Varicose veins are a vascular pathology when, against the background of connective tissue weakness, stretching of the venous wall of the vein occurs. The diameter of the vein increases, and its wall becomes thinner.
A large vein diameter leads to a decrease in blood flow speed, venous stagnation, and contributes to pain in the calves. Against this background, varicose veins can lead to thrombophlebitis - inflammation of the affected veins, which is dangerous due to the development of thromboembolic complications. Visible external bumps along the vessels make it possible to recognize varicose veins in the legs. Varicose veins of the lower extremities (ICD code I83) are a very noticeable disease that is easy to remove.
Varicose veins in the esophagus are part of the symptoms of portal hypertension, and secondary varicose veins in the female perineum indicate varicose veins of the small pelvis and difficulty in the outflow of blood from the main veins.
Varicose veins of the spermatic cord (varicocele) are manifested by the clinic of secondary pelvic phlebohypertension and can lead to infertility in men. The etiology and pathogenesis of varicose veins are very diverse depending on the location of the process. In itself, an increase in the diameter of the veins is not dangerous, but complications of varicose veins carry a great risk to the health, and sometimes even to the life of the patient. The cause of the onset of varicose veins on the legs can be heavy physical activity, childbirth, or a sedentary lifestyle of patients.
To understand what varicose veins look like, just go to the summer beach. Although many carriers of varicose veins are embarrassed to appear there, you will definitely see how varicose veins manifest themselves in men and women. The disease is so widespread that you are bound to see it. After reading this article to the end, you will understand how easy it is to treat varicose veins of the legs. Don’t be afraid of going to a phlebologist; on our website you can sign up for a consultation online.
Can we reverse varicose veins?
Many people ask this question, hoping to cure varicose veins at the initial stage with the help of medications or traditional medical methods. If we are talking about varicose veins in the legs, then phlebologists can clearly answer this question - degenerative destruction of the venous wall cannot disappear without turning off the affected vein from the bloodstream or removing it.
It happens that dilated veins may not yet lose their function and increase in volume due to the overflow of blood from the overlying sections, and the muscle pump of the lower leg helps the outflow of blood into the deep veins.
Depending on the stage of varicose veins, various surgical and conservative methods can be used that can stop the progression of varicose veins at various stages. The procedure here is as follows: if a vein is irreversibly damaged, then it must be removed or coagulated, or glued together.
Why is even initial varicose veins irreversible without surgery? To effectively treat varicose veins in the legs, it is necessary to recognize where the pathological discharge of venous blood comes from and remove it with minimal trauma. However, dilated varicose veins can independently and without surgical intervention restore their function if the phlebologist eliminates the pathological discharges that cause varicose veins and irreversibly changed veins.
Modern treatment of varicose veins has advanced significantly since the first operations for varicose veins in men and women in the 19th century. Depending on the degree of varicose veins, a classification of the disease and suitable treatment methods is made.
The clinics of the Innovative Vascular Center know how to treat varicose veins with minimal medical, psychological and cosmetic inconvenience. We do not need to remove varicose veins according to the classical scheme. Our phlebologists have a hemodynamic concept for treating the main causes of varicose veins, a technique that involves correcting only pathologically altered venous outflow and removing only affected veins.
Treatment cannot be directed to the etiology of the disease, but the pathogenesis of the problem is known, so we can stop it. In women, the presence of varicose veins on the legs can be an annoying symptom due to aesthetic problems, but the fair sex is not ready to exchange the ugly appearance of neglected subcutaneous varicose veins for large scars. Therefore, we offer both cosmetic and radical treatment methods that have the best patient reviews.
Discussion
Statistical analysis of the research data forces us to pay attention to the following points. Based on the comparison of the arithmetic mean values most often used in statistical analysis and its standard deviations M±m, it follows that in group 1 (normal) the diameter of the intramuscular veins of the leg, according to ultrasound data at p = 0.05, i.e. with an error allowed in no more than 5% of observations, corresponded to 0.35±0.06; in group 2 (C0-C1) - 0.45±0.06; in the 3rd group (C2-C3) - 0.79±0.15 and in the 4th group - 0.81±0.16. At the same time, the statistically verified level of median diameters in these groups was, respectively, in group 1 (norm) - 0.35 mm; in group 2 (C0-C1) - 0.45 mm; in the 3rd group (C2-C3) - 0.79 mm and in the 4th group (C2-C3) - 0.81 mm.
