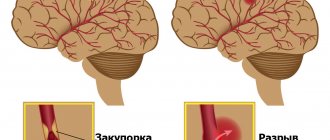
Destruction of venous valves after thrombosis is the main cause of the development of circulatory failure and trophic ulcers in postthrombotic disease. Valvuloplasty (valve repair surgery) for incompetent deep vein valves is an effective method of improving venous outflow. Restoration of the valvular apparatus of the deep veins is possible in various ways, each of them has its own indications. This may involve replacing the affected venous segment with another section of the vein with preserved valves, or switching venous outflow through branches with preserved valves.
The best results are achieved through direct restoration of the valve apparatus using microsurgical valvuloplasty. Valvuloplasty allows for good compensation of venous outflow, which leads to a reduction in edema and healing of trophic ulcers. Deep vein valvuloplasty should be performed by experienced vascular surgeons who are proficient in microsurgical techniques and understand the pathology of venous outflow.
Preparation for surgery and anesthesia
Preparation for intervention on deep vein valves includes bowel cleansing and shaving the hair in the area of surgical access. The night before surgery, the patient is given a mild sedative. Immediately before entering the operating room, premedication is performed with a mild sleeping pill and analgesic.
In the operating room, a catheter is installed in the bladder and a subclavian intravenous catheter for infusion of solutions during surgery. For the purpose of anesthesia, we usually use an epidural catheter - an injection into the spine and prolonged administration of painkillers.
To monitor blood pressure and ECG indicators, a special monitor is connected to the patient.
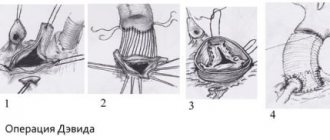
Direct valvuloplasty
It involves dissection of the venous wall above the valve and direct elimination of the anatomical and functional defect. The advantage of the method is the clear identification of the defect, ideal opportunities for restoration of the venous valve leaflets under visual control.
The disadvantages are the risks of damage to the valve apparatus during vein dissection, which can be eliminated by preliminary transverse venotomy followed by dissection of the vein above the valve under visual control. Direct valvuloplasty is a complex surgical procedure, which prevents its widespread use and must be performed under a microscope.
Dilatation of the veins of the extremities is associated with the following risk factors:
- Sedentary lifestyle.
- Pregnancy and childbirth
- Excess weight.
- Work that requires standing for long periods of time.
- Leg injuries.
- Long-term use of contraceptives or other hormonal drugs.
- Congenital weakness of connective tissue and defects of venous valves.
Varicose veins affect about 30% of the adult population in developed countries. That is why phlebologists from the Stolitsa network of clinics pay great attention to the timely detection, diagnosis and treatment of this disease.
External valvuloplasty
It involves narrowing the vein around the valve in order to achieve closure of the valves. This operation has only two advantages: there is no need to cut the vein and it is easy to perform. It is significantly less effective than direct intervention.
The technique of such an operation can be different:
- Using an outer ring or coil on a vein (Vvedensky method)
- An enveloping suture of the vein above the valve without opening the lumen (extravasal valve correction)
- Wrapping the vein with bovine pericardium or a flap from a vascular prosthesis
The main disadvantage of this technique is the uncontrolled effect and the possibility of persistent narrowing of the vein.
Creation of a new venous valve
The principle is to construct a new valve using the patient's venous tissue. The technique for creating the valve depends on the situation with the venous wall. If it is thickened, then it can be stratified, then the resulting flap is fixed in the form of a sail directed with the convex side in the distal direction. You can make a bicuspid valve, which is the most physiological and effective. If there are fibrous cords in the lumen of the vein after thrombosis, then they can be used as leaflets of the valve being created. In the absence of such conditions, you can create a valve using your own venous wall, immersed in the lumen.
Treatment of chronic venous insufficiency
The treatment method for chronic venous insufficiency depends on the stage of the disease and other factors. They can be divided into 3 large groups:
- Disease prevention;
- Conservative treatment methods;
- Surgical treatment methods.
The main methods of prevention
The development of the disease is a sufficient amount of physical activity (walking during the day) and wearing the right shoes (if you have flat feet, correct it). That is, if there are certain risk factors, it is necessary to take appropriate measures to eliminate them.
Conservative methods
Treatments include taking venotonic drugs, the choice of which is currently quite large.
However, the only drugs whose effectiveness has been proven are drugs containing substances such as hesperidin
and
diosmin
(for example, the drug
Detralex
). The duration of medication is determined individually, depending on the stage of the disease.
