Cardiologist
Sokolov
Denis Vladimirovich
16 years of experience
Cardiologist of the first category, candidate of medical sciences, member of the Asute Cardiovascular Care Association (ASSA)
Make an appointment
Extrasystole is a pathology manifested in the form of cardiac arrhythmia. Those suffering from this disease experience extrasystoles - extraordinary contractions of the heart or its individual parts. Patients may feel short of breath, anxiety, and cardiac arrest. The main diagnostic methods are ECG, Holter monitoring, stress cardio tests. The therapeutic course is aimed at eliminating the root cause of heart rhythm disturbances. Treatment of extrasystole is carried out under the supervision of a cardiologist.
General information
The pathology develops against the background of early depolarization of the atria, ventricles or atrioventricular junction. Due to these disorders, the patient's heart contracts prematurely. Isolated cases of extrasystoles can occur in healthy people of any age group.
Most often, signs of extrasystole are detected in men and women over 50 years of age. The disease causes a decrease in coronary and cerebral blood flow. With a complicated course of the pathology, patients may experience cerebrovascular accidents and atrial fibrillation.
Reasons for the development of pathology
The functional form of the disease, which develops in healthy patients without obvious causes, is considered by cardiologists as idiopathic. Heart rhythm disturbances can result from the use of:
- strong tea;
- coffee beans;
- strong alcohol;
- narcotic substances.
Similarly, the condition of patients can be affected by osteochondrosis of the cervical spine, neuroses, vegetative dystonia and arrhythmia (in trained athletes). Women may experience single extrasystoles due to premenstrual syndrome.
The reasons for the development of an organic form of extrasystole in a patient may be:
- heart attacks, cardiosclerosis, coronary heart disease;
- pericarditis and myocarditis;
- congenital or acquired heart defects;
- sarcoidosis, amyloidosis, hemochromatosis.
In some cases, heart rhythm disorder is provoked by an imbalance of sodium, potassium, magnesium and calcium ions in myocardial cells.
Types of pathology
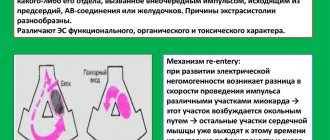
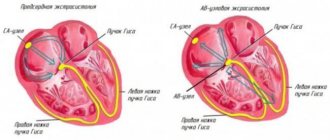
The most common classification of the disease takes into account the reasons for the development of extrasystole in patients. Doctors distinguish functional, organic and toxic forms of pathology. An alternative typology is based on the localization of ectopic foci of excitation and allows us to distinguish four types of heart rhythm disturbances:
- ventricular (62% of clinically diagnosed cases);
- atrioventricular (2%);
- atrial (10%);
- sinoatrial (0.2%).
An important diagnostic sign is the frequency of extrasystoles in the patient. Seizures occurring no more than 5 times per minute are considered rare. The average frequency is recorded at 6–15 extrasystoles per minute, high - at 16 or more.
The problem is not in the extrasystoles themselves, but in the attitude towards them
of extrasystole during the day . Of course, this scared him. The main thing here is to understand that if a person does not have organic damage to the heart muscle, but has neurosis or some kind of exhaustion, then the problem is not in extrasystoles. Because there are people who have 30 thousand extrasystoles a day, but they don’t feel them and live normally. Moreover, almost all people have extrasystoles; they can be detected using a holder - an electrocardiogram device that reads information throughout the day. So the problem is not in the extrasystole , but in the attitude towards it.
Symptoms
Symptoms of extrasystole are not always clearly expressed - the organic form of the disease can proceed almost unnoticed. Extrasystoles are most difficult to tolerate by persons suffering from vegetative-vascular dystonia.
During attacks, patients feel tremors inside the chest, interruptions and freezing of the heart. With functional extrasystole, pain appears, accompanied by fever, weakness, increased sweating, lack of air and increasing feelings of anxiety.
Systematic extrasystoles reduce cardiac output, which leads to a decrease in coronary, cerebral and renal circulation. Patients may feel dizzy. Doctors often record fainting, aphasia or paresis in men and women of the older age group.
Diagnostic measures
Diagnosis of extrasystole takes place in two stages. During the first, the cardiologist examines the patient and collects objective data for anamnesis. The second stage involves men and women undergoing cardiac tests.