The frequency of the most commonly established diameters of the intramuscular veins of the leg was: in group 1 (normal) - from 0.25 to 0.45 mm - 94%; in group 2 (C0-C1) - from 0.35 to 0.55 mm - 88%; in the 3rd group (C2-C3) - from 0.5 to 10 mm - 92%, in the 4th group (C4-C6) - from 0.5 to 10 mm - 90%, with a minimum variance of 0.004 in the 1st and 2nd groups and 0.02 in the 3rd and 4th groups. The standard error of asymmetry was no more than 0.1 in all cases. The homogeneity of the set of values within each group is also evidenced by the coefficient of variation, which in each of the compared groups was less than 33% (17.4, 14.3, 18.7 and 18.9%, respectively).
Of no less interest is the comparison of quartiles in each group and the study groups among themselves. In group 1 (normal), with an upper quartile of 0.4 mm and a lower quartile of 0.3 mm, the range was 0.1 mm with a median of 0.33 mm. In group 2 (C0-C1), with the upper quartile being 0.5 mm and the lower quartile being 0.4 mm, the range was 0.1 with a median of 0.5 mm. In group 3, with an upper quartile of 0.9 mm and a lower quartile of 0.7 mm, the range was 0.2 mm with a median of 0.8 mm. Statistically significant changes in intramuscular vein diameters similar to group 3 were observed among patients of group 4 with the upper quartile being 0.9 mm and the lower quartile being 0.7 mm, the median being 0.8 mm.
Considering the statistical significance of the differences in the mathematical expectation with the standard deviation, with the location of the data within the area of acceptance of the alternative hypothesis at critical values of –1.96 and ±1.96, when comparing the obtained data of all groups with each other, the main conclusion can be drawn that as VD progresses, gradual ectasia of the intramuscular veins of the leg. Normally, the diameter of the intramuscular veins of the leg, according to ultrasound, is 3-4 mm. In patients with clinical class C0 and with beginning signs of varicose veins in patients with clinical class C1 according to CEAP, the diameter of the intramuscular veins tends to increase, but in these cases does not exceed 5 mm. Among patients with clinical classes C2-C3, the diameter of the intramuscular veins begins to exceed the established criterion of 5 mm, but does not exceed 8 mm. A further trend of increasing the diameter of the intramuscular veins of the leg in patients with VD persists even with the appearance of trophic skin disorders in clinical classes C4-C6, the diameters of the intramuscular veins are on average 8 mm or more. At the same time, the percentage of established intramuscular vein diameters exceeding 8 mm is 49% in the group of patients with C4-C6, and 46% in patients with C2-C3. Based on the established data, we can conclude that with the progression of CVI in patients with VD, ectasia of the intramuscular veins of the leg is persistent. At the same time, the direct appearance of trophic disorders cannot be associated with the further progression of ectasia, which by this time has already formed and continues to be persistent. Moreover, the diameter of intramuscular veins in groups C2-C6 is 2 times higher than that in patients of clinical classes C0-C1 and is almost 3 times different from the norm.
A little anatomy and physiology
The definition of varicose veins is the primary expansion of the subcutaneous venous trunks of the lower extremities, caused by congenital, contributing and producing factors. The chance of developing varicose veins exists in 40% of adults on the planet. In developed countries, signs of varicose veins are detected in half of the population.
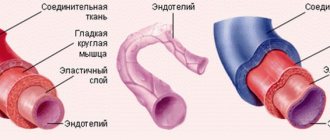
The saphenous veins in the legs are represented by two large venous systems - the system of the great and small saphenous veins. The great saphenous vein begins on the foot, from where it runs along the inner surface of the leg to the groin area, where it flows into the deep vein on the thigh, from the inside of the common femoral artery.
Along the way from the trunk and tributaries of the great saphenous vein, short venous trunks can be identified - perforators, which connect it with the deep veins of the leg and thigh, which is why varicose veins appear away from the main trunks. These perforators are designed to facilitate the path of blood into the deep venous system.
The small saphenous vein is formed at the lateral ankle; it is characterized by several bends along the back surface of the leg and flows into the popliteal vein. The large and small saphenous veins are connected to each other by separate flows. The subcutaneous trunks contain numerous venous valves that ensure the movement of blood to the heart and prevent the reverse flow of blood.
