The article was checked by the Head of the IVF Department, a reproductive specialist, a gynecologist-endocrinologist Kuranosova I.Yu., is for general informational purposes only and does not replace specialist advice. For recommendations on diagnosis and treatment, consultation with a doctor is necessary.
Specialists at the Yauza Clinical Hospital diagnose and treat diabetes in pregnant women and its complications. For a comfortable pregnancy and the safety of the expectant mother and baby, we strictly monitor the blood sugar level of a pregnant woman and, if necessary, prescribe a specially designed diet and medications.
Make an appointment with a gynecologist
- About 7% of pregnant women have manifestations of gestational diabetes mellitus. In 50% of cases the disease is asymptomatic
- Gestational diabetes in pregnant women significantly increases the risk of pregnancy complications for both mother and fetus
- Perinatal mortality increases by 2-3% when diabetes mellitus and pregnancy are combined
Diabetes in pregnancy (gestational diabetes) is an increase in blood glucose levels that first occurs during pregnancy, but does not reach a level sufficient to make a diagnosis of diabetes mellitus. These are hidden disorders of carbohydrate metabolism that threaten to develop into diabetes.
Normal blood glucose level in a pregnant woman
During pregnancy, all women experience changes in insulin sensitivity and glucose tolerance. This is fine. The difference between normal and pathological is the degree of change.
Blood tests for diabetes during pregnancy - norm and pathology
- If a study of venous blood taken on an empty stomach shows a glucose level of more than 5.1 mmol/l, this is normal for pregnant women.
- From 5.1 to 7.0 mmol/l – gestational diabetes.
- If 7.0 mmol/l or more – diabetes mellitus.
- Testing capillary blood (taken from a finger) to diagnose gestational diabetes mellitus is not recommended.
- If during an oral glucose tolerance test (when 75 g of glucose is taken orally during the test), after an hour the glucose level is more than 10.0 mmol/l, and after two hours the blood glucose level is in the range of 7.8-8.5 mmol/l – then this is a normal indicator for pregnant women.
To better understand what gestational diabetes, or pregnancy diabetes, is, you need to talk a little about hormonal changes in the body in pregnant women.
DEFINITION OF DIABETES MELLITUS AND ITS CLASSIFICATION
Diabetes mellitus is a group of metabolic diseases characterized by hyperglycemia, which results from defects in insulin secretion, insulin action, or both (WHO, 1999)
CLASSIFICATION OF DIABETES MELLITUS
(WHO, 1999)
SD type | Characteristics of diseases |
| Diabetes mellitus type 1 • Autoimmune • Idiopathic | Destruction of $-cells of the pancreas, usually leading to absolute insulin deficiency |
| Diabetes mellitus type 2 | With predominant insulin resistance and relative insulin deficiency or a predominant defect in insulin secretion with or without insulin resistance |
| Gestational diabetes mellitus | Occurs during pregnancy |
| Other types of diabetes* | • Genetic defects of function β-cells • Genetic defects in insulin action • Diseases of the exocrine pancreas • Endocrinopathies • Drug or chemical induced diabetes • Diabetes induced by infections • Uncommon forms of immune-mediated diabetes • Other genetic syndromes associated with diabetes mellitus |
Chronic complications of diabetes include vascular complications (micro- and macroangiopathies) and neuropathies.
Diabetic microangiopathies include:
Diabetic retinopathy (DR) is a microangiopathy of the retinal vessels in diabetes mellitus, which in the terminal stage leads to complete loss of vision.
Diabetic nephropathy (DN) is a specific damage to the renal vessels in diabetes mellitus, accompanied by the formation of nodular or diffuse glomerulosclerosis, the terminal stage of which is characterized by the development of chronic renal failure (CRF).
Diabetic macroangiopathies include:
- coronary heart disease and heart failure (as a complication of coronary artery disease);
- cerebrovascular diseases;
- peripheral angiopathy.