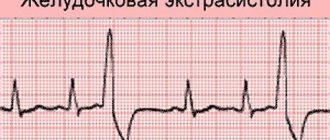
Confirmation of the preliminary diagnosis is carried out during ECG and 24-hour Holter monitoring. These methods make it possible to detect extrasystole in the absence of obvious symptoms of pathology in the patient. Heart rhythm disturbances that do not manifest themselves at rest are recorded during a treadmill test and bicycle ergometry. Ultrasound and MRI of the heart are used as additional diagnostic methods.
How to get rid of extrasystole
The mistake of the VSD person is that he is trying to cure his “heart” disease from a cardiologist, although he does not need this doctor at all. The only thing that can be done is to undergo a heart examination (ultrasound, ECG, Holter) and make sure that there was no cardiac pathology. It is useless to take antiarrhythmic drugs; they will only worsen the situation.
The problem is psychological in nature, so it needs to be solved by a psychologist. Only there, with the help of conversations and special techniques, can one influence the source of extrasystole - the patient’s subconscious. If the condition is severe, then in addition it is necessary to add anti-anxiety drugs. As an independent help, we can recommend trying in every possible way to switch to pleasant events in order to “turn off” your anxious part, due to which extrasystoles appear.
Success attracts those who believe in it. There are many people on the planet who are much more hopeless before death than the typical VSD with his hypochondria and panic. Of course, this is not a reason to calm down and silently endure your fears. But this is a reason to think about the fact that the chances of recovery will be one hundred percent, if you just want to.
Treatment
The treatment tactics for extrasystole are determined by a cardiologist, taking into account the form of the disease diagnosed in a man or woman. The development of heart rhythm disturbances against the background of pathologies of the digestive or endocrine systems will require the patient to contact a gastroenterologist or endocrinologist.
Neurogenic types of the disease are treated with sedatives. If the pathology is toxic, the cardiologist cancels or reduces the dose of drugs that lead to heart rhythm disturbances.
Drug therapy is based on antiarrhythmic drugs. The duration of the course ranges from 4 to 8 weeks. The daily dose of drugs received by the patient gradually decreases as the frequency of extrasystoles decreases.
Radiofrequency ablation is performed when the effectiveness of drug therapy is low. Electrodes are inserted into the patient's heart cavity (through punctures in the femoral vein or artery). Radiofrequency pulses affect arrhythmogenic zones and normalize their condition.
EXTRASYSTOLIA: clinical significance, diagnosis and treatment
Extrasystoles are called premature complexes (premature contractions) detected on an ECG. According to the mechanism of occurrence, premature complexes are divided into extrasystoles and parasystoles. The differences between extrasystole and parasystole are purely electrocardiographic or electrophysiological. The clinical significance and therapeutic measures for extrasystole and parasystole are absolutely the same. According to the location of the source of arrhythmia, electric systoles are divided into supraventricular and ventricular.
Extrasystoles are undoubtedly the most common cardiac arrhythmia. They are often recorded in healthy individuals. When conducting daily ECG monitoring, the statistical “norm” for extrasystoles is considered to be approximately up to 200 supraventricular extrasystoles and up to 200 ventricular extrasystoles per day. Extrasystoles can be single or paired. Three or more extrasystoles in a row are usually called tachycardia (“jogs” of tachycardia, “short episodes of unstable tachycardia”). Unsustained tachycardia refers to episodes of tachycardia lasting less than 30 seconds. Sometimes the definition of “group” or “salvo” extrasystoles is used to designate 3-5 extrasystoles in a row. Very frequent extrasystoles, especially paired and recurrent “jogs” of unstable tachycardia, can reach the degree of continuously recurrent tachycardia, in which 50 to 90% of contractions during the day are ectopic complexes, and sinus contractions are recorded in the form of single complexes or short short-term episodes of sinus rhythm.
In practical work and scientific research, the main attention is paid to ventricular extrasystole. One of the most well-known classifications of ventricular arrhythmias is the classification of B. Lown and M. Wolf (1971).
- Rare single monomorphic extrasystoles - less than 30 per hour.
- Frequent extrasystoles - more than 30 per hour.
- Polymorphic extrasystoles.
- Repeated forms of extrasystoles: 4A - paired, 4B - group (including episodes of ventricular tachycardia).
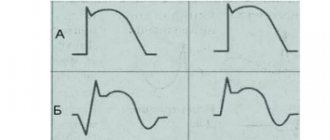
- Early ventricular extrasystoles (type “R on T”).
