A coelomic pericardial cyst is a cystic benign neoplasm filled with colorless fluid with thin walls. Such a cyst is a protrusion of the parietal layer of the pericardium, and the structure of the cells of its walls is similar to the structure of the cells of this lining of the heart. It can communicate with the pericardial cavity or be isolated, consisting of one or more chambers.
According to statistics, such neoplasms are detected quite rarely and account for only 4-10% of all mediastinal formations. As a rule, they are found in people 20-40 years old and 2-3 times more often in women over 40.
About 30-50% of coelomic pericardial cysts are small in size and the process is asymptomatic. Typically, cysts are detected by chance during fluorography during preventive examinations or when examining a patient for other diseases. In other cases, the growth of such a formation provokes compression of the heart and other organs and is accompanied by the appearance of symptoms and complications. When the coelomic cyst suppurates and ruptures, the patient may experience signs of hydrothorax or pleuropulmonary shock. In addition, experts note that such a course of pathology can cause malignancy in the areas on which the cystic fluid has poured out.
In this article, we will introduce you to the supposed causes, features of the anatomical structure, types, symptoms, methods of identifying and treating coelomic pericardial cysts. This information will help you get an idea of this pathology, and you can ask the doctor any questions you have.
A little anatomy
Externally, a coelomic cyst looks like a thin-walled cavity neoplasm with a smooth gray-yellow surface, which is filled with clear or straw-yellow serous fluid. Sometimes fatty inclusions are found on the surface of the cyst. A thin vascular network is visible on its wall.
The basis of the walls of the coelomic cyst is a connective tissue permeated with elastic fibers. Its inner surface consists of cubic or flat mesothelium, and its outer surface consists of loose vascularized connective tissue with inclusions of adipose tissue.
The thickness of the walls of coelomic cysts usually does not exceed the thickness of writing paper, and their diameter can reach 3-10 cm (sometimes more). The shape of such formations can be pear-shaped, oval or round.
The liquid found in the formation cavity usually contains very little protein and a lot of salts. In more rare cases, it contains a large amount of protein.
In 60% of patients with such formations, the cyst is located in the right cardiophrenic sinus. In 30% of cases, the tumor is localized in the left cardiophrenic sinus and only in 10% of patients is it detected in other areas of the mediastinum.
Histological analysis of the tissues of coelomic cysts reveals fibrous connective tissue with inclusions of monocytic and lymphoid cells, lined with mesothelium. Muscle fibers are not found in such formations.
Which method of diagnosing pericardial cysts to choose: MRI, CT, ECHO-CG, angiography
Selection method
- ECHO-KG.
Why is pericardial ultrasound performed?
- Well-defined, echo-negative paracardial mass
- There are no internal echoes
- Lack of perfusion on Doppler ultrasound
- Usually do not interfere with cardiac function.
What will a chest x-ray show?
- Homogeneous paracrine formations
- Usually adjacent to the posterolateral part of the heart shadow with a negative silhouette sign.
What MRI and MSCT images of the heart will show for a cyst in the pericardium
CT:
- Clearly limited education
- Usually less than 3 cm
- Thin wall
- Liquid density value 20-50 EX
- No contrast enhancement
- Lack of partition.
MRI:
- hyperintense on T2-weighted image
- Iso- or hyperintense on T1-weighted image (protein-rich fluid)
- No contrast enhancement.
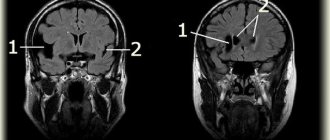
Pericardial cyst. Axial T1-weighted image demonstrates a pericardial cyst (asterisk) in the right paracardia with moderate, homogeneous signal intensity. The cyst has a smooth border and does not contain an internal septum.
Axial fat-suppressed T2-weighted image demonstrates a pericardial cyst with uniform high intensity in the right paracardial region.
Classification
Coelomic pericardial cysts can be classified according to their origin into:
- congenital;
- acquired.
According to experts, in most cases they are congenital malformations of the pericardium or pleura and are formed at different stages of intrauterine development of the fetus. In other cases, the causes of their appearance may be various post-traumatic, inflammatory, parasitic factors or processes caused by the disintegration of neoplasms.