An important, and often leading role in the treatment of CVI is played by wearing compression garments of varying degrees of compression. The selection of these products must be approached with special care and trusted only from trusted manufacturers.
If you have varicose veins in your legs, conservative treatment methods alone may not be enough. In this case, surgical treatment methods
. They, in turn, can be minimally invasive (with small incisions) - sclerotherapy, laser coagulation, radiofrequency ablation or classical. When choosing a surgical treatment method, doctors rely on the wishes of the patient, his age and the presence of concomitant diseases. Let us briefly consider separately the two most popular methods of surgical treatment of varicose veins.
Transplantation (transplantation) of a normal venous segment
In order to restore the valve apparatus in veins that are not suitable for direct valvuloplasty, replacement of the venous segment with a section of the axillary or brachial vein with valves can be used. Using an incision in the shoulder, a section of a healthy vein with valves is removed and sutured into the femoral vein. Thus, a full-fledged valve apparatus is restored.
The disadvantage of this technology is the possibility of developing secondary expansion or, conversely, scarring of the transplanted segment, since the veins are somewhat different in structure.
Diagnosis of varicose veins
The Stolitsa network of clinics uses the most modern, highly informative and patient-safe diagnostic method - ultrasound triplex scanning of veins. Throughout the world, this diagnostic method is considered necessary and sufficient for an accurate diagnosis and determination of treatment strategies.
Our ultrasound helps:
- Assess the size of the veins and their changes in dynamics.
- Determine the presence of blood clots, their size and location
- Assess the condition of the valve apparatus and the efficiency of its operation.
- Examine all indicators of blood flow and assess the patency of veins in color mode.
Thanks to accurate diagnostics, experienced phlebologists at the Stolitsa network of clinics will be able to answer the following questions:
- Is the condition of the venous system normal or is there a venous disease?
- What are the most effective ways to prevent varicose veins in your case?
- How to stop the development of the disease and protect yourself from possible complications.
- What is the prognosis of the disease?
- Which treatment methods will be most effective in your case and what is the predicted result of treatment.
- What alternative treatment methods are suitable for your case.
Possible complications after valvuloplasty
As after any major surgical operation, after valvuloplasty there are complications associated with the intervention itself:
- Bleeding
- Damage to the lymphatic ducts (lymphorrhea)
- Damage to cutaneous and deep nerves
- Postoperative wound suppuration
In our clinic, such complications are extremely rare.
Specific complications of this intervention are:
- Thrombosis of the reconstructed segment
- Ascending venous thrombosis
- Pulmonary thromboembolism
Fortunately, these complications are rare, their frequency does not exceed 1% of all operations performed.
Prognosis after valvuloplasty
The main goal of the intervention is to improve venous hemodynamics in the limb, which should ultimately lead to healing of trophic ulcers, reduction of edema and tissue hardening.
The result of treatment depends primarily on the correct determination of indications for surgery. Such a complex intervention as valvuloplasty should be performed only after all less complex methods of correcting venous outflow have been exhausted - eliminating reflux through the saphenous veins and perforators, the ineffectiveness of compression hosiery and venotonic drugs.
Signs of varicose veins
- The presence of dilated saphenous veins , the non-linear course of the vein is the most objective, but not the only manifestation of varicose veins. Often, even veins dilated several times may not be visible, especially with a pronounced subcutaneous layer.
- Swelling of the lower extremities at the end of the working day, especially with asymmetrical edema, is the earliest and most common sign of varicose veins.
- You should also think about the presence of varicose veins if you have heaviness in the legs in the evening and at night, or cramps in the legs at night.
- Spider veins and the venous pattern of the intradermal veins, although more of an aesthetic problem, may also indicate the presence of changes in the saphenous veins.
- Persistent redness, skin thickening , lipodermatosclerosis, trophic ulcers on the foot of the leg indicate a decompensated course of varicose veins.
Observation after surgery
The patency of the restored venous segment must be monitored after surgery before discharge from the hospital using venous ultrasound.
Subsequently, examinations by a vascular surgeon with ultrasound should be performed at least once every 6 months. After a year, it is advisable to perform MRI venography.
The patient will be prescribed medications to reduce the likelihood of blood clots. Most often it will be warfarin (under the control of an INR analysis), sometimes we prescribe Prodaxa. It is unacceptable to stop taking these medications on your own without consulting your doctor.