It was assumed that high gradations of extrasystoles (classes 3–5) are the most dangerous. However, further studies found that the clinical and prognostic significance of extrasystole (and parasystole) is almost entirely determined by the nature of the underlying disease, the degree of organic damage to the heart and the functional state of the myocardium. In individuals without signs of myocardial damage with normal contractile function of the left ventricle (ejection fraction greater than 50%), extrasystole, including episodes of unstable ventricular tachycardia and even continuously recurrent tachycardia, does not affect the prognosis and does not pose a threat to life. Arrhythmias in individuals without signs of organic heart disease are called idiopathic. In patients with organic myocardial damage (post-infarction cardiosclerosis, dilatation and/or hypertrophy of the left ventricle), the presence of extrasystole is considered an additional prognostically unfavorable sign. But even in these cases, extrasystoles do not have an independent prognostic value, but are a reflection of myocardial damage and left ventricular dysfunction.
In 1983, JT Bigger proposed a prognostic classification of ventricular arrhythmias.
- Safe arrhythmias are any extrasystoles and episodes of unstable ventricular tachycardia that do not cause hemodynamic disturbances in persons without signs of organic heart damage.
- Potentially dangerous arrhythmias are ventricular arrhythmias that do not cause hemodynamic disturbances in persons with organic heart disease.
- Life-threatening arrhythmias are episodes of sustained ventricular tachycardia, ventricular arrhythmias accompanied by hemodynamic disturbances, or ventricular fibrillation. Patients with life-threatening ventricular arrhythmias usually have significant organic heart disease (or “electrical heart disease,” eg, long QT syndrome, Brugada syndrome).
However, as noted, ventricular extrasystole does not have an independent prognostic value. Extrasystoles themselves are in most cases safe. Extrasystole is even called a “cosmetic” arrhythmia, thereby emphasizing its safety. Even “jogs” of unstable ventricular tachycardia are also classified as “cosmetic” ari (RW Campbell, K. Nimkhedar, 1990). In any case, treatment of extrasystole with antiarrhythmic drugs (AAP) does not improve the prognosis. Several large controlled clinical trials have shown a marked increase in overall mortality and the incidence of sudden death (2-3 times or more) in patients with organic heart disease while taking class I AAP, despite the effective elimination of extrasystoles and episodes of ventricular tachycardia. The most famous study that first identified the discrepancy between the clinical effectiveness of drugs and their impact on prognosis is the CAST study. The CAST study (“Cardiac Arrhythmia Suppression Study”) in patients who had suffered a myocardial infarction, against the background of effective elimination of ventricular extrasystoles with class I C drugs (flecainide, encainide and moricizine), revealed a significant increase in overall mortality by 2.5 times and the incidence of sudden death in 3.6 times compared with patients taking placebo. The results of the study forced us to reconsider the treatment tactics not only for patients with arrhythmias, but also for cardiac patients in general. The CAST study is one of the fundamental studies in the development of “evidence-based medicine.” Only when taking β-blockers and amiodarone was there a decrease in mortality in patients with post-infarction cardiosclerosis, heart failure, or resuscitated patients. However, the positive effect of amiodarone and especially β-blockers did not depend on the antiarrhythmic effect of these drugs.
Detection of extrasystole (as well as any other variant of rhythm disturbances) is the reason for an examination aimed primarily at identifying the possible cause of arrhythmia, heart disease or extracardiac pathology and determining the functional state of the myocardium.
AAPs do not cure arrhythmia, but only eliminate it while taking the drugs. At the same time, adverse reactions and complications associated with taking almost all drugs can be much more unpleasant and dangerous than extrasystole. Thus, the mere presence of extrasystole (regardless of the frequency and “gradation”) is not an indication for prescribing AAP. Asymptomatic or low-symptomatic extrasystoles do not require special treatment. Such patients are advised to undergo clinical observation with echocardiography approximately 2 times a year to identify possible structural changes and deterioration in the functional state of the left ventricle. L. M. Makarov and O. V. Gorlitskaya (2003) during long-term observation of 540 patients with idiopathic frequent extrasystoles (more than 350 extrasystoles per hour and more than 5000 per day) revealed enlargement of the heart cavities in 20% of patients (“arrhythmogenic cardiomyopathy”) . Moreover, enlargement of the heart cavities was more often observed in the presence of atrial extrasystole.