According to the number of coelomic pericardial cysts there are:
- single,
- multiple.
Based on the number of cavities inside the cystic formation, they can be:
- single-chamber,
- multi-chamber.
In relation to the pericardial cavity, coelomic cysts are:
- communicating (either pericardial or pericardial diverticula) – communicating with the pericardial cavity;
- connected by a stalk or adhesions (or parapericardial) – the formation is associated with the pericardium by a thin stalk or a planar fusion;
- detached (extraparacardial) – the formation is isolated and not associated with the pericardium.
According to clinical manifestations, coelomic cysts are:
- asymptomatic;
- uncomplicated;
- complicated.
2. Reasons
Depending on the origin and other features, several variants of pulmonary cysts are distinguished: congenital (true) and acquired (false, secondary, retention); solitary (single) and multiple (pulmonary polycystic disease), communicating with the bronchi (open) and isolated (closed). Accordingly, various factors can lead to the formation of a cyst of one type or another.
Anomalies in the intrauterine development of the respiratory organs are often the cause of the formation of microcystic disease, polycystic disease, or the so-called. giant pulmonary cyst of newborns.
At various stages of life, a cyst can form as a result of injury; tuberculosis or other inflammatory (especially abscess) process; bacterial, fungal or parasitic infestation; bronchiectasis, pulmonary emphysema, etc.
Visit our Pulmonology page
Causes
According to one theory, a pericardial cyst can develop against the background of inflammatory heart diseases - myocarditis, pericarditis or endocarditis.
While scientists are considering two theories about the causes of coelomic pericardial cysts.
I theory
According to the first theory, the formation of such cystic formations is associated with a violation of embryoogenesis. It is believed that cysts form in areas of pericardial weakness that bulge like a diverticulum. They communicate with the pericardial cavity and in the future may separate (unlace) from it and become isolated.
In addition, scientists suggest that a coelomic cyst may be a consequence of improper fusion of embryonic lacunae. Normally, these structures unite and form the pericardial sac. However, if one of the lacunae develops unevenly, a true diverticulum or a cyst isolated from the pericardium can form. So far, this is the theory that most scientists adhere to.
II theory
A number of experts believe that the formation of a coelomic cyst can be provoked not only by disturbances of embryoogenesis, but also by some factors affecting the pericardium after birth:
- inflammatory diseases (myocarditis, pericarditis, endocarditis);
- post-traumatic hematomas of the heart;
- tumor processes;
- parasitic diseases.
Symptoms
Sometimes a coelomic pericardial cyst does not manifest itself in any way, and a person may learn about its existence by chance, during examinations for other diseases. In the future, it may not increase in size, and the state of health will not suffer in any way due to its presence.
In other cases, the coelomic cyst may begin to grow, and an increase in its volume leads to compression of surrounding tissues, vessels and organs:
- atria;
- coronary vessels;
- bronchi;
- esophagus.
The patient experiences discomfort, pressure or pain in the heart area. The pain can be aching or stabbing. In their manifestation, they often resemble an angina attack.
In addition to these signs, a coelomic cyst can cause the following symptoms:
- heartbeat;
- dyspnea;
- asthmatic attacks;
- the appearance of a dry cough when changing position or exertion;
- hoarseness of voice;
- difficulty swallowing food or saliva;
- swelling of the veins in the neck;
- cyanosis;
- pain in the hypochondrium, radiating to the shoulder blade or shoulder;
- deformation of the chest in the region of the heart.
The variability and severity of these symptoms depends on the size and location of the coelomic cyst. As she grows, they become more pronounced.
When a coelomic cyst ruptures, the patient develops signs of hydrothorax and pleuropulmonary shock:
- increasing feeling of heaviness in the chest;
- increased shortness of breath and feeling of lack of air;
- the appearance or intensification of cyanosis;
- forced position: the upper part of the body is raised and tilted towards the accumulation of fluid;
- severe pallor;
- painful cough;
- coldness of hands and feet.
Diagnostics
In some cases, an ECG helps to diagnose a pericardial cyst.
As a rule, patients with coelomic cysts first turn to a cardiologist or pulmonologist when symptoms arise.
