A problem in which the blood does not clot well is called a bleeding disorder. It is caused by the fact that blood vessels do not normally become blocked when they are damaged.
When everything is fine, when there is bleeding at the wound site, the blood begins to thicken, which prevents large losses. But sometimes this complex mechanism fails, resulting in severe or prolonged bleeding.
When blood does not clot well, this does not always lead to external loss. It can also appear as bleeding under the skin or in the brain.
Causes
Bleeding disorders are divided depending on the etiology - acquired, genetically determined and congenital, as well as autoimmune.
Blood clotting disorders can be caused by hereditary pathologies, but not only. Genetic diseases can also influence the development of the disease. For example, a newborn baby may be diagnosed with hemophilia or von Willebrand disease.
Also, the disorder can be caused by a lack of vitamin K. In addition, such problems can be a consequence of cancer of the liver and other organs.
Most often, bleeding disorders occur due to infectious hepatitis or scarring, which usually occurs with cirrhosis.
Long-term use of strong antibiotics or drugs to treat blood clots can also cause bleeding problems.
4.What can be done at home for hemophilia?
To prevent bleeding and improve your well-being, patients with hemophilia can recommend the following:
- Ask your doctor about how to manage bleeding if you have hemophilia;
- Maintain a healthy weight. Additional stress on joints due to excess weight can cause bleeding in hemophilia;
- Choose forms of physical activity with caution. It is better to give preference to swimming and other sports that do not put unnecessary stress on the joints;
- Consult your doctor before taking any medications. And do not take aspirin, ibuprofen or other non-steroidal anti-inflammatory drugs because they affect blood clotting.
- Organize your living space to avoid injuries and accidents as much as possible.
Symptoms
Main symptoms of the disease:
- Skin rashes. Depending on the cause of poor coagulation, both small pinpoint hemorrhages (petechiae) and extensive hematomas may appear on the skin.
- Nosebleeds.
- Hemorrhages in the mucous membranes of the mouth, nose, and intestines. The latter option can lead to the appearance of blood in the stool.
- Hemorrhages in the brain. Occurs with fragility of blood vessels and low blood clotting.
- In the event of an injury, cut, or bruise, the bleeding does not stop for a long time.
- Hemorrhages in joints, muscles and internal organs can be observed with the hereditary disease hemophilia. Bruises (hematomas) can form even with minor mechanical damage.
Impaired hemostasis
General information
The process of hemostasis is able to prevent and stop the flow of blood from the vessel. It is he who ensures the formation of the fibrin clot necessary to restore the integrity of the tissue, and finally removes the fibrin when it is no longer needed. Thanks to this system, blood performs an important function - maintaining a liquid state of blood that flows through the vessels, as well as coagulation when the integrity of the vascular wall is violated. As a result, hemostasis should work to maintain blood volume in the body. This complex system involves platelets, blood cells, extravascular tissues, and the vascular wall. Violation of one of the components leads to disruption of the hemostasis process itself.
Causes of impaired hemostasis:
- DIC syndrome. A common type of hemostasis pathology. Blood clotting is impaired due to the massive release of thromboplastic substances from tissues. May be asymptomatic.
- Impaired hemostasis (coagulopathy). Violation of the functions of the blood coagulation and anticoagulation systems. Pathological condition of the body. It is possible to distinguish immune, acquired and genetic forms of coagulopathies.
- Thrombotic syndrome (thrombophilia). It is characterized by inadequate blood coagulation and thrombus formation, leading to ischemia of tissues and organs.
- Hypocoagulative-hemorrhagic condition. Accompanied by a pathological process of reducing blood clotting.
Classification of hemostasis disorders:
- hereditary or acquired;
- hypocoagulative (decreased blood clotting) or hypercoagulative (increased blood clotting);
- local (thrombosis) or global (DIC syndrome).