Indications for the treatment of extrasystole:
- very frequent, as a rule, group extrasystoles, causing hemodynamic disturbances;
- pronounced subjective intolerance to the sensation of interruptions in the heart’s function;
- detection during repeated echocardiographic examination of worsening indicators of the functional state of the myocardium and structural changes (decrease in ejection fraction, dilatation of the left ventricle).
Treatment of extrasystole
It is necessary to explain to the patient that asymptomatic extrasystole is safe, and taking antiarrhythmic drugs can be accompanied by unpleasant side effects or even cause dangerous complications. First of all, it is necessary to eliminate all potentially arrhythmogenic factors: alcohol, smoking, strong tea, coffee, taking sympathomimetic drugs, psycho-emotional stress. You should immediately begin to follow all the rules of a healthy lifestyle.
If there are indications for prescribing AAP in patients with organic heart disease, β-blockers, amiodarone and sotalol are used. In patients without signs of organic heart damage, in addition to these drugs, class I AAPs are used: Etatsizin, Allapinin, Propafenone, Kinidin Durules. Ethacizine is prescribed 50 mg 3 times a day, Allapinin - 25 mg 3 times a day, Propafenone - 150 mg 3 times a day, Kinidin Durules - 200 mg 2-3 times a day.
Treatment of extrasystole is carried out by trial and error, sequentially (for 3-4 days) assessing the effect of taking antiarrhythmic drugs in average daily doses (taking into account contraindications), choosing the most suitable one for a given patient. It may take several weeks or even months to evaluate the antiarrhythmic effect of amiodarone (the use of higher doses of amiodarone, for example 1200 mg/day, can reduce this period to several days).
The effectiveness of amiodarone in suppressing ventricular extrasystoles is 90–95%, sotalol - 75%, class IC drugs - from 75 to 80% (BN Singh, 1993).
The criterion for the effectiveness of AAP is the disappearance of the feeling of interruptions and improvement of well-being. Many cardiologists prefer to start selecting drugs by prescribing β-blockers. In patients with organic heart disease in the absence of effect from β-blockers, Amiodarone is used, including in combination with the former. In patients with extrasystole against the background of bradycardia, the selection of treatment begins with the prescription of drugs that accelerate the heart rate: you can try taking pindolol (Wisken), aminophylline (Teopek) or class I drugs (Etatsizin, Allapinin, Kinidin Durules). Prescribing anticholinergic drugs such as belladonna or sympathomimetics is less effective and is accompanied by numerous side effects.
In case of ineffectiveness of monotherapy, the effect of combinations of various AAPs in reduced doses is assessed. Particularly popular are combinations of AAPs with β-blockers or amiodarone.
There is evidence that the simultaneous administration of β-blockers (and amiodarone) neutralizes the increased risk from taking any antiarrhythmic drugs. In the CAST study, there was no increase in mortality in patients after myocardial infarction who took β-blockers along with class IC drugs. Moreover, a 33% reduction in the incidence of arrhythmic death was found!
The combination of β-blockers and amiodarone is especially effective. With this combination, there was an even greater reduction in mortality than with either drug alone. If the heart rate exceeds 70–80 beats/min at rest and the P–Q interval is within 0.2 s, then there is no problem with the simultaneous administration of amiodarone and β-blockers. In the case of bradycardia or AV block of I-II degree, the administration of amiodarone, β-blockers and their combination requires the implantation of a pacemaker operating in DDD (DDDR) mode. There are reports of increased effectiveness of antiarrhythmic therapy when combining AAP with ACE inhibitors, angiotensin receptor blockers, statins and omega-3-unsaturated fatty acids.
Some controversy exists regarding the use of amiodarone. On the one hand, some cardiologists prescribe amiodarone as a last resort - only if there is no effect from other drugs (believing that amiodarone quite often causes side effects and requires a long “saturation period”). On the other hand, it may be more rational to start selecting therapy with amiodarone as the most effective and convenient drug to take. Amiodarone in low maintenance doses (100–200 mg per day) rarely causes serious side effects or complications and is likely to be safer and better tolerated than most other antiarrhythmic drugs. In any case, in the presence of organic heart disease, the choice is small: β-blockers, amiodarone or sotalol. If there is no effect from taking amiodarone (after a “saturation period” - at least 600-1000 mg / day for 10 days), you can continue taking it at a maintenance dose of 0.2 g / day and, if necessary, evaluate the effect of sequential addition Class I C drugs (Etatsizin, Propafenone, Allapinin) in half doses.
In patients with heart failure, a noticeable decrease in the number of extrasystoles may be observed while taking ACE inhibitors and Veroshpiron.