The presence of such a pericardial formation can be suspected based on the following examination data of the patient:
- bulging of the chest wall in the area of cyst growth;
- difficulty breathing;
- rapid pulse;
- dull sound when percussing the borders of the heart;
- vascular murmurs on auscultation.
With coelomic cysts adherent to the pericardium, changes can be detected on the ECG.
To confirm the diagnosis, the patient is prescribed the following types of studies:
- chest x-ray;
- fluoroscopy of the heart with the introduction of contrast into the esophagus;
- CT or MRI;
- Echo-KG.
If difficulties arise in diagnosis, the patient may be prescribed thoracoscopy and puncture of the cyst, followed by biochemical and electrolyte analysis of the evacuated fluid.
To eliminate errors, differential diagnosis is carried out with the following diseases:
- diaphragmatic hernia;
- neoplasms of the heart;
- hydatid cyst;
- abdominomediastinal lipoma.
Mediastinal cysts
Radiation diagnostic methods still play a leading role in the diagnosis of tumors and mediastinal cysts. We include multiplanar fluoroscopy and three-plane chest radiography into the radiology examination; when confirming a suspicion of a tumor, we always use computed tomography or magnetic resonance imaging. In some cases, invasive angiography is required to clarify the diagnosis. Fluoroscopy and chest radiography make it possible to identify a formation in the mediastinum, localize it in one or another section and thereby suggest the most likely nosological diagnosis. For more accurate localization of the formation, it is advisable to perform these studies under conditions of contrasting the esophagus in order to identify or exclude its deviation, which is not uncommon with formations of the posterior mediastinum. In addition, we gain insight into the condition of the lungs (hypoventilation due to airway compression), pleural cavities (reactive pleurisy, hydrothorax) and diaphragm function (compression of the phrenic nerves). However, it is most often impossible to differentiate a tumor from a cyst, as well as to judge the tumor’s invasion of surrounding structures on the basis of routine x-ray examination. In addition, it must be taken into account that routine X-ray examination does not always allow one to differentiate mediastinal formations from intrapulmonary and intrapleural ones; in such cases, tomography in any version is necessary.
Standard mediastinal tomography , pneumomediastinography, pneumomediastinotomography, which until recently were the methods of choice, are now almost completely replaced from the diagnosis of mediastinal formations by modern, more accurate methods of radiation diagnostics. Computed tomography and magnetic resonance imaging, confirming and clarifying the localization of the formation, provide answers to these questions: analysis of tomograms with high accuracy demonstrates the connection of mediastinal formations with certain organs and structures, and densitometry makes it possible to distinguish denser tumor tissue from the less dense fluid contents of the cyst . Contrasting vessels at the time of examination and the use of magnetic resonance imaging increase the accuracy of visualization of great vessels, which is important for excluding or identifying their invasion or compression. Magnetic resonance imaging seems to be the method of choice also in cases of suspected neurogenic tumor of the posterior mediastinum, since in such situations it is always necessary to exclude an hourglass tumor, and in relation to nervous tissue, magnetic resonance imaging is more sensitive than computed tomography. However, nosological diagnosis based on these high-precision research methods can also be only speculative. Invasive angiography is indicated in those relatively rare cases when it is necessary to exclude or identify invasion or compression of great vessels, or to differentiate the formation from a vascular aneurysm, and computed tomography or magnetic resonance imaging does not provide a definite answer to these questions.
Endoscopic and morphological diagnostics Endoscopic methods in the diagnosis of mediastinal formations are important not only, and perhaps not so much as a means of visual assessment, but as a way to obtain pathological material for morphological studies. Therefore, we will consider them in combination with other methods of morphological diagnosis, in order of increasing invasiveness of the method.
Bronchoscopy is the least invasive, but also the least informative of the instrumental methods for diagnosing mediastinal formations. This study makes it possible to identify and visually quantify the degree of compression of the airways, and also determines the invasion of the trachea and large bronchi by invasive mediastinal tumors. Endoscopically visible deviation of the trachea, bulging of one or another of its walls, expansion of its bifurcation serve as indirect signs of mediastinal formation and indicate its localization. However, a histological diagnosis can be made using bronchoscopy in no more than 25% of cases (Adler et al., 1983). We consider bronchoscopy indicated in all cases of mediastinal formations, which, according to radiological diagnostics, appear to be associated with the respiratory tract.