Due to the congenital weakness of the venous wall and the load on it, insufficient functioning of the internal valve apparatus of the veins develops, the blood begins to move in the opposite direction, causing overflow of the saphenous vein, its further stretching and the development of severe varicose veins. Therefore, without eliminating the pathological discharge of blood, it is impossible to achieve a cure for chronic varicose veins.
The classification of subcutaneous varicose veins on the legs is formed from the name and cause of the disease, the affected venous system and the stage of chronic venous insufficiency. Varicose veins of the lower extremities are formed by a combination of several factors:
- Congenital distensibility and weakness of the venous wall and increased intravenous pressure.
- Increased strain on the veins due to prolonged standing activities, heavy physical activity, pregnancy and childbirth.
- Congenital and acquired obstacles to venous outflow (compression syndromes, tumors and bone formations pressing on the veins.
- Consequences of deep vein thrombosis
Vascular diseases of the extremities and their causes
Among diseases of the blood vessels of the legs, atherosclerosis and inflammatory lesions of the arteries are common. Atherosclerotic lesion of the vessels of the lower extremities is a disease that affects older people (over 45 years old), mainly men. With atherosclerosis of the vessels of the extremities, the arteries of the legs narrow, preventing the passage of blood.
Another type of disease that affects the vessels of healthy-looking legs is inflammatory lesions of the arteries. They also cause vasoconstriction, which occurs as a result of the development of the inflammatory process. When inflamed, the walls of the artery thicken evenly along their entire length, complicating the flow of blood. Smoking increases the risk of arterial disease; thromboangiitis obliterans is more often diagnosed in young men who smoke.
Complete blockage or occlusion of the vessels of the legs can occur with any of the listed pathologies. Its sad consequences are gangrene and amputation. To avoid this, consult a doctor promptly when the first characteristic symptoms appear:
- Intermittent claudication;
- Pain in the legs that occurs when walking;
- Feelings of fatigue and weakness in the legs (or one leg);
- Erectile dysfunction in men;
- Cold feet, numbness, tingling sensation.
These and other symptoms of vascular diseases of the lower extremities are a reason to urgently consult a doctor.
Modern principles of treatment of varicose veins
Many patients often ask the question - what treatment is needed for varicose veins if only its first signs appear. Varicose veins on the legs are a continuously progressive disease and prone to complications, so without medical intervention one cannot count on recovery. Let's consider the main indications for the treatment of varicose veins in the legs.
Relief of symptoms of chronic venous insufficiency
Venous hypertension is a subjectively unpleasant consequence of impaired venous outflow, but varicose veins in themselves do not hurt. Symptoms of varicose veins that require prevention and treatment include a feeling of heaviness in the legs, swelling in the evenings, increased fatigue of the legs and even pain in the calf muscles. As the disease progresses, congestion develops in the venous perforators and deep veins, which can lead to skin hyperpigmentation, cause eczema in varicose veins, and heaviness in the calves.
The most popular and popularly advertised method of treating the symptoms of varicose veins on the legs is taking various tablets for varicose veins, using ointments and creams, which makes turning to specialists belated. It is important to understand that such remedies do not affect the course of varicose veins, which is why they can only slightly alleviate complaints and symptoms in the early stages. You should not expect that varicose veins will disappear after treatment with such drugs.
Treatment of complications of varicose veins (trophic ulcers, thrombophlebitis, venous bleeding)
In approximately 50% of cases, varicose veins are complicated by local inflammatory processes, which expands the indications for active surgical tactics. Most often, a patient comes to treat varicose veins when its complications develop - thrombophlebitis (ICD code I80), which is very painful or a trophic ulcer appears. Sometimes night cramps in the calf muscles, redness of the skin, and painful sensations are disturbing.
Treatment of thrombophlebitis can be carried out conservatively (heparin ointment, lyoton, compresses) or more actively - removal of the affected varicose vein or its laser coagulation. Clinical recommendations do not give a clear answer to this question, but with an active approach, along with thrombophlebitis, its cause is also removed, and this is varicose veins.
Trophic ulcer is an extreme manifestation of chronic venous insufficiency and poses a great danger. It looks like a skin defect in the area of the medial ankle with active purulent discharge, flaccid granulations and is accompanied by constant damage to the subcutaneous tissue around.