Advantages of the Innovative Vascular Center
The Innovative Vascular Center is one of the few medical institutions in Russia where reconstructive operations on the deep venous system are successfully practiced. We have technologies and experience in microsurgical operations on the valves of the veins of the lower extremities in post-thrombotic disease, methods of endovascular correction of venous outflow (angioplasty and stenting of the iliac veins), and bypass operations on the deep veins.
The clinic has worked out in detail the diagnosis of venous outflow disorders and indications for reconstructive surgery on the deep veins.
1.2. Anatomy of the veins of the lower extremities
The first attempt to create a classification of the superficial venous network of the lower extremities in our country belongs to the famous domestic anatomist V. N. Shevkunenko (1949). He believed that the reduction of the primary venous network that occurs during embryogenesis leads to the emergence of main subcutaneous trunks. In accordance with this, he divided all possible structural options into three types: a) the type of incomplete reduction; b) extreme reduction type and c) intermediate type (Fig. 1.3)
Rice. 1.3.
Types of variability of the superficial veins of the lower extremities [Shevkunenko V.N., 1949]. a — type of incomplete reduction; b — type of extreme reduction; c - intermediate type
If in the superficial venous system, mainly on the lower leg, the intermediate type of vein structure dominates, then for the deep veins the main form is most common, which is the result of an extreme degree of reduction of the primary venous network. In this form, the deep veins are represented by two equal trunks with a small number of anastomoses between them. In the scattered form, the veins of the lower leg are multi-trunked, with a large number of anastomoses. The intermediate form occupies a middle position. All three types of structure of the superficial venous system of the lower extremities (main, diffuse and intermediate) have been studied in sufficient detail and do not cause significant controversy. Much more disagreement exists in the description of the structural features of the deep veins at various levels of the lower limb, especially their relationship with each other. The sources of the inferior vena cava are the veins of the foot, where they form two networks - the cutaneous venous plantar network and the cutaneous venous network of the dorsum of the foot. The common dorsal digital veins, which are part of the cutaneous venous network of the dorsum of the foot, anastomose with each other, form the cutaneous dorsal venous arch of the foot. The ends of this arch continue proximally in the form of two longitudinal venous trunks: the lateral marginal vein (v. marginalis lateralis) and the medial vein (v. marginalis medialis). The continuation of these veins on the lower leg are, respectively, the small and large saphenous veins.
On the plantar surface of the foot, a subcutaneous venous plantar arch is distinguished, which widely anastomoses with the marginal veins and sends intercapitate veins into each interdigital space, which anastomose with the veins forming the dorsal arch. The deep venous system of the foot is formed from paired companion veins accompanying the arteries. These veins form two deep arches: dorsal and plantar. The superficial and deep arches are connected by numerous anastomoses. From the dorsal deep arch the anterior tibial veins (vv. tidiales anteriores) are formed, from the plantar (vv. tidiales posteriores) - the posterior tibial veins, receiving the peroneal veins (vv. peroneae). Thus, the dorsal veins of the foot pass into the anterior tibial veins, and the plantar medial and lateral veins form the posterior tibial veins.
Venous valves are present only in the largest veins of the foot. Their location and quantity are variable. The superficial venous system of the foot is connected to the deep system by vessels that do not have valves. This fact is of no small importance in clinical practice, since the introduction of various medicinal and contrast agents into the superficial veins of the foot in the distal direction ensures their unhindered entry into the deep venous system of the lower limb. Thanks to this anatomical feature, it is also possible to measure venous pressure in the deep veins of the foot segment by puncture of the superficial vein of the foot. According to a number of authors, there are about 50 such vessels at the level of the foot, of which 15 are located at the level of the sole.
The venous system of the leg is represented by three main deep collectors (anterior, posterior tibial and peroneal) and two superficial - great and small - saphenous veins. Since the main load in the implementation of outflow from the periphery is borne by the posterior tibial veins, into which the peroneal veins drain, it is the nature of their damage that determines the severity of the clinical manifestations of disorders of venous outflow from the distal parts of the limb.
The great saphenous vein of the lower extremity (v. saphena magna), being a continuation of the medial marginal vein (v. marginalis medialis), passes to the lower leg along the anterior edge of the inner malleolus, then passes along the medial edge of the tibia and, bending around the medial condyle of the femur from behind, in the area of the knee joint passes to the inner surface of the thigh.