Fine-needle aspiration biopsy is a more invasive method, but significantly more informative than bronchoscopy. Cytological examination of the punctate obtained by this method provides morphological diagnosis of mediastinal formations, according to the literature, in 80 - 90% of cases. The diagnosis of a mediastinal cyst is confirmed immediately by puncture. Fine-needle biopsy, performed under the control of computed tomography, can reach almost all anatomical parts of the mediastinum. If necessary, puncture with a thin needle can be performed not only by percutaneous, but also by transesophageal, transtracheal or transbronchial access. An important advantage of the method is the ability to perform the procedure on an outpatient basis using local anesthesia, which is especially important for patients with signs of mediastinal compression. Based on the above advantages, many authors consider it necessary in all cases of mediastinal formations to begin morphological diagnosis with fine-needle aspiration biopsy, using more invasive methods only in cases where puncture of the formation does not provide a definite diagnosis.
The disadvantages of puncture biopsy include, first of all, a certain number of complications accompanying it: for example, according to Adler et al (1983), certain complications are observed in 21.4% of puncture biopsies of the mediastinum, including pneumothorax - in 3.6% patients. In addition, the amount of pathological material aspirated through a fine needle is usually very small, which limits its ability to be studied by cytological examination. In addition, if biopsy is a local research method, the results of which largely depend on which point of the visible substrate the biopsy instrument reaches, then puncture biopsy is even more local. Obviously, the last two circumstances are responsible for the not so rare discrepancies between puncture biopsy and postoperative histological diagnoses. Thus, puncture biopsy is justified for all mediastinal formations and is especially indicated in cases where preoperative morphological diagnosis is important for treatment tactics, but the results of this study, unfortunately, cannot be absolute. A biopsy of peripheral lymph nodes (if there are pathological changes in them: enlargement, hardening or pain) is of particular importance for the diagnosis of lymphomas.
Parasternal mediastinotomy, an abdominal surgery requiring hospitalization and general anesthesia, is a variant of open excisional biopsy. The amount of pathological material obtained in this case is usually sufficient for a full-fledged morphological study. However, the possibilities of visualizing a pathological formation in the mediastinum from this approach are very limited, and the range of application of diagnostic mediastinotomy is reduced to a biopsy of formations of the anterior mediastinum adjacent parasternally to the anterior chest wall. The method is used infrequently, and the introduction of endovideosurgery into clinical practice will apparently completely replace mediastinotomy.
Mediastinoscopy in the diagnosis of tumors and mediastinal cysts also has rather limited use. Visualization and excisional biopsy by classical transcervical mediastinoscopy are available only in the middle and upper part of the anterior mediastinum. Due to the limitations of the review and instrumental manipulations, it is possible to make a nosological diagnosis in slightly more than half of the cases. At the same time, many consider mediastinoscopy to be contraindicated for tumors of the anterior mediastinum due to the real possibility of damage to the thymic capsule; in this case, if the tumor is a thymoma, contamination of the mediastinal tissue is inevitable. Thoracoscopy seems to be the most informative diagnostic method, combining the ability to directly visualize mediastinal formations from various angles with excisional biopsy under visual control. The application of this endoscopic technique to the diagnosis and then to the treatment of tumors and mediastinal cysts has expanded significantly with the advent of videothoracoscopy in surgical clinics.
This technique provides the surgeon with a significantly wider view and, as a result, a more accurate selection of the site for biopsy compared to mediastinoscopy and mediastinotomy. Operative videothoracoscopy makes it possible not only to determine the relationship of the mediastinal formation with surrounding structures, but also to identify, in some cases, invasion of the latter. According to various authors, videothoracoscopy with biopsy provides a reliable diagnosis of tumors and mediastinal cysts in 86 - 100% of cases. At the same time, it must be remembered that thoracoscopy is an intracavitary surgical intervention that requires general anesthesia, one-lung artificial ventilation and is accompanied by a certain percentage of complications.