Diabetic neuropathy is damage to the nervous system caused by diabetes.
Emergency conditions for diabetes
Uncontrolled hyperglycemia can lead to ketoacidotic coma (more often in type 1 diabetes) or hyperosmolar coma (more often in type 2 diabetes). These life-threatening conditions require a complex of emergency treatment measures.
- Ketoacidotic coma
- Hypoglycemic coma
- Hyperosmolar coma
- Hyperlactic acidemic coma
DIAGNOSIS OF DIABETES MELLITUS
Diagnostic criteria for diabetes and other disorders of carbohydrate metabolism (WHO, 1999)
| GLUCOSE CONCENTRATION, mmol/L (MG/%) | |||
| Whole blood | Plasma | ||
| Venous | Capillary | Venous | |
| NORM | |||
| On an empty stomach and 2 hours after TSH | 3,3-5,5 (59-99) | 3,3-5,5 (59-99) | 4,0-6,1 (72-110) |
| <6,7 (<120) | <7,8(<140) | <7,8(<140) | |
| DIABETES | |||
| On an empty stomach or 2 hours after TSH or 2 hours after a meal (postprandial glycemia) or random determination of glycemia at any time of the day, regardless of meal time | ≥6,1 (≥110) | ≥6,1 (≥110) | ≥7,0 (≥126) |
| ≥10,0 (≥180) | ≥11,1 (≥200) | ≥11,1 (≥200) | |
| ≥10,0 (≥180) | ≥11,1 (≥200) | ≥11,1 (≥200) | |
| IMPAIRED GLUCOSE TOLERANCE | |||
| On an empty stomach (if determined) and 2 hours after TSH | <6,1 (<110) | <6,1 (<110) | <7,0(<126) |
| 6,7-10,0 (120-180) | 7,8-11,1 (140-200) | 7,8-11,1 (140-200) | |
| On an empty stomach and after 2 hours (if determined) | IMPAIRED FASTING GLYCEMIA | ||
| ≥5,6 (≥100) <6,1 (<110) | ≥5,6 (≥100) <6,1 (<110) | ≥6,1 (≥110) <7,0 (<126) | |
| <6,7 (<120) | <7,8(<140) | <7,8(<140) | |
Fasting glucose refers to the blood glucose level in the morning before breakfast after a prior fast of ≥8 hours.
Postprandial glycemia is the blood glucose level 2 hours after a meal.
Glycated hemoglobin (HbAl c) - This indicator allows you to evaluate the average level of glycemia over 1.5-2 months [2,8,17]. Under physiological conditions, its level is 3-6%.
Pump insulin therapy. The device currently in use is a continuous glucose monitoring device, which is a device the size of a pager (pump). It is equipped with a subcutaneous sensor that calculates glucose levels every 5 minutes, recording up to 288 glucose values per day. The device can be used in patients with various types of diabetes in outpatient and inpatient settings[2,8,9].
Gestational diabetes mellitus (GDM) is an impairment of glucose tolerance of varying severity that occurs during pregnancy. In a five-year, blinded, randomized study, Hyperglicemia and adverse pregnancy outcomes (HAPO) examined 25,505 pregnant women of different ethnic groups. In 15 largest centers in nine countries, they underwent PTG with 75 g of glucose at 24-32 weeks of pregnancy. The study results demonstrated a strong relationship between maternal hyperglycemia and neonatal outcomes. In 2010, the International Association of Diabetes and Pregnancy Study Groups (IADPSG), based on the HAPO study, proposed new criteria for the diagnosis of GDM. Currently, the diagnosis of “impaired glucose tolerance” is not used during pregnancy. Any disorder of carbohydrate metabolism that first appeared or was identified during pregnancy is defined as
Manifestations of GDM are usually hidden and can be detected in risk groups after a glucose tolerance test (TSG).
