Glycated hemoglobin is one of the indicators of a biochemical blood test. Allows you to determine the average blood sugar level over the past three months. In tests it may be referred to as HbA1C or A1C.
Knowing its significance is important in order to promptly identify diabetes mellitus, monitor the course of the disease and the effectiveness of the therapy used.
What may affect the results
Glycated hemoglobin test results may be inconsistent in patients with hemoglobinopathy, including sickle cell disease, pregnancy (second and third trimesters) and the puerperium, HIV, recent bleeding or transfusion, erythropoietin therapy, and patients on hemodialysis. reflect the true glucose content.
Only plasma glucose criteria should be used to diagnose diabetes in these situations. Interpretation of the result may be complicated by the presence of variant forms of hemoglobin: hemoglobin A2, which increases in beta thalassemia (a genetic disease), and fetal hemoglobin (fetal hemoglobin), which remains high until 6 months after birth.
Why are rates declining?
A decrease in glycosylated hemoglobin in diabetics is called hypoglycemia. The cause of the pathological condition is often a tumor of the pancreas, which provokes the synthesis of large amounts of insulin.
Reasons for low HbA1c hemoglobin levels other than diabetes:
- long-term adherence to a low-carbohydrate diet;
- genetic diseases, fructose intolerance;
- kidney pathologies;
- intense physical activity;
- excess insulin dose.
To diagnose pathologies that cause a decrease in HbA1c hemoglobin levels, a comprehensive examination of the entire body is required.
Reference values are presented in the table
| Glycated hemoglobin, % | Interpretation |
| < 6,0 | normal level |
| ≥ 6,5 | diagnostic criterion for diabetes mellitus |
| 6,0 – 6,5 (5,7 – 6,4) | increased risk of developing diabetes and its complications according to WHO (according to ADA, American Diabetes Association) |
Hemoglobin is the oxygen-carrying protein of red blood cells. Depending on the structure there are:
- normal hemoglobin (designated HbA), which makes up 85-95% of total hemoglobin;
- hemoglobin A2 (HbA2), which constitutes less than 3.5% of the total hemoglobin content;
- fetal hemoglobin (HbF) - in an adult it is less than 1%.
Oxygen, joining the hemoglobin found in red blood cells, is delivered to the organs and tissues of the body, where it is needed for their normal functioning.
In various diseases, a chemical change in the structure of hemoglobin occurs. Thus, in diabetes mellitus (a disease associated with impaired absorption of glucose, resulting in the development of hyperglycemia - a persistent increase in blood glucose levels), glucose is added to hemoglobin to form glycated hemoglobin (indicated as HbA1c). And the higher the blood glucose level, the more hemoglobin is modified into glycated hemoglobin.
The formation of glycated hemoglobin is irreversible (that is, glycated hemoglobin cannot return to normal hemoglobin), and its concentration in the blood depends both on the lifespan of red blood cells (up to 120 days) and on the concentration of glucose in the blood. Since the rate of formation of glycated hemoglobin is higher, the higher the level of glucose in the blood, its concentration can be used to judge the average glucose level in the blood over the last 8–12 weeks before the study. Moreover, the content of glycated hemoglobin does not depend on daily and hourly fluctuations in glucose, physical activity and food intake immediately before taking a blood sample.
A glycated hemoglobin test is recommended for all people over 45 years of age for timely assessment of the risk of developing diabetes and its complications (at least once every three years).
If at least one of the risk factors for developing diabetes is present (excess weight, cardiovascular diseases, hypertension (BP ≥ 140/90 mmHg), relatives with diabetes, impaired cholesterol metabolism (HDL (high-density lipoprotein) level) <0.9 mmol/L) or triglyceride levels >2.82 mmol/L), glucose levels should be monitored by testing glycated hemoglobin at least once a year.
For patients diagnosed with diabetes mellitus, glycated hemoglobin concentration testing is recommended to be done every three months to monitor the effectiveness of treatment and assess the risk of complications:
- retinopathy (damage to the retina of the eye, which in severe cases can result in blindness);
- nephropathy (kidney damage);
- polyneuropathy (damage to nerve fibers, which can lead to muscle atrophy (wasting));
- arterial hypertension (high blood pressure);
- atherosclerosis (cholesterol deposits in the walls of blood vessels);
- IHD (coronary heart disease).
Normal hemoglobin level in women
What is glycated hemoglobin in women? This is a specific combination of red blood cell hemoglobin with glucose. For women aged 30 years, the norm is 4.9%, 40 years – 5.8%, 50 years – 6.7%, 60 years – 7.6%. Normally, the content of glycated hemoglobin in seventy-year-old women is 8.6%, and in 80-year-old women it is 9.5%.