The small saphenous vein (v. saphena parva) is a continuation of the external marginal vein of the foot (v. marginalis lateralis). Passing behind the lateral malleolus and heading upward, the small saphenous vein is first located along the outer edge of the Achilles tendon, and then lies on its posterior surface, approaching the midline of the posterior surface of the leg. Usually, starting from this area, the vein is represented by one trunk, less often - two. At the border of the middle and lower third of the leg, the small saphenous vein penetrates the thickness of the deep fascia and is located between its layers. Having reached the popliteal fossa, it pierces the deep layer of fascia and flows into the popliteal vein. Less commonly, the small saphenous vein, passing above the popliteal fossa, flows into the femoral vein or tributaries of the deep vein of the thigh, and sometimes ends in some tributary of the great saphenous vein. Often in its terminal section the vein bifurcates and flows into the deep or saphenous veins in separate trunks. In the upper third of the leg, the small saphenous vein forms numerous anastomoses with the system of the great saphenous vein.
The large and small saphenous veins have a large number of deep branches along their length. The deep veins of the leg in its upper third form the popliteal vein, the sources of which are the posterior and anterior tibial veins.
Superficial veins communicate with deep veins through perforating veins or perforators (vv. perforantes). Yu. H. Loder (1803) divided these veins into direct ones, connecting the main trunks of the saphenous veins with the deep ones, and indirect ones, ensuring the connection of the tributaries of the saphenous veins with the deep venous highways. Since that time, terminological confusion has persisted in the literature regarding the veins connecting the superficial and deep venous systems. R. Linton defined direct perforating veins as veins connecting superficial veins with deep ones, and communicating veins as veins connecting superficial veins with muscular ones. Often in literature and practice, the terms “perforators” and “communicators” are considered equivalent and are used arbitrarily. In the domestic literature, it is currently generally accepted to consider the communicant veins flowing into the main trunks of the deep veins to be direct, and the communicant veins connecting the superficial veins with the muscular tributaries of the deep veins to be indirect. The sections of communicating veins at the level of passage (perforation) of the intrinsic fascia of the leg are called perforating. Many authors combine the concepts of perforating and communicating veins into a single group of internal perforating veins. Starting from the surface with one or more tributaries, after merging, the trunk of the vein passes through the fascia, flowing into the deep or muscular vein independently or dividing into branches. In this regard, some authors distinguish, respectively, several forms of communicating veins: simple, complex, atypical, branching and collecting. Other researchers believe that the perforator vein provides directed transfer of blood from the axes of the superficial veins to the deep veins through perforation of the superficial aponeurosis. The communicating vein promotes indifferent diffusion of blood between various axes or sections of the superficial veins into the supraaponeurotic spaces. In this case, the division of these veins follows the main topographic groups - medial, lateral and posterior.
In each lower limb, up to 155 perforators are described, called “permanent” and identified in at least 75% of studies and surgical interventions performed for varicose veins. The connection between the saphenous and deep veins is carried out mainly indirectly, that is, through the muscular veins. The number of direct communicating veins on the lower leg ranges from 3 to 10. There are much more indirect communicating veins than direct ones. Most perforators are located along the axes of the “power” lines. This arrangement meets a functional need. The simplest perforator vein complex is represented by the simple vein of Cockett. It contains: 1) a supraaponeurotic segment, originating in the nearest axis of the superficial vein; 2) a transaponeurotic segment, perforating the superficial aponeurosis through a larger or smaller lumen, which in some cases allows the passage of arterioles and nerve branches together with the vein; 3) a subaponeurotic segment, ending very quickly in the nearest axis of the deep vein; 4) valve apparatus, classically including one or two supraaponeurotic valves, one to three subaponeurotic valves, a mandatory element of which is the presence of an attachment ring corresponding to the thickening of the venous wall.
The diameter of the communicating veins is also variable. According to various sources, normally it ranges from 0.1 to 4 mm. In pathological processes, ectasia of the communicating veins can reach 7-8 mm or more. From the point of view of practical surgery, in our opinion, the classification of the French phlebological school is most acceptable. They divide perforating veins into minimal (1-1.5 mm), medium (2-2.5 mm) and volumetric (3-3.5 mm). The term "megavena" is used for vessels with a diameter of more than 5 mm.