Risk groups for developing GDM:
| OPTIONS | HIGH RISK | MODERATE RISK | LOW RISK |
| Overweight (>20% of ideal) | Yes | Yes | No |
| Type 2 diabetes in close relatives | Yes | No | No |
| History of GDM | Yes | No | No |
| Impaired glucose tolerance | Yes | No | No |
| Glucosuria during previous or current pregnancy | Yes | Not really | No |
| History of hydramnios and large fetus | Not really | Yes | No |
| Birth of a child weighing more than 4000 g or a history of birth control | Not really | Yes | No |
| Rapid weight gain during this pregnancy | Not really | Yes | No |
| Woman's age over 30 | Not really | Yes | <30 years |
Glucose tolerance test procedure
To diagnose GDM, a glucose tolerance test (TGT) is used, which is performed against the background of a normal diet without restriction of carbohydrates. The study is carried out on an empty stomach, no earlier than 10 hours after the last meal. After determining the fasting blood glucose level, the patient is asked to drink a solution with 75 g of glucose. During TSH, a pregnant woman should refrain from physical activity, eating, and smoking. Next, the glucose level is determined 1 hour and 2 hours after the glucose load.
Diagnosis and screening of GDM
Criteria for identifying GDM based on TSH
| Load | On an empty stomach | After 1 hour | After 2 hours | After 3 hours |
| 50 g glucose | >5.3 mmol/l | >7.8 mmol/l | – | – |
| 100 g glucose | >5.3 mmol/l | > 10.0 mmol/l | >8.6 mmol/l | >7.8 mmol/l |
GDM is diagnosed if the normal level is exceeded by at least 2 of the given indicators for OPT with 100 g of glucose. If only 1 of them is exceeded, the test is repeated after 2 weeks.
Hormonal and metabolic changes during pregnancy in patients with diabetes
Physiological pregnancy in the early stages is accompanied by increased glucose utilization and an increase in the amount of adipose tissue in the mother’s body. The main hormonal and metabolic changes during pregnancy are associated with the formation of a new endocrine organ - the placenta, which secretes protein and steroid hormones (chorionic gonadotropin, placental lactogen, progesterone, estrogens). The hormonal function of the placenta is associated with the mobilization of fat from the depot and a decrease in the utilization of glucose by insulin-sensitive tissues. Developing insulin resistance contributes to an increased use of lipid metabolism products, while glucose is saved to feed the fetus, for which it is the main source of energy. During pregnancy, fasting blood glucose levels decrease. Glucose and ketone bodies easily pass through the placental barrier. Insulin does not cross the placental barrier. Hyperglycemia in the mother promotes increased transfer of glucose across the placenta and causes hyperplasia of β-cells of the pancreatic islets in the fetus, hyperinsulinemia and, as a consequence, fetal macrosomia.
Due to increased glucose utilization in early pregnancy, a decrease in insulin requirements is observed, reaching minimum values at 9-11 weeks of pregnancy (89.3% of the initial level). In order to adequately and timely reduce insulin doses, it is necessary to determine blood glucose levels more often (6-8 times a day). With the onset of the second half of pregnancy and the development of insulin resistance, the need for insulin gradually increases, reaching maximum values at 32-33 weeks (140-160% of the original).
From the 35th week of pregnancy, there is a gradual decrease in the need for insulin with a sharp decrease towards childbirth to 80-75% of the initial level. A decrease in insulin requirements may begin earlier in cases of severe placental insufficiency (PI, which is often found in patients with vascular complications of diabetes and may require early delivery). Insulin requirements remain low during the first two days of the postpartum period. Starting from the 3rd day of the postpartum period, the need for insulin begins to increase and quickly reaches the initial level.
The effect of pregnancy on vascular complications of diabetes depends on the degree of diabetes compensation before and during pregnancy, the severity of diabetes complications before pregnancy, and the addition of preeclampsia. A third of patients experience transient worsening of retinopathy and nephropathy with unsatisfactory compensation of diabetes.
