Pathogenesis
The cause of hemorrhagic diathesis is a violation of one of the stages of hemostasis - a physiological process that stops blood loss. Depending on which stage was violated, HD is divided into:
- Angiopathy (vasopathy). This includes diathesis caused by defects in the vascular walls. Normally, when damaged near the rupture site, the vessel contracts, then the properties of its walls change, they become sticky. This is necessary so that platelets can stick to them. This mechanism is disrupted in HD such as hemorrhagic vasculitis, Randu-Osler-Weber disease, as well as in the absence of vitamin C in the body.
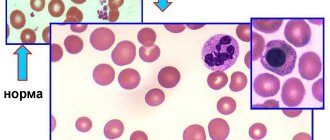
- Thrombocytopathies, i.e. diseases associated with a defect in the platelet component of the coagulation system. Platelets may be produced in insufficient quantities or, as a result of changes in their functional properties, be destroyed too quickly. In both scenarios, platelet adhesion to the walls of blood vessels is difficult. This is typical for thrombocytopenic purpura, leukemia, thrombocytopenia, hemorrhagic aleukia, etc.
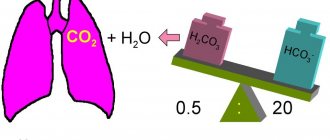
- Hemophilia (coagulopathy). In this group of diseases we are talking about a violation of the plasma component of hemostasis. That is, the stage when a successive cascade of reactions is launched in the blood, as a result of which the protein fibrinogen is converted into insoluble fibrin. This includes hemophilia, parahemophilia, disseminated intravascular coagulation syndrome, congenital afibrinogenemic purpura, etc.
The etiology of the hemostasis defects listed above may be different. There are congenital disorders associated with hereditary pathogenetic factors and acquired ones.
Hereditary ones appear in childhood. Parents usually bring a child to the pediatrician with symptoms.
Acquired ones are called symptomatic, because they are usually a manifestation or complication of some other disease: systemic lupus erythematosus, cirrhosis of the liver, etc. Their debut can only occur in old age.
Diet
Diathesis in children responds well to treatment if the recommended diet is followed.
During breastfeeding, the baby's mother should adhere to it. Allergenic foods (sweets, citrus fruits, eggs, honey, etc.) are excluded. During the introduction of complementary foods, in order to avoid the development of diathesis, the baby’s skin reactions to the new product should be monitored, and if signs of illness appear, exclude it for three to five months, until the next attempt. After the introduction of complementary foods, the basis of the menu should be cereals, lean meat and fish, vegetables and fruits. The consumption of sweets and foods high in food additives should be limited as much as possible. Contact us!
Specialists at the PsorMak Skin Diseases Center have been successfully treating diathesis in children for many years. Contact us for an initial consultation, our doctors will help you develop a complete understanding of how to properly treat the disease in the acute stage (with skin rashes). In addition, we will help you create a dietary diet and suggest what other measures to correct the child’s lifestyle should be taken to improve his health and effectively combat the disease. Make an appointment by calling +7 (495) 150-15-14,
Clinical picture
The main manifestation of hemorrhagic diathesis is bleeding. Depending on their nature, the following classification is proposed:
Capillary (microcirculatory)
They are characterized as painless small superficial hemorrhages into the skin and mucous membranes. This manifests itself as bruises, petechiae, nasal and uterine bleeding, and bleeding gums.
Hematoma
We are talking about extensive hemorrhages in the patient’s joints, muscles, and soft tissues. The result is very painful hematomas that can lead to tissue dissection, deforming arthrosis, and fractures. This type of bleeding is very typical for hemophilia.
Capillary-hematoma (mixed)
This type is characteristic of DIC syndrome, von Willebrand disease, and overdose of anticoagulants. It is a combination of small external hemorrhages, such as microcirculatory ones, and large subcutaneous hematomas.
Vasculitic purpuric
They look like small pinpoint rashes on the arms, legs, thighs, and torso. As a rule, it is distributed symmetrically throughout the body. Accompanied by mild swelling. Residual pigmentation after such rashes remains for a long time. This symptom is characteristic of hemorrhagic vasculitis.
Angiomatous
This includes persistent, recurrent bleeding of one or two localizations. Most often nasal, but sometimes gastrointestinal, pulmonary. A special case of angiomatous hemorrhages is also hematuria - blood in the urine.
A natural consequence of blood loss is often anemia, which is accompanied by increased fatigue, dizziness, pale skin, weight loss, and fever.
Hemorrhagic syndrome in newborns
Pathology of blood coagulation occurs not only in adults, but also in newborns, in whom the risk of its occurrence is somewhat higher due to the imperfection of hematopoiesis and many other organs and systems.
Children in the first days of life are characterized by increased vascular permeability, decreased coagulability and immaturity of the hemostatic system, however, these features are considered physiological and do not contribute to hemorrhagic syndrome.
If in the first hours and days of life a hemorrhagic syndrome appears and rapidly increases in a baby, then most likely it is associated with genetic disorders. Medicines that the pregnant woman took before giving birth (salicylates), hypoxia during pregnancy, and the state of prematurity can also predispose to increased bleeding during the neonatal period.
Often, signs of hemorrhagic syndrome are detected a week after the birth of the baby, when he has already been discharged home, so further observation and determination of the cause of hemostatic pathology lies in the area of responsibility of the pediatrician.
Classic symptoms of hemorrhagic diathesis in newborns include delayed healing of the umbilical ring with bleeding, nosebleeds, discharge of blood from the genital tract in girls, and the presence of blood in stool and urine. Severe forms of pathology occur with intracerebral and intraventricular hemorrhages, damage to the lungs and gastrointestinal tract.