Thanks to recent anatomical, ultrasound and endoscopic studies of the venous system of the lower extremities, it has become possible to clearly recognize venous valves, which have the appearance of a transparent veil and are able to resist the powerful hemodynamic shocks of muscle pumps. The number, location and direction of the leaflets of the valve structures of the veins are also quite variable. The statement that all veins connecting the superficial and deep venous systems have valves that allow blood to pass only into the depths cannot be considered absolutely reliable, since valveless perforating veins have been identified on the foot and leg. The veins of the leg also have valves, the valves of which are oriented towards the superficial veins in some cases and in the opposite direction in others. Functioning passively depending on the direction of blood flow, the valve apparatus of the veins of the lower extremities prevents retrograde discharge of blood, protecting venules and capillaries from sudden pressure drops during the operation of the muscular-venous mechanisms of the foot, leg and thigh. Hence the mutual dependence of the localization and function of the valves.
Significant variability in the structure of the superficial venous network of the lower extremities is aggravated by discrepancies in the names of veins and the presence of a large number of eponyms, especially in the names of perforating veins. To eliminate such discrepancies and create a unified terminology for the veins of the lower extremities, the International Interdisciplinary Consensus on Venous Anatomical Nomenclature was created in 2001 in Rome. According to it, all veins of the lower extremities are conventionally divided into three systems:
- Superficial veins.
- Deep veins.
- Perforating veins.
Superficial veins lie in the space between the skin and the deep (muscular) fascia. The GSV is located in its own fascial sheath, formed by the splitting of the superficial fascia. The trunk of the SVC is also located in its own fascial sheath, the outer wall of which is a superficial layer of muscular fascia. Superficial veins provide the outflow of approximately 10% of the blood from the lower extremities. The deep veins are located in spaces deeper than this muscular fascia. In addition, deep veins always accompany arteries of the same name, which does not happen with superficial veins.
Rice. 1.24.
Superficial veins of the lower extremities
The deep veins provide the main drainage of blood - 90% of all blood from the lower extremities flows through them. Perforating veins perforate the deep fascia, connecting the superficial and deep veins. The term “communicating veins” is reserved for veins that connect certain veins of the same system (i.e., either superficial to each other, or deep to each other).
Main superficial veins:
1.
Great saphenous vein (GSV) - vena saphena magna, in English literature - great saphenous vein (GSV). Its source is the medial marginal vein of the foot. It goes up the medial surface of the leg and then the thigh. Drained into the BV at the level of the inguinal fold. Has 10-15 valves. The superficial fascia splits into two layers, forming a canal for the GSV and cutaneous nerves. On the thigh, the trunk of the GSV and its large tributaries in relation to the fascia can take three main types of mutual arrangement: - i-type, in which the trunk of the GSV lies entirely subfascially from the SPS to the knee joint; - h-type, in which the trunk of the GSV accompanies a large tributary located suprafascially. At a certain point it pierces the fascia and flows into the GSV. Distal to this location, the trunk of the GSV is usually much smaller in diameter than its tributary; - s-type, extreme degree of h-type, while the trunk of the GSV distal to the confluence of the tributary is aplastic. In this case, it seems that the trunk of the GSV at some point abruptly changes direction, perforating the fascia. The existing fascial canal is considered by many authors as a protective outer “cover” that protects the GSV trunk from excessive stretching when the pressure in it increases.
2.
The most constant tributaries:
2.1
. Intersaphenous vein(s) [vena(e)) intersaphena(e)], in English literature - intersaphenous vein(s) - runs (run) along the medial surface of the leg. Connects the GSV and SSV. Often has connections with perforating veins of the medial surface of the leg.
2.2
. Posterior thigh circumflex vein (vena circumflexa femoris posterior), in English literature - pos terior thigh circumflex vein. It may have its source in the SVC, as well as the lateral venous system. It rises from the back of the thigh, wraps around it, and drains into the GSV.
2.3
. Anterior surrounding thigh vein (vena circumflexa femoris anterior), in English literature - anteri or thigh circumflex vein. May have its source in the lateral venous system. It rises along the anterior surface of the thigh, going around it, and drains into the GSV.
2.4
. Posterior accessory great saphenous vein (vena saphena magna accessoria posterior), in English literature - posterior accessory great saphenous vein (the segment of this vein on the lower leg is called the posterior arched vein or vein of Leonardo). This is the name of any venous segment on the thigh and lower leg, running parallel and posterior to the GSV.
2.5.
Anterior accessory great saphenous vein (vena saphena magna accessoria anterior), in English literature - anterior accessory great saphenous vein. This is the name of any venous segment on the thigh and lower leg, running parallel and anterior to the GSV.
2.6.
Superficial accessory great saphenous vein (vena saphena magna accessoria superficialis), in English literature - superficial accessory great saphenous vein. This is the name of any venous segment on the thigh and lower leg, running parallel to the GSV and more superficial relative to its fascial sheath.