Management of pregnancy in patients with diabetes mellitus
Management of pregnancy during diabetes requires clear definition of goals:
- Achieving normoglycemia
- Preventing the development of complications
- Stabilization of existing complications
- Maintaining pregnancy to term (minimum 38 weeks)
- Preventing obstetric complications:
preeclampsia
polyhydramnios
urinary tract infections
To successfully achieve your goals, a team approach of specialists in the management of pregnant women and patients with diabetes is necessary:
- Endocrinologist
- Obstetrician-gynecologist
- Neonatologist
- Ophthalmologist
Absolute contraindications for prolonging pregnancy in diabetes mellitus are::
- severe nephropathy with creatinine clearance less than 50 ml/min, daily proteinuria 3.0 g or more, blood creatinine more than 120 mmol/l, arterial hypertension;
- severe coronary heart disease;
- progressive proliferative retinopathy.
Pregnancy is undesirable if:
- HbA1c >7.0% in early pregnancy;
- development of diabetic ketoacidosis in early pregnancy;
- presence of diabetes in both spouses;
- combination of diabetes mellitus with Rh sensitization in the mother;
- combination of diabetes and active pulmonary tuberculosis;
Pregnancy that develops against the background of diabetes mellitus carries a risk to the health of the mother and fetus.
Risk factors for a mother with diabetes:
- progression of vascular complications (retinopathy, nephropathy, ischemic heart disease);
- frequent development of hypoglycemia, ketoacidosis;
- frequent complications of pregnancy (preeclampsia, infection, polyhydramnios).
Risk factors for the fetus:
high perinatal mortality;
congenital anomalies (2-4 times higher);
neonatal complications;
risk of developing diabetes:
- 1.3% - if the mother has type 1 diabetes,
- 6.1% - if the father has type 1 diabetes.
Treatment tactics for diabetes during pregnancy
In the treatment of diabetes during pregnancy, the main goal is to achieve normoglycemia , when the level of glucose in the blood does not go beyond physiological fluctuations (3.5-6.7 mmol/l).
The principles of diet therapy are the exclusion of easily digestible carbohydrates, split meals (5-6 times with an interval of 2-3 hours.) Products that must be completely excluded from the diet include sugar, jam, sweets, baked goods, ice cream, factory juices, other sugar-sweetened drinks, grapes, bananas. The diet is prescribed taking into account body weight and must contain a sufficient amount of calories (at least 1700 kcal per day). 50-55% of the diet should be carbohydrates, 20-25% proteins and 20% fats. Food should contain sufficient fiber. Slowly digestible carbohydrates should be represented by potatoes, cereals (buckwheat, millet, pearl barley, oatmeal) and wholemeal bread. When calculating the calorie content of food, it is convenient to use “bread unit” equivalents. To assimilate one bread unit (10-12 g of carbohydrates) 1-2 units of insulin are required [2,5,8,9].
Bread unit (XE, carbohydrate unit) is a conventional unit developed by nutritionists, used to approximate the amount of carbohydrates in foods: one XE is equal to 10 (excluding dietary fiber) or 12 grams (including ballast substances) carbohydrates or 20 (25) g. bread.
Insulin therapy has been used in the treatment of diabetes since 1922 and is prescribed by an endocrinologist. For 60 years, insulins produced from the pancreas of cows and pigs have been used. Since 1985, human insulin has been produced using genetic engineering. According to the duration of action, all insulins are divided into 4 groups: ultra-short, short, medium and long-acting. The main route of insulin administration is subcutaneous. intramuscular and intravenous insulin administration is indicated only for ketoacidosis. There are traditional and intensive (basal-bolus) insulin therapy. The most modern method of intensive insulin therapy is intensive subcutaneous administration of insulin using a specialized dispenser (pump insulin therapy) [2,9].