It should be noted that daily ECG monitoring to assess the effectiveness of antiarrhythmic therapy has lost its importance, since the degree of suppression of extrasystoles does not affect the prognosis. In the CAST study, a pronounced increase in mortality was noted against the background of achieving all criteria for a complete antiarrhythmic effect: a reduction in the total number of extrasystoles by more than 50%, paired extrasystoles by at least 90%, and complete elimination of episodes of ventricular tachycardia. The main criterion for the effectiveness of treatment is improvement in well-being. This usually coincides with a decrease in the number of extrasystoles, and determining the degree of suppression of extrasystoles is not important.
In general, the sequence of selection of AAP in patients with organic heart disease, in the treatment of recurrent arrhythmias, including extrasystole, can be presented as follows.
- β-blocker, amiodarone or sotalol.
- Amiodarone + β-blocker.
- Combinations of drugs:
- β-blocker + class I drug;
- amiodarone + class I C drug;
- sotalol + class I C drug;
- amiodarone + β-blocker + class I C drug.
In patients without signs of organic heart disease, you can use any drugs, in any sequence, or use the scheme proposed for patients with organic heart disease.
Brief characteristics of the AAP
β-blockers. Since the CAST study and the publication of a meta-analysis of studies on the use of class I antiarrhythmic drugs, which showed that almost all class I antiarrhythmic drugs can increase mortality in patients with organic heart disease, beta-blockers have become the most popular antiarrhythmic drugs.
The antiarrhythmic effect of β-blockers is due precisely to the blockade of β-adrenergic receptors, i.e., a decrease in sympathetic-adrenal effects on the heart. Therefore, β-blockers are most effective for arrhythmias associated with sympathetic-adrenal influences - the so-called “catecholamine-dependent” or “adrenergic arrhythmias”. The occurrence of such arrhythmias is usually associated with physical activity or psycho-emotional stress.
Catecholamine-dependent arrhythmias in most cases are simultaneously “tachydependent,” i.e., they occur when a certain critical heart rate is reached, for example, during physical activity, frequent ventricular extrasystole or ventricular tachycardia occur only when the sinus rhythm reaches 130 beats per minute. When taking a sufficient dose of β-blockers, the patient will not be able to achieve a rate of 130 beats/min at any level of physical activity, thus preventing the occurrence of ventricular arrhythmias.
β-blockers are the drugs of choice for the treatment of arrhythmias in congenital long QT syndromes.
For arrhythmias not associated with activation of the sympathetic nervous system, β-blockers are much less effective, but the addition of β-blockers often significantly increases the effectiveness of other antiarrhythmic drugs and reduces the risk of the arrhythmogenic effect of class I antiarrhythmic drugs. Class I drugs in combination with β-blockers do not increase mortality in patients with cardiac damage (CAST study).
For so-called “vagal” arrhythmias, β-blockers have an arrhythmogenic effect. “Vagal” arrhythmias occur at rest, after eating, during sleep, against the background of a decrease in heart rate (“brady-dependent” arrhythmias). However, in some cases, for brady-dependent arrhythmias, the use of pindolol (Wisken), a β-blocker with intrinsic sympathomimetic activity (ISA), is effective. In addition to pindolol, β-blockers with BCA include oxprenolol (Trazicor) and acebutolol (Sectral), however, the internal sympathomimetic activity is expressed to the maximum extent in pindolol.
Doses of β-blockers are adjusted according to their antiarrhythmic effect. An additional criterion for sufficient β-blockade is a decrease in heart rate to 50 beats/min at rest. In previous years, when the main beta-blocker was propranolol (Anaprilin, Obzidan), there were cases of effective use of propranolol for ventricular arrhythmias in doses of up to 960 mg/day or more, for example up to 4 g per day! (RL Woosley et al., 1979).
Amiodarone. Amiodarone tablets 0.2 g (the original drug is Cordarone) has the properties of all four classes of AAP and, in addition, has a moderate a-blocking effect. Amiodarone is undoubtedly the most effective antiarrhythmic drug available. It is even called an “arrhythmolytic drug.”