Beginning varicose ulcers are prone to progression and respond very poorly to conservative treatment. The optimal treatment method today is laser correction of venous outflow (EVLC) for varicose veins of the great or small saphenous vein and proper local treatment (special dressings, washing the ulcer). One doesn’t work without the other, so you can’t count on healing a trophic ulcer with ointments alone. A mandatory component of treatment is compression therapy using special compression stockings. They greatly alleviate patient complaints.
Cosmetic indications for varicose veins
Varicose veins are a disease that rarely leads to dangerous complications, but often forces you to turn to specialists. Convex varicose veins cause many aesthetic problems to their owners. Usually young patients are embarrassed by these nodes and hide their legs. While men are not so afraid of varicose veins and can always wear trousers, women always want to walk around with their legs open.
The good news is that now you can get rid of advanced varicose veins on the legs of women or men in one procedure of laser coagulation of varicose veins without any traces. Modern interventions are performed without incisions, through minimal punctures that are completely invisible 3-4 weeks after the intervention. The patient is placed on the operating table under local anesthesia, and the operation lasts 40-50 minutes. The laser provides amazing cosmetic results and lasting recovery from the manifestations of varicose veins, which is why EVLT is popular among doctors and young patients for varicose veins of the legs at any stage.
Prevention of complications of varicose veins
These problems can be solved using conservative and surgical methods. The main goal of modern phlebology is to minimize surgical trauma in the treatment of varicose veins with the longest possible therapeutic and cosmetic effect. To solve the first problem, it is necessary to block the venous vessels working in the opposite direction, through which a pronounced discharge occurs; to solve the second problem, it is necessary to remove or turn off the dilated veins from the blood circulation.
How can you cure varicose veins on the legs?
Understanding the cause of varicose veins allows you to choose the right method of treatment. The goal of modern treatment of varicose veins is to solve several problems:
- Termination of pathological discharge in a vertical position through the incompetent saphenous veins of the lower extremities.
- Elimination of reflux between deep and superficial veins - perforators - the main mechanism for the development of varicose trophic ulcers.
- Removal of varicose - degenerated superficial vessels (varixes).
- Compression therapy using special stockings and socks.
Diagnosis of varicose veins
To make a correct diagnosis of superficial vein disease, an examination by an experienced specialist and an ultrasound scan of the subcutaneous and deep veins from the abdomen to the feet are necessary. Information from these research methods is sufficient to correctly recognize this diagnosis in the vast majority of patients. The main signs of varicose veins on the legs can be determined with the naked eye, and the causes can be determined using ultrasound.
In some cases, we perform invasive tests including phlebography on an angiographic unit. After treatment, patients need periodic monitoring of the condition of the operated veins, which we carry out using ultrasound diagnostics. If at the diagnostic stage the doctor has questions about the condition of the deep veins, then MRI diagnostics or CT scan with contrast will accurately determine their patency.
Movement of blood through vessels
The difference between arteries and veins is clearly demonstrated by the mechanism of blood flow. When the heart muscle contracts, blood is forced into the arteries. In the largest of them, the aorta, pressure can reach 150 mm Hg. Art. In the capillaries it decreases significantly to 20. In the vena cava the pressure is minimal and amounts to 3-8 mm Hg. Art.
Treatment methods for varicose veins at the Innovative Vascular Center
A vascular surgeon can cure varicose veins of the lower extremities only by eliminating the causes of their occurrence. It is necessary to combat the cause of the development of varicose veins and the progression of the disease. Let's look at the main technologies with proven effectiveness.
Laser treatment of varicose veins (EVLT)
Endovenous laser coagulation is based on heating the venous wall with a coherent light beam. Varicose veins can be effectively treated without any incisions or general anesthesia. A light-conducting fiber is inserted into the vein through a puncture under ultrasound guidance. Laser energy of a certain wavelength at the moment of its occurrence is absorbed by the venous wall, which leads to its heating and destruction of connective tissue. As a result, the vein wall turns into scar tissue and blood flow through the affected vein completely stops. The same effect is achieved as with surgical removal of a vein, but without incisions, general anesthesia and pain.
