pectoris;
- myocardial infarction;
- pericarditis.
Angina pectoris
Angina pectoris is one of the clinical forms of coronary heart disease (CHD). It is a consequence of a decrease in the amount of oxygen entering the heart muscle (myocardium) due to impaired blood flow in the arteries (ischemia). This may be the result of the development of atherosclerosis of the coronary arteries, which leads to a decrease in their lumen, spasm of blood vessels or thrombosis and other disorders. The consequence in all cases is a deficiency of oxygen in the myocardium, which provokes the occurrence of characteristic symptoms:
- dull, pressing or pulling pain behind the sternum (sometimes it is localized in the region of the heart), tending to radiate to the left shoulder and the inner surface of the left arm, less often to the neck, right arm and stomach and passes when physical activity stops and the transition to a calm state, so attacks usually last less than 5 minutes;
- dyspnea;
- increased diastolic (lower) blood pressure.
A distinctive sign of angina pectoris is the occurrence of an attack during physical activity, transition from heat to cold, especially in strong winds. But the most pathognomonic symptom is the rapid elimination of pain after taking nitroglycerin.
Myocardial infarction
Myocardial infarction is a condition that requires emergency medical attention. It is a consequence of the progression of coronary artery disease, and in some cases the disease begins with it. This is a severe complication of myocardial ischemia, in which foci of necrosis, i.e., tissue death, form in it. This most often results from rupture of an atherosclerotic plaque. This triggers a whole chain of changes, the result of which is occlusion (blocking) of the coronary artery, which leads to the cessation of nutrition of the corresponding section of the myocardium and the development of ischemic necrosis.
Myocardial infarction is accompanied by severe, excruciating pain behind the sternum, which in nature can be either pressing, bursting or squeezing, or burning, stabbing, or felt like a blow to the heart. It is in many ways similar to an attack of angina, but is much stronger and more often accompanied by a fear of death. The pain is localized in the area behind the sternum and usually spreads to the left, less often it covers the entire surface of the chest and radiates to the stomach, reminiscent of appendicitis, exacerbation of gastric ulcer, etc.
Pain during myocardial infarction radiates to the left shoulder, forearm, hand, and more often it radiates to the little finger and ring finger. They can also radiate to the right hand or to the stomach area, under the shoulder blades, the left side of the neck, jaw, or ear.
The attack can last 15-30 minutes, but more often it drags on for several hours up to 24 hours. In addition to chest pain, this may be accompanied by:
- decreased blood pressure;
- nausea, vomiting;
- shortness of breath;
- severe weakness, combined with increased emotional arousal due to fear of death;
- dizziness;
- cold sweat;
- feeling of heartbeat;
- headache;
- pallor, marbling of the skin;
- tremor.
Shortly before the onset of pain, the following may be observed:
- varying degrees of chest discomfort or pain, as with angina pectoris, but occurring against the background of complete calm or with little physical activity;
- dyspnea;
- weakness;
- dizziness.
Myocardial infarction differs from an attack of angina pectoris in the severity of pain and the duration of its persistence. Also, during a heart attack, taking nitroglycerin leads to only a slight improvement or has no effect at all.
Pericarditis
Pericarditis is a disease accompanied by inflammation of the pericardial sac. Most often, its development is caused by concomitant disorders (viral, bacterial, fungal infections, in particular tuberculosis and borreliosis, as well as metastatic lesions, metabolic disorders), although it can also be a consequence of exposure to ionizing radiation, trauma, or occur in the absence of visible signs. causes (idiopathic pericarditis).
There are acute and chronic pericarditis. In the first case, the following are observed:
- pressing pain in the chest in the area of the heart of varying degrees of intensity, sometimes radiating to the left arm;
- increased pain when taking a deep breath, coughing and swallowing;
- reduction of pain when taking a sitting position, slightly leaning forward, and intensification in a supine position.
With chronic pericarditis, moderate chest pain and shortness of breath are observed. Often, patients previously noticed an increase in body temperature, weakness, muscle discomfort and other typical symptoms of infectious diseases.
With pericarditis, pain is relatively constant, and its severity increases gradually. Taking nitroglycerin does not eliminate the ailment, although NSAIDs (ibuprofen and others) help improve well-being.
Chest pain: what to do?