For women over 80 years of age, the normal content of glycated hemoglobin is 10.4%. In cases where a patient has been suffering from diabetes mellitus for a long period of time, the endocrinologist can set an individual norm for her, based on the characteristics of the body and the severity of the disease.
When the glycated hemoglobin content is from 5.5% to 7%, women are diagnosed with type 2 diabetes mellitus. An indicator from 7% to 8% indicates well-compensated diabetes mellitus, from 8 to 10% – fairly well compensated, from 10 to 12% – partially compensated. If the level of glycated hemoglobin is over 12%, diabetes is uncompensated.
An increased level of glycated hemoglobin in women may indicate the presence of anemia, impaired body tolerance to glucose, and the consequences of surgical interventions (removal of the spleen). Doctors speak of a reduced level of glycated hemoglobin in women when its content in the blood plasma is less than 4.5%. In pregnant women, the content of glycated hemoglobin may be lower than normal due to an increase in the daily need for iron. For pregnant women, the daily iron requirement is 15 mg-18 mg, from 5 to 15 mg. A decrease in hemoglobin levels in women can occur due to heavy, prolonged uterine bleeding.
Reasons for a decrease in glycated hemoglobin in the blood:
- Hypoglycemia (low blood glucose).
- Normalization of glucose levels in patients with diabetes (effective treatment).
- False underestimation in hemolytic anemia.
- False underestimation after bleeding, blood transfusion (blood transfusion).
Sources:
- Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2021 American Diabetes Association Diabetes Care Jan 2021, 44 (Supplement 1) S15-S33; DOI:10.2337/dc21-S002
- Cas Weykamp, Ph.D. HbA1c: A Review of Analytical and Clinical Aspects. Ann Lab Med 2013;33:393-400
- Wenjia Guo, Qi Zhou, Yanan Jia, Jiancheng Xu. Increased Levels of Glycated Hemoglobin A1c and Iron Deficiency Anemia: A Review. Med Sci Monit 2021 Nov 7;25:8371-8378.
- Oliver Schnell, J Benjamin Crocker, Jianping Weng. Impact of HbA1c Testing at Point of Care on Diabetes Management. J Diabetes Sci Technol 2021 May;11(3):611-617.
Features of the study
The level of glycated hemoglobin may increase under the following conditions:
- the risk of developing diabetes mellitus or the presence of this disease;
- lack of vitamin B12, as well as iron - both components are closely related to hemoglobin metabolism;
- active consumption of alcohol or alcoholic beverages, alcoholism;
- a pronounced decrease in the acidity of erythrocytes;
- chronic renal failure, renal dysfunction;
- genetic or biochemically caused disorders in the protein composition of the blood;
- increased life expectancy of red blood cells;
- against the background of active use of opiates.
The glycating hemoglobin level decreases in the following situations:
- against the background of active intake of vitamin preparations, especially vitamin C, B12;
- for chronic liver diseases;
- against the background of increased acidity of red blood cells;
- when using certain medications, such as aspirin or antiviral drugs;
- with reduced life expectancy of red blood cells.
Before prescribing a diagnosis, the patient must tell the attending physician about the medications that the person is taking, because some medications can have a significant impact on the test result.
Assessing the level of glycated hemoglobin is an important diagnostic criterion that helps the doctor suspect the development of diabetes mellitus in a patient, prescribe additional research methods in a timely manner and begin therapy.
The interpretation of diagnostic results should be carried out exclusively by the attending physician - only the doctor fully understands all the factors that could have influenced the study indicator.
Additional examinations
There are quite a few auxiliary techniques.
- Oral interview and history taking. Doctors record complaints and also examine the probable origin of the deviation in laboratory analysis. This is the first and very important step. Since it sets the vector for all further diagnostics.
- Measuring sugar levels. Building a graph. Specialized technique. It is actively used to examine patients with diabetes. Or as a screening method for healthy people. Who have not yet received a serious diagnosis.
- Ultrasound of the digestive tract.
- FGDS is prescribed as needed. Endoscopy provides information about the organic state of the gastrointestinal tract.
The study of the level of glycated (glycosylated) hemoglobin is mainly used to diagnose diabetes, as well as to assess the quality of therapy and the dynamics of the pathological process. That is, how it develops over time. This is a screening technique.