EVLT is more effective than open phlebectomy. 98% of all operated patients recover from varicose veins, regardless of the degree of development of the nodes. Rare side effects include numbness of the skin in the area of the coagulated vein, inflammation and blood clots in the coagulated veins. The overall incidence of such complications does not exceed 1%. At the Innovative Vascular Center, EVLT is the “gold standard”; it can cure any varicose veins, both in the initial and advanced stages. Patients leave the best reviews just after laser treatment.
Radiofrequency obliteration of varicose veins (RFO)
In terms of its impact and effect, RFO, like laser, is classified as a thermal method for treating varicose veins, but it uses a different physical principle. The radio probe is also inserted into the vein through a puncture. The intervention is performed under local anesthesia. The RFO principle is based on the generation of thermal energy in the probe head, which is then transferred to the walls of the vessel. Heating the wall leads to thermal destruction of its structural elements with subsequent scarring of the vein.
Both of these methods (EVLC and RFO) belong to thermoablative (thermal) technologies. They are similar in their effectiveness, however, the laser heats the vein wall itself, and with RFO, the working surface of the probe heats up and heat is transferred to the wall through the liquid part of the blood.
According to our estimates, EVLT more radically destroys the structure of the affected vein, therefore, after the laser, the relapse rate is lower than with radiofrequency obliteration. We noted the absence of recurrence of varicose veins in 98% after EVLT and 86% after RF. Based on the experience of 20 years of work, our phlebologists have concluded that varicose veins are treated more effectively with thermal methods than with conventional vein removal surgery.
Non-thermal methods of obliteration of varicose veins
In the 70s of the 20th century, surgeons began to show increased interest in minimally invasive types of surgical treatment for varicose veins and began to use electrocoagulators. A good idea, but poorly implemented in practice. Patients reported skin burns, which may be why doctors were afraid to use thermal methods for varicose veins for a long time. Chemical methods used to obliterate veins have proven to be safe and quite effective. These include sclerotherapy in various forms and adhesive obliteration.
Sclerotherapy
Sclerotherapy is the intravenous administration of special drugs that cause damage to the venous wall with subsequent obliteration (overgrowth) of the lumen of the varicose vein. The history of this method dates back to the 19th century and has an interesting development path. At the Innovative Vascular Center, we use the most advanced technology - foam sclerotherapy. Persistent treatment for six months allows you to get rid of varicose veins of the lower extremities for a long time. Although the relapse rate is about 50% over 5 years. With sclerotherapy, treatment is not precisely targeted at the causes of varicose veins, but eliminates the venous nodes themselves, and therefore can be used in combination with other minimally invasive methods (EVLT, RFO). A feature of sclerotherapy is the appearance of dense lumps - coaguls at the site of sclerotic veins, which resolve within six months.
Gluing veins for varicose veins with special glue
Venaseal technology is the name given to a non-thermal method of obliteration of varicose trunks of saphenous veins, which involves introducing a special glue into the lumen of the vein, which polymerizes inside the lumen of the vein, causing its blockage. The idea looks interesting and was developed in the last decade, but there are several pitfalls. Firstly, the glue remains inside the affected veins as a foreign body; it does not dissolve. Secondly, there are risks of periphlebitis around the sealed vein, as the body’s reaction to a foreign body. Thirdly, this is an expensive treatment method.
The cost of treating varicose veins with this method is approximately twice as expensive as laser coagulation. There are no long-term studies regarding the long-term results of such treatment. The advantages of this technology have not yet been identified, but research is actively underway and perhaps varicose veins will become a disease in which the entire treatment regimen will turn into one “magic” injection. It is characteristic that this method has not yet been considered in the latest clinical recommendations, but is already actively proposed by some phlebological centers.
results
In order to exclude the phenomenon of orthostatic hypervolemia, conducting the study in the first half of the day was fundamental. Numerical characteristics of descriptive statistics in all groups are presented in the table . The histograms constructed on the basis of the obtained data are presented in Fig. 2 . A standard histogram of the range of data (medians with an interquartile range of the 25th–75th percentile) obtained in the comparison groups is presented in Fig. 3 . In Fig. 4, 5 show histograms of the range with analysis of data on the mathematical expectation and standard deviations in the comparison groups at critical values of –1.96 and ±1.96. Analysis of the statistical significance of the obtained mathematical characteristics in the comparison groups using a two-sample t-test for independent samples according to the Student's t-test calculated by the program showed a high statistical significance of the differences between all groups, since the p value in all cases was less than 0.0000 and only when comparing C2—C3 and C4-C6 was one order of magnitude greater - 0.004, which did not affect the statistical significance of the differences when testing hypotheses about the mathematical expectation.