If pain grips a person’s chest and it becomes difficult to breathe, you should immediately go to the hospital, even if the symptoms are mild and go away on their own. The causes of unpleasant sensations can be different, and they can only be determined with the help of special studies. It is especially important to consult a doctor in cases where the patient has hit his chest, or symptoms have arisen for no apparent reason, but are abrupt and severe. Such situations can pose a danger to a person’s life, and the sooner appropriate measures are taken, the greater the chance of a full recovery.
Gastrointestinal pathologies
Diseases of the gastrointestinal tract, or more precisely the esophagus, can also provoke the appearance of chest pain. In such cases, they often radiate to the back, to the right and left of the sternum, and in most cases they are associated with food intake and are associated with swallowing disorders.
Swallowing problems are called dysphagia.
Most often, patients with complaints of chest pain are diagnosed with:
- esophageal diverticulum;
- gastroesophageal reflux disease (GERD);
- hiatal hernia;
- spasm of the esophagus (esophagospasm).
Esophageal diverticulum
A diverticulum of the esophagus is a protrusion of its wall with the formation of a kind of “pocket” in which food accumulates. Clinical manifestations of the disease usually occur when the size of the diverticulum is more than 2 cm. In such cases, periodic pain in the sternum and back is observed, as well as regurgitation of chewed food. Sometimes the body temperature also rises to subfebrile levels.
GERD
GERD is a chronic disease accompanied by the reflux of stomach contents into the esophagus, and in some cases, the contents of the duodenum. This causes irritation of the mucous membrane and its inflammation.
With GERD, chest pain is localized in the center and left, which often causes concern in patients. In some cases, they spread to other parts of the sternum. The intensity of pain can vary from mild discomfort to quite severe pain. Their appearance is associated with food, but sometimes they also occur after smoking, and some patients complain of chest pain when they lie down, including at night.
Also with GERD the following may be observed:
- heartburn that occurs when the body bends forward or in a lying position;
- belching of air or food;
- feeling of heaviness, bloating;
- fast saturation;
- dysphagia or pain when swallowing.
A characteristic feature of GERD is the onset of all symptoms directly during or immediately after eating. Also a pathognomonic manifestation is improvement in well-being after taking antacids and changing body position to vertical and walking.
Hiatal hernia
A hiatal hernia means a displacement into the chest cavity of those anatomical structures that should normally be located underneath it, in particular the abdominal segment of the esophagus, the cardia of the stomach, or even intestinal loops. With age, the risk of developing pathology progressively increases; as a result, it is found in 69% of people over 70 years of age.
A diaphragmatic hernia is not always accompanied by chest pain. In fact, very often it is asymptomatic and is discovered by chance during an examination regarding complaints of other disorders of the gastrointestinal tract. But in about 50% of cases, a hiatal hernia leads to pain in the central abdomen just below the ribs, spreading along the esophagus or radiating to the area between the shoulder blades and the back. Less often, they are encircling in nature or localized only behind the sternum, thereby resembling the clinical picture of pancreatitis or angina pectoris, myocardial infarction.
Another symptom of the disease may be heart rhythm disturbances. This leads to fairly frequent diagnostic errors, and therefore the prescription of treatment that does not lead to improvement. To avoid this, it is important to trace the conditions for the onset of pain. The presence of a diaphragmatic hernia is indicated by:
- the appearance of pain after eating, during physical activity, coughing and lying down;
- reduction or complete disappearance of discomfort after belching, taking a deep breath, changing body position, or after the patient drinks a glass of water;
- increased pain when bending forward;
- the occurrence of swallowing disorders, especially when consuming liquid and puree foods, very cold or, conversely, very hot drinks, as well as when rushing while eating.
A hernia is dangerous due to strangulation. In this case, severe cramping pain occurs in the chest, radiating to the back. This is accompanied by nausea, vomiting, often with blood, as well as increased heart rate, decreased blood pressure and shortness of breath.
Also, the disease is often complicated by the development of GERD. Therefore, the characteristic signs of reflux are subsequently added to the existing symptoms.
Esophagospasm
The spasm occurs at the junction of the esophagus and the stomach. This is accompanied by symptoms very similar to those of angina pectoris. The pain can be quite severe. They are localized in the heart area, but can radiate to the neck, lower jaw and shoulders, but unlike angina, they appear during meals and can persist not only for several minutes, but also for hours. This is accompanied by dysphagia and a feeling of difficulty passing food, which can quickly subside after drinking warm drinks, in particular tea or water.