Sources
- Ribeiro de Lima JG., Abud GF., Freitas EC., Bueno Júnior CR. Effects of the COVID-19 pandemic on the global health of women aged 50 to 70 years. // Exp Gerontol - 2021 - Vol150 - NNULL - p.111349; PMID:33892133
- Manaer T., Yu L., Nabi XH., Dilidaxi D., Liu L., Sailike J. The beneficial effects of the composite probiotics from camel milk on glucose and lipid metabolism, liver and renal function and gut microbiota in db/db mice. // BMC Complement Med Ther - 2021 - Vol21 - N1 - p.127; PMID:33888105
- Mani Deepthi D., Vaikkakara S., Patil A., Ganta S., Sachan A., Raghavendra K., Kiranmayi VS., Chowhan AK. Effect of Correction of Hyperthyroidism with Anti-thyroid Drugs on the Glycated Hemoglobin in Non-diabetic Patients with Primary Hyperthyroidism. // Int J Endocrinol Metab - 2021 - Vol19 - N1 - p.e105751; PMID:33815517
- Pohanka M. Glycated Hemoglobin and Methods for Its Point of Care Testing. // Biosensors (Basel) - 2021 - Vol11 - N3 - p.; PMID:33806493
- Hu X., Deng H., Zhang Y., Guo X., Cai M., Ling C., Li K. Efficacy and Safety of a Decision Support Intervention for Basal Insulin Self-Titration Assisted by the Nurse in Outpatients with T2DM: A Randomized Controlled Trial. // Diabetes Metab Syndr Obes - 2021 - Vol14 - NNULL - p.1315-1327; PMID:33790599
- Okamoto T., Shima H., Noma Y., Komatsu M., Azuma H., Miya K., Tashiro M., Inoue T., Masaki C., Tada H., Takamatsu N., Minakuchi J. Hereditary spherocytosis diagnosed with extremely low glycated hemoglobin compared to plasma glucose levels. // Diabetol Int - 2021 - Vol12 - N2 - p.229-233; PMID:33786277
- Mazahery H., Gammon CS., Lawgun D., Conlon CA., Beck KL., von Hurst PR. Pre-diabetes prevalence and associated factors in New Zealand school children: a cross-sectional study. // NZ Med J - 2021 - Vol134 - N1531 - p.76-90; PMID:33767489
- Abbas E., Ahmed Siddiqui I., Khan MS., Perveen K., Butt A., Fawwad A. Fasting Glucagon Level in Type 2 Diabetes and Impaired Glucose Tolerance and Its Association With Diabetes-Associated Clinical Parameters: A Study From Karachi, Pakistan. // Cureus - 2021 - Vol13 - N2 - p.e13430; PMID:33758717
- Alkethiri K., Almtroudi T., Jurays AB., Abanumay F., Aldammas M., AlKhodheer M., Iqbal M., Habib SS., Bashir S. The relationship between type 2 diabetes mellitus with cognitive functions. // Heliyon - 2021 - Vol7 - N3 - p.e06358; PMID:33748460
- Jaber H., Issa K., Eid A., Saleh F.A. The therapeutic effects of adipose-derived mesenchymal stem cells on obesity and its associated diseases in diet-induced obese mice. // Sci Rep - 2021 - Vol11 - N1 - p.6291; PMID:33737713
The role of the compound in the body
The substances in question perform one key function, although sometimes they speak of two.
- Binding of sugars. This refers to excess glucose. Analyzes show this process well. It is especially noticeable in diabetics. Persons suffering from impaired synthesis and processing of poly- and monosaccharides. Simply put, this is not a transfer, but rather an inactivation of sugars. It happens all the time. Without interruptions throughout a person's life.
- Transport of glucose to tissues. As is the case with typical Hb, the sugar-containing form ensures the transfer of energetically valuable substances to tissues and individual cells. Hence the high rate of energy metabolism. For this reason, glycosylated hemoglobin is one of the key compounds in metabolism.
Such hemoglobin also plays a less noticeable role: we are talking about the most important laboratory practice - testing blood for sugar.
As a rule, the study of Hb1Ac concentration is carried out in parallel to obtain more accurate and informative results. This is an absolutely correct examination tactic.
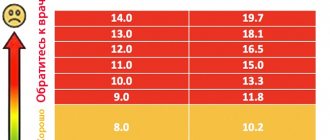
Correspondence table between HbAl and glucose levels
Hemoglobin and sugars are closely related. Glycated fractions are formed through the Maillard reaction. When proteins and saccharides interact.
As a rule, when diagnosing diabetes and a number of other pathological processes, both hemoglobin concentration and glucose levels are examined. Both indicators complement each other. This method is much more informative.
If we talk about compliance with norms and correlation:
| HbA1c level in percent | Sugar concentration in mmol/liter |
| 4 | 3.8 |
| 5 | 5.4 |
| 6 | 7 |
| 7 | 8.6 |
| 8 | 10 |
| 9 | 11.5 |
| 10 | 13.5 |
| 11 | 14.3 |
| 12 | 16 |
| 13 | 18 |
| 14 | 20 |
| 15 | 21 |
| 16 | 23 |
| 17 | 25 |
| 18 | 26 |
| 19 | 27.7 |
The figures are approximate. Deviations of both values are possible.