Table . Numerical characteristics of descriptive statistics for comparison groups, according to the diameters of the intramuscular veins of the leg, obtained during ultrasound scanning*
| Numerical characteristic | Norm | C0—C1 | C2—C3 | C4—C6 |
| Sample size | 412 | 359 | 570 | 274 |
| Expected value | 0,351 | 0,454 | 0,796 | 0,808 |
| Standard deviation | 0,061 | 0,065 | 0,149 | 0,153 |
| Credibility —95,000% | 0,345 | 0,448 | 0,783 | 0,790 |
| Credibility ±95,000٪ | 0,357 | 0,461 | 0,808 | 0,827 |
| Standard error of mathematical expectation | 0,003 | 0,003 | 0,006 | 0,009 |
| The coefficient of variation, % | 17,4 | 14,3 | 18,7 | 18,9 |
| Median | 0,330 | 0,500 | 0,800 | 0,805 |
| Fashion | 0,300 | 0,500 | 0,900 | 0,900 |
| Mode frequency | 139 | 135 | 67 | 30 |
| Dispersion | 0,004 | 0,004 | 0,022 | 0,023 |
| Minimum value | 0,220 | 0,300 | 0,300 | 0,450 |
| Maximum value | 0,510 | 0,610 | 1,300 | 1,250 |
| Asymmetry | 0,725 | —0,683 | 0,051 | 0,011 |
| Standard error of skewness | 0,120 | 0,129 | 0,102 | 0,147 |
| Lower quartile | 0,300 | 0,400 | 0,700 | 0,700 |
| Upper quartile | 0,400 | 0,500 | 0,900 | 0,910 |
| Quartile range | 0,100 | 0,100 | 0,200 | 0,210 |
| Swipe options | 0,290 | 0,310 | 1,000 | 0,800 |
| 10,000 percentile | 0,300 | 0,350 | 0,600 | 0,600 |
| 90,000 percentile | 0,450 | 0,510 | 0,970 | 0,990 |
Note. *—variable value P (confidence probability) = 0.95; significance level p<0.05.
Rice. 2. Standard histograms of variation series in the compared groups.
a - group 1 (norm); b - 2nd group (C0-C1); c - 3rd group (C2-C3); d - 4th group (C4-C6). The Y axis shows percentages, the X axis shows the diameter of the veins in centimeters.
Rice. 3. Histogram of analysis of median data with interquartile range 25-75th percentile obtained in the compared groups.
Rice. 4. Histogram of data analysis of mathematical expectation and standard deviations in the compared groups.
a - in the 1st (normal) and 2nd (C0-C1); b — in the 1st (normal) and 3rd (C2-C3); c - in the 1st (normal) and 4th (C4-C6).
Rice. 5. Histogram of data analysis of mathematical expectation and standard deviations in groups C0-C1 and C4-C6 (a) and C2-C3 and C4-C6 (b).
Taking into account the established fact, the null hypothesis H0, representing the statement that when clinical classes on CEAP change, there is no change in the diameter of intramuscular veins, was rejected, and the alternative hypothesis H1 was accepted as the main one, stating that when clinical classes on CEAP change in patients, increase in the diameter of the intramuscular veins of the leg.
Surgical methods for treating varicose veins of the lower extremities
Doctors have been dealing with the question of how to get rid of large varicose veins of the superficial veins in the legs and prevent complications since the mid-19th century. The history of the fight against enlarged veins makes it clear how from the early large incisions that disfigured the legs, surgery moved to micropunctures, which make it possible to combat varicose veins without cosmetic defects.
Since the beginning of the 21st century, open surgical methods have begun to give way to minimally invasive thermal and non-thermal ones, but classical phlebectomy is still the most used operation for varicose veins. Radical surgery is actually not superior to thermal obliteration methods in terms of long-term results, but requires serious anesthesia, has a painful postoperative period and residual noticeable scars.
Advanced phlebologists use elements of classical surgery in the form of microphlebectomy using punctures to remove individual varicose nodes and tributaries. This may be the most cosmetic method for removing varicose veins for thin skin. A month after such an operation, there is not even any redness left on the skin.