Esophagospasm has a reflex origin and usually accompanies other diseases of the gastrointestinal tract, including GERD, peptic ulcer of the stomach and duodenum, hiatal hernia, cholecystitis, etc.
But esophagospasm can be relieved by taking nitroglycerin, since the esophagus is also formed by smooth muscle fibers.
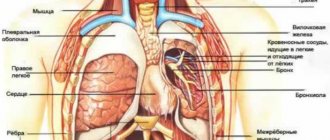
Diseases of the respiratory system
Pathologies of the pleura and pleural cavity, as well as the lungs themselves, can provoke pain in the chest. A distinctive feature of these diseases is the presence of a connection between pain and breathing: it increases with inhalation and decreases with exhalation. This causes an involuntary decrease in breathing rate - it becomes frequent and superficial. Most often, chest pain in such situations is caused by pneumonia, pleurisy, pleural empyema and tumors of the bronchopulmonary localization and pleura.
Pneumonia
Pneumonia is inflammation of the lungs that occurs as a result of damage to the lung tissue by a variety of bacteria, viruses or fungi. Most often, it is a consequence of acute respiratory infections, including infection with a new strain of coronavirus, which is accompanied by a deterioration in the patient’s condition after a temporary improvement.
As a result, pneumonia has typical symptoms characteristic of most respiratory infections:
- rapid increase in body temperature to 38 °C and above;
- chills;
- headache;
- decreased appetite;
- cough is initially dry, and then with sputum, less often hemoptysis;
- dyspnea;
- superficial or deep pain in the chest, which tends to intensify with coughing and breathing;
- muscle weakness, joint discomfort;
- general weakness, depression.
Today, diagnosing pneumonia is not difficult and is usually detected during the initial examination of the patient.
Pleurisy
Pleurisy is inflammation of the pleural layers covering the surface of the lungs and chest wall. This is accompanied by the formation of fibrinous deposits or the accumulation of liquid exudate in the cavity formed by two layers of the pleura. This may be a consequence of an infectious lung infection, in particular tuberculosis, although it also occurs with bacterial, viral and fungal infections of other origins. Also, pleurisy can develop against the background of rheumatism, after myocardial infarction, as well as with gastrointestinal pathologies and in some other cases.
There are dry and exudative pleurisy, and the second form is often a consequence of untimely treatment of dry pleurisy. In such cases the following are observed:
- intermittent chest pain, aggravated by deep breathing, coughing, swallowing, and in some cases, by tilting the body in the opposite direction;
- pain radiating to the stomach, shoulder;
- severe, prolonged hiccups;
- lag of the affected half of the chest when breathing;
- dry cough;
- dyspnea;
- weakness, decreased performance;
- increase in body temperature to subfebrile values;
With pleurisy, there is often a friction noise between the layers of the pleura, which resembles the creaking of snow underfoot. Moreover, if you place your palm on your chest, you can feel their friction.
With exudative pleurisy, pain is present at the beginning of the development of the disease and at the end. But after a sufficient volume of exudate accumulates in the pleural cavity, they disappear. The remaining symptoms are generally similar to those of dry pleurisy.
Empyema of the pleura
Pleural empyema, in fact, is one of the variants of the course of pleurisy, but unlike other forms, it is characterized by the accumulation of pus in the pleural cavity. It can be a consequence of pneumonia (pneumonia), the formation of tumors, cysts, bronchiectasis and other disorders of the lungs, less often in the abdominal organs.
The pathology is characterized by:
- chest pain;
- dyspnea;
- fever;
- chills;
- decreased appetite;
- forced position of the body (lying on the sore side).
The development of pleural empyema requires hospitalization in the surgical department.
Tumors of the lungs and pleura
There are many types of benign and malignant neoplasms that can affect the lungs, bronchi and pleura. They are often accompanied by recurrent pleurisy with constantly increasing pain on the affected side. But direct chest pain caused by a neoplasm, especially a malignant one, occurs after it reaches a large size. This significantly worsens the prognosis, although today there are methods for treating even large tumors that were previously considered inoperable.
Spine pathologies
When chest pain appears, it is difficult to immediately suspect its cause in the development of spinal diseases. Nevertheless, osteochondrosis of the thoracic region and intercostal neuralgia can also make themselves felt in a similar way.