For type 1 diabetes, insulin therapy is the main treatment method. In the absence of compensation in pregnant women with type 2 diabetes and GDM, insulin therapy is prescribed while following a diet. The use of oral hypoglycemic drugs and biguanides during pregnancy is contraindicated due to their teratogenic effects. Transfer to insulin therapy in pregnant women with type 2 diabetes is required in almost 40% of patients [8,15]. In GDM, the need for insulin therapy occurs in 10-30% of cases [13].
Algorithm for managing pregnant women with diabetes mellitus
Maintaining an adequate diet:
- calorie content: 1st trimester - 30 kcal/kg BMI,
2 - 3rd trimesters - 35-38 kcal/kg BMI;
- composition: proteins - 15%, fats - 30%,
carbohydrates - 55% (mostly complex).
protein consumption 1.5 - 2.0 g/kg.
- tableted hypoglycemic drugs
Intensive insulin therapy with genetically engineered human insulins.
Regular self-monitoring of glycemia in order to maintain normoglycemia:
- fasting glucose 3.5 - 5.5 mmol/l;
- glycemia after meals 5.0 - 7.8 mmol/l.
Monitoring HbA1c every trimester; the goal is ≤6.5%.
Observation by an ophthalmologist - examination of the fundus once every trimester.
Observation by a gynecologist and diabetologist
(weight, blood pressure, albuminuria are measured at each visit):
- up to 34 weeks of pregnancy - every 2 weeks;
- after 34 weeks - weekly.
Condition of the fetus and newborn
The negative impact of hyperglycemia and ketonemia in early pregnancy is manifested by an increase in the incidence of fetal malformations (diabetic embryopathy). The incidence of fetal malformations in type 1 and type 2 diabetes is 9.5%, and in decompensated diabetes it increases to 20%. The most common defects of the cardiovascular system are anencephaly and anal atresia. In the first 9-12 weeks of pregnancy, the fetus does not yet produce its own insulin. Maternal hyperglycemia during this period of pregnancy causes an increased risk of congenital malformations. An increased level of glucose in the mother’s blood leads to hyperglycemia in the fetus and hypersecretion of insulin by its pancreas, which leads to the development of a symptom complex - “diabetic fetopathy”, the main symptom of which is macrosomia. Excess insulin leads to an increase in the size of the fetus and placenta, inhibits the maturation of the fetal central nervous system, the surfactant system in the lungs, the adrenal cortex, and the hematopoietic system. In this case, hypertrophy of some organs (heart, adrenal glands, liver, kidneys) can be combined with a decrease in the size of others (brain, thymus gland). In addition, fetal hyperinsulinemia inhibits lecithin synthesis. This explains the increased incidence of respiratory distress syndrome observed in children of diabetic mothers. If hyperglycemia is noted shortly before birth, then after birth the child experiences hypoglycemia, the cause of which is persistent high insulinemia with a sudden cessation of the flow of glucose, which previously came through the umbilical vein from the mother. Therefore, immediately after birth, the baby needs an infusion of glucose. Because these hypoglycaemias can be prolonged, in most cases it is necessary to observe the baby of a mother with diabetes for several days in the neonatology department.
On ultrasound, diabetic fetopathy is indicated by a double body contour resulting from excessive deposition of subcutaneous fat.
Achieving and maintaining normoglycemia before and throughout pregnancy significantly reduces the incidence of malformations and perinatal complications of the fetus.
Delivery tactics
The optimal period is 38 - 40 weeks.
The optimal method is programmed vaginal delivery with careful glycemic control during and after birth.
Indications for caesarean section:
- generally accepted in obstetrics;
- the presence of severe or progressive complications of diabetes and pregnancy;
The most common complications during childbirth are premature rupture of amniotic fluid (20-40%), weakness of labor (20-30%). During childbirth with a large fetus, there is a high risk of birth canal injuries, shoulder dystocia and clavicle fracture. On the day of birth, insulin doses must be reduced by 2-2.5 times; in the postpartum period, starting from the 3rd day, insulin doses increase [2,8,9].