The main disadvantage of amiodarone is the high frequency of extracardiac side effects, which, with long-term use, are observed in 10–75% of patients. However, the need to discontinue amiodarone occurs in 5–25% (JA Johus et al., 1984; JF Best et al., 1986; WM Smith et al., 1986). The main side effects of amiodarone include: photosensitivity, changes in skin color, dysfunction of the thyroid gland (both hypothyroidism and hyperthyroidism), increased activity of liver transaminases, peripheral neuropathies, muscle weakness, tremor, ataxia, visual impairment. Most of these side effects are reversible and disappear after discontinuation or reduction of the dose of amiodarone. Hypothyroidism can be controlled by taking levothyroxine. The most dangerous side effect of amiodarone is lung damage (“amiodarone lung disease”)—interstitial pneumonitis or, less commonly, pulmonary fibrosis. In most patients, lung damage develops only with long-term use of relatively large maintenance doses of amiodarone - more than 400 mg/day. Such doses are extremely rarely used in Russia. The maintenance dose of amiodarone in Russia is usually 200 mg/day or even less (200 mg per day, 5 days a week). B. Clarke et al (1985) report only three cases out of 48 observations of the occurrence of this complication while taking amiodarone at a dose of 200 mg per day.
The effectiveness of dronedarone, a non-iodine derivative of amiodarone, is currently being studied. Preliminary data indicate that dronedarone has no extracardiac side effects.
Sotalol. Sotalol (Sotalex, Sotahexal) tablets 160 mg is used in an average daily dose of 240–320 mg. Start with 80 mg 2 times a day. For refractory arrhythmias, sotalol up to 640 mg/day is sometimes used. The β-adrenergic blocking effect of sotalol appears starting at a dose of 25 mg.
While taking sotalol, there is an increased risk of developing ventricular tachycardia of the “pirouette” type. Therefore, it is advisable to start taking sotalol in a hospital. When prescribing sotalol, it is necessary to carefully monitor the QT interval, especially in the first 3 days. The corrected QT interval should not exceed 0.5 s. In these cases, the risk of developing pirouette-type tachycardia is less than 2%. With an increase in the dose of sotalol and the degree of prolongation of the QT interval, the risk of developing torsade de pointes (TdP) increases significantly. If the corrected QT interval exceeds 0.55 s, the risk of torsade de pointes reaches 11%. Therefore, if the QT interval prolongs to 0.5 s, it is necessary to reduce the dose of sotalol or discontinue the drug.
The side effects of sotalol correspond to the typical side effects of β-blockers.
Ethacizin. Etatsizin tablets 50 mg. The most studied domestic drug (created in the USSR). It has been used for the treatment of arrhythmias since 1982. The rapid achievement of a clinical effect makes it possible to successfully use Etatsizin in people without organic heart disease for the treatment of ventricular and supraventricular rhythm disturbances: extrasystoles, all types of paroxysmal and chronic tachyarrhythmias, including atrial fibrillation, and Wolff syndrome. Parkinson-White. Etatsizin is most effective in patients with nocturnal arrhythmias, as well as with ventricular extrasystoles. The average daily dose of Etatsizin is 150 mg (50 mg 3 times a day). The maximum daily dose is 250 mg. When ethacizine is prescribed to prevent recurrence of atrial fibrillation, supraventricular and ventricular tachycardias, its effectiveness, as a rule, exceeds that of other class I FGAs. The drug is well tolerated, the need for discontinuation occurs in approximately 4% of patients. Main side effects: dizziness, headache, numbness of the tongue, impaired gaze fixation. Typically, adverse reactions are observed relatively rarely, and their severity decreases after the first week of taking Etatsizin.
Allapinin. The domestic drug Allapinin, 25 mg tablets (also created in the USSR) has been used in clinical practice since 1986. Prescribed 25–50 mg 3 times a day. The maximum daily dose is 300 mg. Allapinin is quite effective for supraventricular and ventricular arrhythmias. The main side effects are dizziness, headache, impaired gaze fixation. The need for withdrawal occurs in approximately 6% of patients. One of the features of allapinin and theoretically its disadvantage is the presence of a β-adrenergic stimulating effect.
Propafenone (Ritmonorm, Propanorm), tablets 150 mg, ampoules 10 ml (35 mg). Prescribe 150–300 mg 3 times a day. If necessary, the dose is increased to 1200 mg/day. Propafenone, in addition to slowing conduction, slightly lengthens refractory periods in all parts of the heart. In addition, propafenone has a slight β-adrenergic blocking effect and calcium antagonist properties.
The main side effects of propafenone include dizziness, impaired gaze fixation, ataxia, nausea, and a metallic taste in the mouth.