Osteochondrosis of the thoracic spine
Osteochondrosis is the process of dehydration of intervertebral discs and the occurrence of degenerative changes in them. Damage to the thoracic region is much less common than to the cervical or lumbar, and the symptoms are largely reminiscent of angina pectoris and gastrointestinal pathologies. Therefore, patients are often falsely diagnosed with other diseases, and treatment that does not bring results is prescribed.
The risk of developing osteochondrosis directly depends on lifestyle. Therefore, if previously it was mainly found in older people, today it is often detected in young people. Prolonged, regular sitting increases the likelihood of dehydration and progressive degeneration of the discs in the thoracic spine. Therefore, it is most often diagnosed in people who are forced to sit for a long time at a computer, behind the wheel of a car, at a machine, etc.
Osteochondrosis of the thoracic region can manifest itself:
- constant dull pain between the shoulder blades;
- girdle pain localized at the level of the armpits;
- pain in the heart and behind the sternum;
- burning sensation in the back.
A characteristic feature is the occurrence of painful sensations after prolonged sitting, at the end of the working day.
The main danger of osteochondrosis is its steady progression, especially in the absence of comprehensive treatment. As a result, over time, the affected disc, which is a dense cartilage with a jelly-like internal content, becomes deformed and bulges, usually towards the spinal canal. This is called protrusion. Subsequently, it can transform into an intervertebral hernia, which means the final rupture of the outer dense ring of the disc, through which the jelly-like internal contents (nucleus pulposus) can exit into the spinal canal. This is dangerous due to the infringement of the spinal roots passing here and even the spinal cord itself, which will lead to disruptions in the functioning of the internal organs innervated by them, shooting pains, numbness and other sensitivity disorders.
Intercostal neuralgia
Intercostal neuralgia is a consequence of damage to the peripheral nerves passing through the tissues in the area of the intercostal spaces. This may be due to their mechanical compression, herpetic infection, hypothermia, exposure to toxic substances, injuries and other factors.
With intercostal neuralgia, the pain is lumbago-like or burning. They spread along the ribs to the sternum. They can be either short-term or last for hours or even days. When touching the skin in the intercostal spaces, changing body position, walking, deep breathing, coughing, the pain intensifies.
What to do, what examinations need to be completed
Basic methods of investigating the causes of chest pain, including a thorough history and physical examination, provide 90% of success towards the correct diagnosis.
Increased body temperature, accompanying a feeling of tightness, is common with pneumonia, acute myocardial infarction, pericarditis, and herpes zoster. Pain in the chest along with weakening of the pulse is characteristic of dissection of the aorta or aneurysm.
Enlarged jugular veins occur in congestive heart failure, sometimes occurring as a complication of an inferior heart attack or pulmonary embolism, when the blockage accounts for more than 60% of the blood supply to the lung.
Pain in the middle of the chest, palpable on palpation, indicates a musculoskeletal cause. Unilateral discomfort in the thoracic region is a sign of damage to one or more adjacent ones involving the spinal or peripheral nerve (herpes zoster).
Auscultation, in which the doctor listens to the chest, is an important part of the physical examination. Auscultation findings:
- weak one-sided breathing, in which pressure on the chest, raises suspicion of pneumothorax, local attacks of auditory detection - effusion;
- tubular breathing is heard over the inflamed area, sometimes over the effusion;
- limited areas with audible crepitus in the chest are present with prolonged lobar pneumonia, enlarged areas accompanied by pain in the heart indicate either multilobar inflammation or pulmonary edema due to left ventricular failure after acute myocardial infarction (or heart failure);
- with pericarditis and pleurisy, a rustling sound occurs (pericardial sounds are heard only when you hold your breath).
The main tests aimed at determining the cause of discomfort behind the sternum in the middle include a blood test. With pneumonia, leukocytosis is detected (changes in the cellular composition of the blood), which may be present to a lesser extent in acute myocardial infarction. Cardiac-specific markers increase within 6 hours after myocardial infarction.