Tactics for managing patients after childbirth
Reducing the insulin dose.
Breastfeeding (warn about the possible development of hypoglycemia!).
Control of compensation, complications, weight, blood pressure.
- For GDM: reclassification of the state of maternal carbohydrate metabolism no later than after 6 weeks. after childbirth (with normal glycemic values - repeat examinations once every 3 years; if impaired tolerance to carbohydrates is detected - once a year).
contraception 1.0-1.5 years
Causes of diabetes in pregnant women
The hormonal changes that occur during pregnancy are associated with increased production of large amounts of steroid hormones. Some of them, such as cortisol and progesterone, have a significant effect on cell receptors, increasing their resistance to insulin. This leads to an increase in blood glucose levels and requires a significant increase in insulin production by the pancreas. In cases where the compensatory capabilities of the pancreas are insufficient, sugar metabolism gets out of control and a condition called pregnancy diabetes, or gestational diabetes, develops. This condition occurs quite often. Between 3 and 10% of pregnant women are susceptible to developing pathological insulin resistance, leading to gestational diabetes. Unlike diabetes mellitus diagnosed before pregnancy, pathological insulin resistance that appears during pregnancy does not cause fetal malformations and in most cases does not require treatment with insulin. But, nevertheless, uncompensated gestational diabetes can significantly complicate the course of pregnancy.
Specialists at the Yauza Clinical Hospital diagnose, treat and prevent diabetes in pregnant women and its complications, such as impaired intrauterine growth. Doctors at the Yauza Clinical Hospital strictly monitor the blood sugar level of a pregnant woman and, if necessary, prescribe a specially designed diet. This ensures a comfortable pregnancy and the safety of the expectant mother and baby.
Disadvantages and advantages of the research method
The HbA1c result is much less likely to be distorted by environmental factors. Its advantages also include:
- speed of obtaining results and its high accuracy;
- identifying the problem at the very initial stages of development, when other methods do not indicate pathology;
- versatility, possibility of carrying out for patients of any age group;
- colds, taking medications and physical activity do not affect the results of the analysis.
But there are also some disadvantages:
- high cost of implementation;
- lack of equipment in a medical facility;
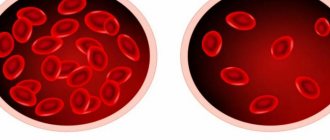
- unreliable results when diagnosing hemoglobinopathy or anemia;
- the result can be distorted by thyroid hormones if the endocrine system malfunctions.
Diabetes in pregnant women - consequences for the child
Large disproportionate fruit. The most important and common complication of diabetes in pregnant women is impaired growth of the intrauterine fetus. Developing in conditions of increased levels of blood glucose, which penetrates the fetoplacental barrier, the fetus is forced to compensate for the increased sugar level using its own insulin. Due to the fact that the structure of insulin and growth hormone are very similar, high levels of insulin stimulate fetal growth. The problem is that a large fetus develops. In such a fetus, the body proportions differ from the proportions of correctly developing newborns, whose head volume is larger than the volume of the shoulder girdle. In fetuses with uncompensated gestational diabetes, the size of the shoulder girdle predominates, and the size of the abdomen increases. This leads to the fact that during childbirth, after the fetal head passes through the birth canal, the shoulders can get stuck (shoulder dystocia) and the baby and the mother can be severely injured or die.
Polyhydramnios or oligohydramnios. In addition, with gestational diabetes, the balance of the amount of amniotic fluid may be disrupted and either polyhydramnios or oligohydramnios may develop. This is a serious risk factor for intrauterine fetal death or premature birth.
Underdevelopment of the lungs. In pregnant women with diabetes, the lungs of the fetus mature later, since the production of surfactant (a special lubricant of the internal walls of the alveoli, where oxygen is exchanged in the lungs) is impaired. Therefore, premature birth with gestational diabetes is especially dangerous.