Possible negative consequences
In addition to anemia, the consequences of HD can be:
- Immune disorders;
- Loss of mobility of one or more parts of the body;
- Loss of vision due to retinal hemorrhages;
- Damage to internal organs, leading to deterioration of their functioning;
- Anemic coma.
This is a serious disease. It is important to see a doctor as soon as possible at the first signs, get diagnosed, and carefully follow the recommendations. If necessary, go to a clinic where you will be provided with the necessary nursing care and timely treatment.
Is it possible to cure diathesis with surgical methods?
Surgery methods in the treatment of diathesis can help restore joint mobility and prevent its fusion. To remove blood from cavities, punctures of the joint, pleura, and pericardium are used. After the blood is removed, a hemostatic drug and antibiotics are introduced into the cavity. Early physical therapy helps prevent immobility.
In cases of massive loss of platelets and red blood cells, the use of splenectomy (removal of the spleen) is considered. This organ is associated with the utilization of cellular elements. Without the spleen, sufficient cell content accumulates in the blood and long-term remission of the disease occurs.
If necessary, vascular prosthetics are performed. When choosing a surgical treatment method, the risk of high blood loss from surgery is always taken into account.
Thus, in hemophilia, to eliminate stiffness, the joint can be replaced with an artificial analogue, but it is unknown how the coagulation system will behave during the intervention. It is not advisable to cause additional bleeding.
Diagnostics
Hemorrhagic diathesis is a variety of diseases with similar symptoms. Moreover, these diseases are very different in etiology, consequences, possible complications, and treatment methods. Therefore, it is very important to correctly make a differential diagnosis. To do this, experts resort to:
- Physical examination. This is necessary to determine the type of hemorrhage and its location. Record the presence or absence of swelling, joint pain, etc.
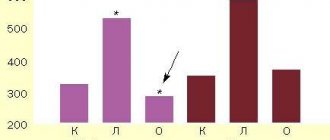
- Laboratory tests. A general blood test can reveal a decrease in the number of red blood cells, platelets, and a drop in hemoglobin levels. Urine and stool analysis is designed to detect hidden hemorrhages, if present. Biochemical blood testing makes it possible to comprehensively assess the parameters of its coagulation.
- Instrumental diagnostics. For example, trepanobiopsy, sternal puncture. These are procedures to obtain a sample of bone marrow to analyze its hematopoietic function.
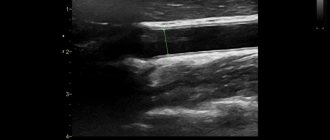
Based on the characteristics of the course of the disease, other diagnostic procedures may be prescribed: Coombs test, functional tests for capillary fragility, kidney ultrasound, liver ultrasound, etc.
To make a correct differential diagnosis, it is desirable to involve specialists of different profiles in the process: immunologist, rheumatologist, hematologist, gynecologist.
HOW TO MAKE AN APPOINTMENT at the PsorMak Institute for Healthy Skin
1. Click the button you see below -
Make an appointment
2. Fill in the fields in the form that appears. Be sure to check the correct phone number so that our specialist can reach you. After filling out, click on the “Submit” button.
3. Wait for our specialist to call. He will answer any of your questions and agree on the date and time of your visit to PsorMak.
The initial appointment includes:
- Visual examination , which will allow the specialist to get a general understanding of the condition of your skin and the pathology itself.
- Collecting anamnesis - finding out information about the development of the disease, living conditions, previous diseases, operations, injuries, chronic pathologies, allergic reactions, heredity, etc. Together with a general examination, this allows you to make a fairly accurate diagnosis and choose a method of treatment and/or prevention.
Treatment
Therapy varies for different diagnoses. We can conditionally combine the medical measures that are resorted to in this case into the following large sections:
Stop bleeding
Before starting treatment, it is necessary to deal with the main symptom - bleeding. For this purpose, tourniquets, pressure bandages, hemostatic sponges, and cold application are used.
Hemocomponent therapy
Those. transfusion of plasma, platelets or red blood cells. Such measures are resorted to only in cases of urgent need, when it is vital to compensate for the deficiency of coagulation factors. May have negative effects on the immune system.
Taking medications
These can be glucocorticoids for thrombocytopathies, vitamins for problems with vascular walls, medications that ensure normal blood clotting. A wide range of drugs are also used to combat the side effects of the main treatment.
Surgical intervention
Appeal to such measures may be due to:
- Repeated massive blood loss;
- Damage to blood vessels due to constant bleeding;
- Damage to joints.
Recommended regimen for using Enterosgel during exacerbation
- First of all, nursing mothers are recommended to take Enterosgel internally themselves to improve the quality of milk (1 tablespoon three times a day);
- A child under one year of age is given Enterosgel (paste) without the “sweet” label immediately before meals, before each feeding;
- For infants up to 6 months: add 2/3 of water or breast milk to 1/3 teaspoon of Enterosgel paste and give before each feeding;
- For children under one year of age Enterosgel: 1/2 teaspoon + ½ teaspoon of water, also before each feeding;
- After a year, Enterosgel is usually given simply 1-2 teaspoons three times a day, added to fruit puree;
- Locally, when it gets wet, periodically apply Enterosgel, diluted with 1/3 of the Tsindol mash, to the affected areas, and alternate this procedure with conventional local remedies.
Prevention
Prevention of hemorrhagic syndrome begins in the maternity hospital. Vitamin K is intended to prevent hemorrhages in premature newborns, administered to babies for the purpose of prevention in a minimal dose (1 mg) immediately after birth.
In order to prevent hemophilia in families where cases of the disease have occurred, future parents should visit a geneticist to calculate the risk of having a sick child.
If there is increased bleeding or taking blood-thinning drugs, the patient is obliged to report these circumstances to dentists, surgeons and other specialists whose actions may lead to bleeding.