Other diagnostic methods . Other diagnostic techniques have very limited use in the case of tumors and mediastinal cysts. Of historical interest is the Mondor test, aimed at studying disorders of the autonomic innervation of the chest in neurogenic tumors of the posterior mediastinum. There are reports in the literature about certain diagnostic capabilities of radioisotope methods (Ferguson et al., 1987), tumor markers (Kohman et al., 1993), and the diagnosis of parathyroid cysts based on determining the level of parathyroid hormone in their contents (Ramos-Gabatin et al. , 1985). But all these reports refer to casuistically rare cases and therefore are not included in the usual algorithm for examining patients with mediastinal masses.
So, diagnosis of a mediastinal tumor or cyst begins with a standard x-ray examination, the main purpose of which is to answer the question: are we really dealing with a mediastinal formation?
The next stage is modern methods of non-invasive radiation diagnostics: computed tomography and magnetic resonance imaging, which should clarify the localization of the formation, its structure, consistency, identify its relationships with surrounding organs and anatomical structures, as well as the nature of these relationships. Endoscopic and biopsy methods, confirming the diagnosis, should answer the question about the nosology of the formation and thereby provide grounds for choosing treatment tactics.
However, as can be seen from the above, none of the preoperative diagnostic methods, including even such informative ones as videothoracoscopy with biopsy, guarantees against errors and discrepancies with the final diagnosis when it comes to mediastinal tumors and cysts. In connection with this circumstance, the last means of surgical diagnosis—early surgical exploration, which is usually immediately followed by removal of the formation—is of particular importance. Regarding staging studies, as we mentioned above, most malignant and invasive mediastinal tumors usually do not produce the hematogenous metastases so typical of other malignancies and rarely produce distant implants. Since there are simply no typical localizations of the latter, the development of screening methods for searching for implants is very difficult. Therefore, staging studies are usually planned after a morphological diagnosis has been established, based on the type of tumor and its tendency to spread.
The required minimum examination for suspected mediastinal formation includes: • multiplanar fluoroscopy and three-plane radiography of the chest organs under contrast conditions of the esophagus; • computed tomography of the mediastinum, if invasion of large vessels is suspected - under conditions of bolus contrast of the latter; for tumors of the posterior mediastinum that are suspected to be neurogenic, magnetic resonance imaging is advisable; • bronchoscopy - in case of formation of the mediastinum, demonstrating intimate connections with the trachea or large bronchi. • If the above diagnostic measures do not allow us to establish the nosology of the formation, modern requirements dictate the need to move to more invasive methods of morphological diagnosis: • transthoracic fine-needle aspiration biopsy under the control of a computer or magnetic resonance imaging scanner; • diagnostic video thoracoscopy; • wide thoraco- or sternotomy, combining diagnostic and therapeutic purposes.
The main role in the diagnosis of pericardial cysts and diverticula, as well as other mediastinal neoplasms, is played by X-ray examination. Multiaxial fluoroscopy and radiography of the chest cavity allows one to determine the localization of the formation, its relationship to neighboring organs, its shape and changes in its position during respiratory movements.
An informative research method is CT. This modern research method allows not only to identify the formation, determine its size, but also to assess the thickness of the walls of the cyst, the nature of the contents, and the relationship with neighboring anatomical formations.
Another modern research method is ultrasound echocardiography (EchoCG). Using this widespread, informative, non-burdensome research method for the patient, it is possible to identify thin-walled, cavity, fluid-filled formations, evaluate their relationship with the heart and other mediastinal organs, and identify communication with the pericardial cavity.
Differential diagnosis of pericardial cysts is quite difficult. They should be distinguished from dermoid cysts of the mediastinum, lung cysts, and aortic aneurysms. The integrated use of the listed research methods makes it possible to exclude most of these diseases and establish the true nature of the changes.
Treatment
Previously, methods such as puncture or sclerotherapy were used to eliminate coelomic cysts. They gave a dubious or only temporary effect. After puncture and removal of fluid, the cyst cavity was filled with serous contents again over time, and the formation again increased in size. And the introduction of sclerosant into the cyst cavity often resulted in the sclerosing substance entering the cavity of the pericardial sac and causing the development of constrictive pericarditis.
Such imperfect methods have been replaced by other effective cardiac surgical methods for treating coelomic cysts:
- cyst removal during open heart surgery;
- thoracoscopy.