Hypoglycemia and metabolic disorders in the fetus. Due to the constant increased production of its own insulin during pregnancy, immediately after birth, the child finds himself in a state of hypoglycemia with impaired electrolyte metabolism, which threatens his life.
All this dictates the need for the earliest possible detection of gestational diabetes in pregnant women, the level of sugar in the blood of a pregnant woman and to prevent the development of complications.
.
Diagnosis of diabetes in pregnant women at the Clinical Hospital on Yauza
Signs of diabetes in pregnant women
Gestational diabetes in pregnant women is not usually associated with the classic symptoms of diabetes, such as thirst or excessive urine output (polyuria).
Tests for diabetes in pregnant women
First phase. At the first visit of a pregnant woman to a doctor at any stage, she is examined for glucose levels in venous blood - determination of fasting glucose, regardless of food intake, and glycated hemoglobin. This is the first phase of research to detect diabetes mellitus or gestational diabetes in pregnant women. If diabetes mellitus is detected, the patient is referred for observation and treatment to an endocrinologist.
Second phase. At a period of 24-28 weeks, all patients who did not show any detected disorders of carbohydrate metabolism during the first study are called for a glucose tolerance test (OGTT) to identify “hidden diabetes”. This is done because the occurrence of gestational diabetes is associated with the development of insulin resistance under the influence of hormones produced by the placenta. Therefore, in the vast majority of cases, gestational diabetes develops in the second half of pregnancy after 24 weeks, when the peak production of placental hormones is observed.
Glucose tolerance test
It is carried out to identify pathological insulin resistance, characteristic of latent diabetes in pregnant women. Pregnant women undergo a two-hour test, only in the laboratory. During the 3 days preceding the test, a woman should eat her usual diet, including carbohydrates (>150 g of carbohydrates per day), and maintain her usual physical activity. The evening before testing, dinner should include 30-50 g of carbohydrates. On the day of the study, before the analysis, you should not smoke or take medications that can affect glucose levels (vitamins, glucocorticoid hormones, iron supplements containing carbohydrates, beta-adrenergic agonists, beta-blockers). You can drink water. Venous blood is collected on an empty stomach (after 8-14 hours of fasting, usually in the morning, before breakfast). Then the patient takes a glucose solution (75 g). And blood is drawn an hour and two after the sugar load. Normally, the blood glucose level after a sugar load should not exceed 10 mmol/l after an hour, and 8.5 mmol/l after 2 hours. If manifest diabetes mellitus is detected, the patient is referred to an endocrinologist; for gestational diabetes mellitus, she is treated by an obstetrician-gynecologist or therapist.
How to get tested for glycated hemoglobin?
Blood is taken for research from a vein . Diagnostics does not require special preparation rules; you just need to follow some general recommendations. The patient, as before other tests, should not eat food 2-3 hours before blood sampling; he is only allowed to drink clean, still water. You should not smoke 30 minutes before the test, and you should also avoid physical and emotional stress.
Analysis for glycated hemoglobin - how to donate blood ? There are no specific features when collecting blood from a vein to study glycosylated hemoglobin. According to the standard algorithm for collecting blood from a vein, the patient enters the manipulation room and takes a comfortable position. At the same time, he places his hand on a special hard cushion, bending it slightly at the elbow joint. The nurse bandages the arm above the elbow with a special tourniquet.
The medical professional assesses the condition of the patient's veins, selects the most full vein, treats the area with alcohol, inserts a needle, and draws blood into a vacuum tube.
Then the nurse draws blood to a special mark and removes the needle. A cotton ball is applied to the puncture site.
There is also a scheme for collecting blood using a disposable syringe, however, in modern laboratories they use a system of vacuum tubes - in this case, the likelihood of contact of the patient’s blood with the surface of the skin of medical personnel is reduced, and the risk of damage to blood cells is also reduced.
Then the material is sent for diagnostics, and after some time the patient receives the results of the study, with which he is sent to the attending physician.