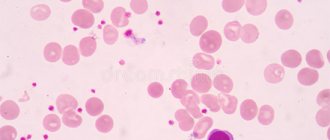
Reduced blood clotting
Reduced blood clotting can be manifested by increased bleeding, repeated bleeding, and hemorrhages that occur even with minor injuries. Platelet-vascular hemostasis is disrupted by quantitative and qualitative changes in platelets (thrombocytopenia and thrombocytopathies), as well as lesions of the vascular wall. Thrombocytopenia is a decrease in the platelet count in the blood below normal. However, spontaneous bleeding occurs only when its number decreases to less than 30 G/l. Thrombocytopathies are understood as qualitative inferiority and dysfunction of platelets with normal or reduced levels.
Causes of decreased blood clotting:
- Immune reactions (viruses, drugs);
- Deficiency of cyanocobalamin and folic acid;
- Effect of toxic drugs;
- Hormonal disorders (hypothyroidism);
- Heredity.
One of the possible causes of bleeding may be a decrease in the production of von Willebrand factor by the endothelium of the vascular wall - a large molecular component of blood coagulation factor VIII (hereditary von Willebrand disease). This factor accumulates in platelets and is released during their degranulation.
Hemorrhagic syndrome
Hemorrhagic syndrome is characterized by a state of increased bleeding and disturbances in one of the links of the blood coagulation system. It can be either an acute or chronic disease.
Characteristic symptoms:
- rash in the form of small dots;
- spots up to 3 mm in diameter (petechiae);
- bruises on the skin and mucous membranes (eczymoses);
- spontaneous bleeding.
Ecchymoses are not just bruises, but characteristic signs of hemorrhage into the skin or mucous membrane. If the above symptoms are detected, it is important to conduct laboratory diagnostics. It will show indicators of a decrease in the number of platelets and an increase in the bleeding time.
von Willebrand disease
Von Willebrand disease is a congenital deficiency of von Willebrand factor (VWF) that results in platelet dysfunction. Usually characterized by mild bleeding. There is also an increase in bleeding time, a normal platelet count, and possibly a slight increase in partial thromboplastin time. The diagnosis is based on low levels of von Willebrand factor antigen and abnormal ristocetin cofactor activity. Treatment includes bleeding control with replacement therapy
Symptoms of von Willebrand disease:
- tendency to subcutaneous hemorrhages;
- prolonged bleeding of small cuts;
- prolonged menstruation (in some cases);
- abnormal bleeding after surgery.
Thrombocytopenia due to impaired hemostasis
Thrombocytopenia is characterized by a decrease in the number of platelets and is accompanied by increased bleeding and problems with bleeding. It can accompany any hematological diseases as one of the main symptoms.
As an independent disease, it is sometimes diagnosed as Werlhof's disease . The main causes of thrombocetopenia are impaired platelet production, as well as their increased destruction. Also among the possible causes are infectious and epidemiological :
- HIV;
- hepatitis;
- acute manifestations of herpes infection;
- Infectious mononucleosis;
- ARVI;
- flu.
Impaired hemostasis and the development of bleeding during thrombocytopenia are caused by the following mechanisms:
- increasing the permeability of microvessels for red blood cells and other components of the blood;
- fragility of blood vessels due to wall degeneration;
- decrease in the adhesive-aggregation function of platelets;
- violation of the reaction of release of platelet coagulation factors;
- decreased clot retraction as a result of decreased activity of platelet contractile protein.
Coagulation hemostasis
Along with the primary, vascular-platelet hemostasis, a secondary hemostasis develops - coagulation. It plays the role of additional support and regulation of blood loss from the vessels. Violation of coagulation hemostasis can be caused by the following factors :
- activation of the fibrinolytic system;
- increase in endogenous anticoagulants;
- overdose of anicoagulants.
Anticoagulants inhibit the formation of fibrin threads; they prevent thrombus formation, help stop the growth of existing blood clots, and enhance the effect of endogenous fibrinolytic enzymes on blood clots.
Causes of phase I disorders of blood coagulation
thromboplastin formation may be the following:
- decreased production of factors (IX, X) in liver pathology;
- formation of antibodies in leukemia;
- overdose of the anticoagulant heparin;
- genetic defects in the synthesis of factors VIII, IX and XI.