Chest examinations that reveal pathologies that accompany pressing pain in the sternum:
| Diagnostic measures. | What is expected during the examination. |
| History, physical examination. | Musculoskeletal and skin diseases. |
| ECG, O2 saturation. | Cardiac arrhythmia, myocardial infarction, pulmonary embolism, hypoxic diseases. |
| Elevated troponin T. | Acute myocardial infarction, myocardial necrosis of another etiology. |
| D-dimer. | Rule out pulmonary embolism. |
| X-ray. | Pneumonia, pneumothorax, damage to the ribs and vertebrae. |
| Echocardiography. | Aortic dissection, delayed pulmonary embolism, delayed acute myocardial infarction, aortic stenosis. |
| CT, angio computed tomography | Pulmonary embolism, aortic dissection, pneumothorax, pneumonia, pleural disease, rib injury. |
| Stress tests, coronary angiography, gastroscopy, psychiatric examinations | Other causes (for example: cardiac neurosis, cardiac phobia) |
Tactics for determining the cause of chest pain
When discomfort or chest pain occurs, patients often initially turn to a therapist, which is very rational. At the appointment, the doctor initially finds out the nature of the complaints. Much attention is paid to:
- localization of pain (left, right, center or girdling, deep or superficial);
- intensity (the severity of painful sensations is not always equivalent to the existing threat);
- character (squeezing, pressing, dull, aching, stabbing, shooting, etc.);
- conditions of occurrence (during physical activity, eating, transition from heat to cold, at rest, when taking a horizontal position, etc.);
- conditions of termination (after rest, when walking, after eating, drinking, drinking nitroglycerin, when lying on the sick or healthy side, after belching, vomiting);
- duration;
- accompanying symptoms;
- irradiation (in the left arm, neck, jaw, between the shoulder blades, in the stomach, etc.);
- the duration of the pain.
The doctor must find out whether there have been recent injuries to the chest or spine. Mention of such episodes makes it possible to simplify diagnosis and quickly determine the cause of chest pain.
Physical examination
The second stage of diagnosis is a physical examination. It involves sequential execution:
- examination of the skin and mucous membranes for rashes, color changes, and signs of cyanosis;
- assessment of pulse in the radial and femoral arteries;
- blood pressure measurements;
- palpation of the chest, muscles, spinous processes of the vertebrae, identifying symptoms of radicular syndrome;
- percussion (tapping) of the chest;
- auscultation of the heart and lungs (heart sounds are assessed, murmurs, wheezing in the lungs, the sound of pleural friction are detected);
- palpation of the abdomen;
- examination of the lower extremities for signs of varicose veins, thrombophlebitis.
The suspected cause of pain can be detected at any stage of the examination. As a result, the patient receives an appointment for laboratory and instrumental diagnostics.
Diagnostics
A comprehensive examination begins with a general practitioner or family doctor. The specialist conducts a physical examination and identifies the leading pathological syndrome, and if necessary, sends the patient for consultation with specialized specialists (pulmonologist, cardiologist). To establish a diagnosis, the results of instrumental and laboratory tests are necessary, of which the following are most often prescribed:
- X-ray of the OGK.
Radiation diagnostics helps to differentiate cardiac and pulmonary pathology. Damage to the respiratory system is manifested by focal infiltrates, rounded shadows, and increased vascular pattern. Signs of cardiac problems are changes in the size and configuration of the heart shadow, congestion in the lungs. - Electrocardiography.
An ECG evaluates the electrical activity of the myocardium. The cardiogram reveals a decrease in the voltage of the waves or their inversion, deviation of the heart axis, and signs of disturbances in the myocardial conduction system. Daily ECG monitoring and bicycle ergometer test are of great diagnostic value. - Echocardiography.
Ultrasound diagnostics shows structural and functional abnormalities in the activity of the heart. The method is necessary for diagnosing pericarditis (effusion in the heart sac), cardiomyopathy (expansion of cavities or thickening of the walls of the organ). EchoCG allows you to measure the contractile function of the left ventricular myocardium. - Invasive methods.
In case of pathological processes in the pericardium, a diagnostic puncture is performed for bacteriological and cytological examination of the exudate. In case of coronary artery disease, coronary angiography is performed to assess the extent of vascular damage. The functional state of the myocardium is determined by perfusion scintigraphy. - Laboratory diagnostics.
Analyzes are of auxiliary value. In case of cardiac pathology, an extended biochemical study is indicated with determination of the lipid spectrum and acute phase parameters, measurement of myocardial markers. Diagnosis of pulmonary diseases requires microscopy and sputum culture.
Echocardiography