Quinidine. Currently, in Russia they mainly use Kinidin Durules, table. 0.2 g each. A single dose is 0.2–0.4 g, the average daily dose is from 0.6 to 1.0 g. The maximum daily dose of quinidine in previous years (when quinidine was the main antiarrhythmic drug) reached 4. 0 g! Currently, such doses are not used and the approximate maximum daily dose of quinidine can be considered 1.6 g.
In small doses (600–800 mg/day), quinidine is well tolerated. Side effects usually occur at higher doses. The most common side effects when taking quinidine include gastrointestinal dysfunction: nausea, vomiting, diarrhea. Headache, dizziness, and orthostatic hypotension are less common. The most dangerous complication from taking quinidine is the occurrence of ventricular tachycardia of the “pirouette” type. According to the literature, this complication occurs in 1–3% of patients taking quinidine.
P. Kh. Janashia , Doctor of Medical Sciences, Professor S. V. Shlyk , Doctor of Medical Sciences, Professor N. M. Shevchenko , Doctor of Medical Sciences, Professor of Russian State Medical University, Moscow
Prognosis and prevention
The nature of the prognosis formed by the cardiologist depends on the form of pathology diagnosed in the patient. The least favorable cases are heart rhythm disturbances that occur against the background of myocardial infarction, cardiomyopathy and myocarditis. Changes in myocardial tissue can provoke atrial fibrillation. The absence of organic heart lesions allows doctors to formulate a favorable prognosis for 85–90% of patients.
A set of preventive measures is aimed at preventing diseases that provoke heart rhythm disturbances: coronary heart disease, cardiomyopathies, myocarditis, etc. Patients of all age groups are recommended to regularly undergo preventive examinations in clinics, visit a therapist, cardiologist, neurologist and doctors of other specializations.
People at risk are advised to exercise moderately and avoid drinking drinks high in caffeine and ethanol.
And here is what antiarrhythmologist Alexander Ivanovich Korzun says about extrasystole:
“ extrasystole and does not require treatment. To their misfortune, someone feels these extrasystoles. In such cases, it is optimal to distract yourself with life: friends, family, children, work, hobbies, etc. If you can’t get distracted, then you need the help of a psychotherapist.”
According to these experienced doctors, it turns out that it does not matter what kind of extrasystoles a person has: ventricular, supraventricular, or preventricular. It is important that if he does not have organic heart disease, then the problem of extrasystole can be successfully solved with the help of a psychotherapist. There are also good experts who say: before there was no holder, and all people lived peacefully. Now the problem arises due to the fact that a person begins to feel extrasystoles, and the holder records them, thus creating a problem. Psychotherapy helps here, that is, increasing stress resistance.
True, the same Korzun also says that extrasystole is often a consequence of problems of the gastrointestinal tract. And gastrointestinal diseases primarily occur in people suffering from nervous disorders. Therefore, if a person really has problems with the gastrointestinal tract (gastritis, ulcers, reflux esophagitis), then he really needs to first treat the stomach in order to reduce the severity and manifestations of extrasystoles.
About drugs
Often, if a person goes to a cardiologist, he is prescribed antiarrhythmic drugs: Citalex, Propanorm, etc. Here, everyone takes responsibility for themselves whether they will take these medications or not, but reliable sources say that these drugs worsen a person’s condition. Therefore, you just need to keep in mind that with a healthy heart, extrasystole does not cause any problems. Problems begin when a person begins to obsess over them, when he begins to struggle with them, when he begins to read what he does not need to read and interpret it incorrectly.
With all the trust and respect for Eduard Guglin or Alexander Korzun, by constantly visiting their sites, a person only harms himself because he comes across some messages that he does not need. He begins to read about other types of arrhythmia, about other problems, without understanding the connection between them and taking individual phrases out of context.
Simply because an ordinary person who has problems and is looking for solutions to them is not a qualified cardiologist.
Therefore, if a person has such a symptom of vegetative-vascular dystonia as extrasystole , and he really wants to get rid of this problem, then, first of all, it is necessary to exclude communication on this topic, stop visiting medical sites and begin to move along the path of getting rid of neurosis, from anxiety disorder, from your internal tension, which leads to these problems. And then the extrasystole will gradually go away.
Of course, this article is intended for a rather narrow audience: some have extrasystole , others do not. If you don't have one, you're lucky: you don't even have to think that you might have one. But if it does appear, you are doubly lucky, because you will know that this is a completely harmless form of arrhythmia.