Causes of phase II coagulation disorders
Causes of violations of thrombin :
- liver diseases;
- hypovitaminoses;
- jaundice;
- enteritis;
- drug dysbacteriosis;
- extensive resection of the small intestine;
- anaphylactic shock;
- heparin overdose.
Causes of phase III coagulation disorders
Hemorrhagic diathesis associated with a violation of the third phase of coagulation - the phase of fibrin , occurs when:
- liver pathologies;
- affected lungs;
- hereditary factor;
- injuries (surgeries) of the lungs, pancreas, burns.
Increased blood clotting
Increased blood coagulation manifests itself at the local level (thrombosis) or manifests itself as generalized intravascular coagulation. The basis of the disease is a violation of platelet-vascular and coagulation hemostasis.
Hypercoagulation can be caused by:
- increased platelet count in the blood;
- weakening of fibrinolysis;
- an increase in platelet content in the blood;
- decreased antithrombotic properties of the vascular wall.
DIC syndrome is a severe disorder of hemostasis that occurs when there is an excessive intake of procoagulants and blood coagulation activators into the blood, which leads to the formation of multiple microthrombi in the vessels of the microvasculature, and then the development of hypocoagulation, thrombocytopenia and hemorrhage as a result of increased functional activity of the anticoagulation system and blood fibrinolysis with subsequent depletion of all systems. The universality and nonspecificity of DIC syndrome is due to the variety of possible factors of its occurrence. Among them, doctors highlight:
- traumatic surgical operations;
- states of shock;
- infections;
- renal failure;
- obstetric ptology;
- intravascular hemolysis;
- terminal states (the process of the body dying).
Treatment of hemostasis disorders
Treatment of the disease is a difficult task for the resuscitator and anesthesiologist. Most patients with hereditary and congenital forms of pathologies undergo treatment and observation by a specialist throughout their lives. Doctors use three basic principles for treating hemostatic disorders.
Etiotropic principle of treatment. It is necessary to exclude or reduce the degree of action of factors causing hemostasis disorders. This may be protection from the following factors:
- physical:
- chemical;
- biological;
- pathological.
Pathogenetic principle of treatment. To prevent the procoagulant activity of platelets, injections of procoagulants and antifibrinolytic drugs are practiced. Transfusions of whole blood, platelets, and protein blood products (fibrinogen, thrombin) are also actively used.
Symptomatic principle of treatment. Solutions are introduced into the patient's body that normalize the rheological properties of blood (blood fluidity). As a result, normalization of the functions of organs and tissues impaired due to microcirculation disorders, bleeding and hemorrhage is achieved.
Treatment
For treatment of this condition to be effective, the causes of the disease must be determined. It is very important to promptly identify and treat the main disorders - liver pathologies or oncological lesions.
Additional therapy methods include:
- injection of vitamin K;
- drugs to improve clotting;
- transfusion of frozen blood plasma;
- Other medications include hydroxyurea and oprelvekin, which help eliminate platelet problems.
The patient's diet should include foods high in calcium, folic acid, vikasol, and amino acids.
These include dairy products: cheese, cottage cheese, kefir. Fish and meat will also help eliminate the symptoms of pathology. It is equally important to eat leafy vegetables - green onions, spinach, cabbage.
Who needs to determine blood clotting?
To reduce the risk of developing vascular accidents and unexpected bleeding, it is necessary to periodically monitor the state of the blood coagulation system using a laboratory method. This is especially important for:
- people over 40 years old;
- women during and after menopause;
- women during pregnancy;
- people who regularly take blood thinners (aspirin);
- patients suffering from varicose veins;
- those preparing for surgery, etc.
The doctor must prescribe blood clotting tests if hemophilia is suspected (usually this disease is detected in early childhood and young adulthood) or when treating an existing thrombosis with fibrinolytic therapy and anticoagulants.