Prevention and prognosis
In order for glycated hemoglobin to remain within normal limits, several general preventive recommendations must be followed:
- completely give up bad habits;
- eat properly and balanced;
- rationalize your daily routine;
- exercise regularly;
- undergo a complete preventive examination at the clinic at least 2 times a year with visits to all clinicians - for early detection of pathological etiological factors.
Glycosylated hemoglobin has an ambiguous prognosis, since the possibility of correcting the indicator is influenced by the provoking disease. You should donate blood for biochemical study once every 3 months.
What diagnoses can be made
According to the results of the study, glycated hemoglobin shows two main diagnoses:
- Impaired sugar processing. If the concentration of the substance increases, it is almost 100% likely that we can talk about diabetes.
- In some cases, pathological changes accompany disorders of the thyroid gland. When too few substances are produced and they are not able to suppress the excess absorption of sugars.
In some cases, high levels are considered a variant of the clinical norm. But to confirm this, you need to conduct a comprehensive diagnosis under the supervision of an endocrinologist.
If there are no indicators of diabetes or other symptoms of the disease, dynamic monitoring of the patient’s condition is continued and additional measures are prescribed.
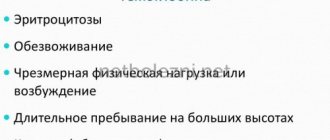
Pathological reasons for the increase
An increase in glycated hemoglobin in the analysis does not bode well for the patient: with one hundred percent probability we can talk about damage to the body. If we make allowances for natural changes, it is worth mentioning the figure 95-97%.
Here is just a small list of pathological processes.
Spleen lesions
This organ is responsible for the deposition (accumulation) of blood cells. In particular, red blood cells. This is where red blood cells end their lives, die and are recycled. However, this is not all. The cycle continues constantly.
With lesions of the spleen, an increase in glycated hemoglobin occurs. Because the organ is no longer able to function normally and absorb waste material. Old cells remain in the blood - hence the increase in the concentration of the substance.
Treatment depends on the essence of the pathological process. Most often, disorders of the spleen are eliminated radically. The organ is removed. After some time, the body itself will adapt to the new conditions and everything will be fine.
Liver disorders
The organ plays a key role in all biochemical processes without exception. Diseases such as hepatitis or cirrhosis have an effect.
- In the first case, an inflammatory process occurs without tissue destruction or death. At least fatal dysfunctions do not occur immediately.
- The second pathological process is necrosis itself, the death of liver tissue. If you don't help the largest gland, the consequences will be fatal.
Treatment. Hepatoprotectors are prescribed. Essentiale, Karsil. Herbal infusions are possible. But only as an auxiliary method.
For liver cirrhosis, medications are needed, and an organ transplant is also prescribed. With the help of pills you can suppress and slow down the course of the disorder. Take the disease at least partially under control.
Iron deficiency
Causes iron deficiency anemia. Accordingly, in order to correct the pathological process, special treatment is required.
First-line drugs are ferrocontaining solutions. They artificially replenish iron concentrations. They return everything to normal. Accordingly, glycated hemoglobin is restored.
However, not all so simple. Pathologies sometimes affect the digestive tract. The gastrointestinal tract cannot absorb iron normally. In this situation, all that remains is to treat the underlying disease.
Afterwards, we can talk about the concentration of the substance returning to normal.
Diabetes
A classic endocrinological disorder. Accompanied by impaired insulin production or tissue insensitivity to this substance.
In both cases, the consequences are severe: damage to the central nervous system, digestive tract, and circulatory structures. Everything suffers. Diabetes mellitus is the main reason for which the concentration of glycated hemoglobin in the blood increases.
Treatment consists of symptomatic correction of the body's condition.
- It is necessary to administer insulin systematically, as needed. This is necessary to adjust your sugar levels.
- Patients must adhere to a gentle fortified diet. Minimum fat, easily digestible carbohydrates.
- It is necessary to adjust your body weight. Otherwise there will be no point in therapy.
Glycated hemoglobin returns to normal on its own as soon as the amount of sugar is restored.
How to proceed
Once the test results are confirmed, the pediatrician will refer you to an endocrinologist. Treatment begins with selecting an effective dosage of insulin.
The little patient is prescribed a low-carbohydrate diet and regular blood tests for grape sugar levels. Parents are taught to monitor portion size, food quality, control sugar using a glucometer, and the method of administering insulin.
Scrupulous adherence to the doctor’s recommendations will compensate for impaired insulin production and avoid the development of complications.
Without treatment, the child will begin to lag behind his peers in growth and mental development, vision problems, neurological and vascular pathologies will appear.