3.
Small saphenous vein (vena saphena parva), in English literature - small saphenous vein. It has its source in the external marginal vein of the foot. It rises along the back surface of the leg and flows into the popliteal vein, most often at the level of the popliteal fold. Receives the following tributaries:
3.1.
Superficial accessory small saphenous vein (vena saphena parva accessoria superficialis), in English literature - superficial accessory small saphenous vein. It runs parallel to the trunk of the SVC above the superficial layer of its fascial sheath. It often drains independently into the popliteal vein.
3.2.
Cranial extension of the small saphenous vein (extensio cranialis venae saphenae parvae), in English literature cranial extension of the small saphenous vein. Previously called the femoropopliteal vein (v. femoropoplitea). It is a rudiment of an embryonic intervenous anastomosis. When there is an anastomosis between this vein and the posterior circumferential femoral vein from the GSV system, it is called the vein of Giacomini.
4.
Lateral venous system (systema venosa lateralis membri inferioris), in English literature - lateral ve nous system. Located on the anterior and lateral surface of the thigh and lower leg. It is assumed that it is a rudiment of the lateral marginal vein system that existed in the embryonic period.
5.
Inguinal venous plexus (confluens venosus subin guinalis), in English literature - confluence of su perficial inguinal veins. It is the terminal section of the GSV near the anastomosis with the BV. Here, in addition to the last three tributaries listed, three fairly constant tributaries flow into: the superficial epigastric vein (v. epigastrica superficialis), the external pudendal vein (v. pu denda externa) and the superficial vein surrounding the ilium (v. circumflexa ilei superficialis). In the English-language literature there is a long-established term Crosse, denoting this anatomical segment of the GSV with the listed tributaries.
Rice. 1.5.
Perforating veins of the lateral and posterior surfaces of the lower extremities
Rice. 1.6.
Perforating veins of the anterior and medial surfaces of the lower extremities
There is no doubt that only the main clinically significant venous collectors are listed and have proper names. Considering the high diversity of the structure of the superficial venous network, other superficial veins not included here should be named by their anatomical location. The deep veins, as already indicated, are located deeper than the muscular fascia and often accompany the arteries of the same name.
Perforating veins are one of the most numerous and diverse venous systems in shape and structure. In clinical practice, they are often called by the names of the authors involved in their description. This is not only inconvenient and difficult to remember, but sometimes it is not entirely historically correct. Therefore, in the above international consensus it is proposed to name perforating veins according to their anatomical location.
Thus, all perforating veins of the lower extremities should be divided into 6 groups, which are divided into subgroups:
1.
Perforating veins of the foot
1.1. Dorsal perforating veins of the foot
1.2. Medial perforating veins of the foot
1.3. Lateral perforating veins of the foot
1.4. Plantar perforating veins of the foot
2.
Perforating veins of the ankle
2.1. Medial perforating veins of the ankle
2.2. Anterior perforating veins of the ankle
2.3. Lateral perforating veins of the ankle
3.
Perforating veins of the leg
3.1. Medial perforating veins of the leg
3.1.1. Paratibial perforating veins
3.1.2. Posterior tibial perforating veins
3.2. Anterior perforating veins of the leg
3.3. Lateral perforating veins of the leg
3.4. Posterior perforating veins of the leg
3.4.1. Medial gastrocnemius perforating veins
3.4.2. Lateral gastrocnemius perforating veins
3.4.3. Intercapital perforating veins
3.4.4. Paraachillary perforating veins
4.
Perforating veins of the knee joint
4.1. Medial perforating veins of the knee joint
4.2. Suprapatellar perforating veins
4.3. Perforating veins of the lateral surface of the knee joint
4.4. Subpatellar perforating veins
4.5. Perforating veins of the popliteal fossa
5.
Perforating veins of the thigh
5.1. Medial perforating veins of the thigh
5.1.1. Perforating veins of the adductor canal
5.1.2. Perforating veins of the groin area
5.2. Perforating veins of the anterior thigh
5.3. Perforating veins of the lateral thigh
5.4. Perforating veins of the posterior thigh
5.4.1. Perforating veins of the posteromedial thigh
5.4.2. Sciatic perforating veins
5.4.3. Perforating veins of the posterolateral thigh
5.5. Pudendal perforating veins
6.
Perforating veins of the buttocks
6.1.
Superior gluteal perforating veins
6.2.
Middle gluteal perforating veins
6.3.
Inferior gluteal perforating veins