The following clinical cases may be indications for removal of a coelomic pericardial cyst:
- severe symptoms of compression of neighboring organs and tissues;
- risk of cyst suppuration or rupture;
- breakthrough of the cystic cavity into neighboring organs;
- risk of malignant degeneration of the wall.
Traditional cardiac surgery is always associated with many risks and requires the highest qualifications of the surgeon. During such an operation, the cyst is excised, and if the integrity of the pericardial sac is damaged, it is sutured. With such interventions there is always a risk of damage to the phrenic nerve, and therefore during the operation the doctor always mobilizes it.
A more modern and less traumatic method for removing coelomic cysts is thoracoscopy. To perform it, endoscopic equipment is used to remove the formation through small punctures in the chest.
The entire intervention process is accompanied by visual control of the surgical field using a video camera installed with the device. The surgeon, looking at the monitor, can control every movement of the instruments used.
Removal of a coelomic cyst using thoracoscopy is performed in the following steps:
- the doctor examines the cyst and decides on the method of its removal;
- cutting off the cyst or ligating its pedicle using a special technique is performed in close proximity to the pericardium;
- in case of large volumes of formation, a preliminary puncture is performed to remove fluid and reduce the size of the cyst;
- the cystic formation is removed gradually, and the integrity of the pericardium is not compromised.
Thoracoscopic interventions are minimally invasive and are not accompanied by such tissue trauma as classical operations. After removal of the cyst, the patient can get out of bed the next day, experience less postoperative pain and recover faster. As a rule, discharge from the hospital can occur several days after surgery.
3. Symptoms and diagnosis
Small single cysts in most cases are asymptomatic and can only be diagnosed during instrumental examination. Multiple and/or fairly large cysts are manifested by nonspecific symptoms in the form of shortness of breath, cough, chest pain, weakness; in case of suppuration of the cyst, general inflammatory symptoms (fever, high temperature, headache) are added, and with further aggravation the condition can become life-threatening (pneumo- or pyothorax, hyperthermia, intense pain, hemoptysis, indomitable cough, etc.).
A complicated cyst should be differentiated from destructive pulmonary tuberculosis.
The initial examination when dealing with the above-mentioned complaints involves examination, auscultation, percussion and x-rays. The most informative diagnostic method in this case is multislice computed tomography. Depending on the clinical situation, videothoracoscopy, ultrasound, general clinical and special laboratory tests (in particular, allergy tests, in some cases biopsy, etc.) may also be prescribed.
About our clinic Chistye Prudy metro station Medintercom page!
Forecasts
The prognosis for timely surgical treatment of coelomic cysts is favorable. After a course of rehabilitation, patients fully restore their ability to work.
The lack of timely cardiac surgical care for coelomic cysts is always accompanied by the risk of developing life-threatening complications: breakthrough of the cystic cavity into the bronchus or other organs, rupture of the cyst, suppuration and inflammation of nearby tissues, malignancy of the cyst.
Coelomic pericardial cyst is a benign tumor. If the patient is asymptomatic, a patient with such a tumor can be observed by a cardiologist, who will monitor the dynamics of the growth of the cystic formation according to periodically performed X-ray, CT or MRI studies. If the cyst is large and there is a risk of developing its complications, the patient is recommended to undergo surgical treatment, which significantly improves the prognosis of the outcome of the disease.
1.General information
According to generally accepted medical concepts, a cyst is an abnormal, unnatural cavity in any tissue or organ, filled with gas or liquid. Unlike an abscess (a sealed purulent-inflammatory melting in the tissue), a cyst is not necessarily accompanied by inflammation and clinical symptoms; the presence of such a “quiet” cyst may remain unknown to the carrier for a long time.
A cyst in the lung tissue, surrounded by a fibrous and alveolar-epithelial membrane, in general, corresponds to all these characteristics, however, taking into account the peculiarities of the structure and functioning of the respiratory organs, it also has its own specific etiopathogenesis, clinical picture, course and outcome. Cysts in the lungs, as a rule, are initially detected during a preventive or diagnostic X-ray examination in childhood or young age, less often in adults and the elderly. And although a lung cyst is not one of the most common pulmonary diseases, this does not make it any less dangerous.
A must read! Help with hospitalization and treatment!