Bundle branch block - what is it, why is this condition dangerous?
Bundle branch block is characterized by incomplete or complete blocking of one or two branches simultaneously. The latter is a complete block of the bundle branch, the first is partial.
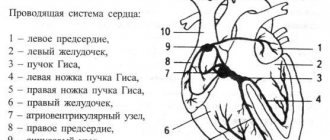
This conduction disorder is intermittent or permanent. The bundle of His consists of the left and right bundle branches. The first is divided into 2 branches: posterior and anterior. Impulses pass through them to the ventricles, after which the latter contract. Any blocking of excitation impulses leads to the development of various types of arrhythmia.
RBBB is not a separate independent disease, but a consequence and electrocardiological manifestation of the underlying cardiac pathology. In patients with age, the detection rate of this disorder increases.
Reasons for the blockade
Bundle branch block can be caused by various reasons.
| Right bundle branch block | occurs in diseases accompanied by overload and hypertrophy of the right ventricle - mitral stenosis, atrial septal defect, tricuspid valve insufficiency, coronary artery disease, cor pulmonale, arterial hypertension, acute myocardial infarction (posterior phrenic or apical), etc. |
| Left bundle branch block | include atherosclerotic cardiosclerosis, aortic valve defects, cardiomyopathy, myocardial infarction, myocarditis, bacterial endocarditis, myocardial dystrophy. Less commonly, bundle branch block develops against the background of pulmonary embolism, hyperkalemia and intoxication with cardiac glycosides. |
The causes of double-bundle blocks are usually aortic defects (aortic insufficiency, aortic stenosis) and coarctation of the aorta.
How dangerous is the condition?
Possible complications of the process:
- Heart failure. The probability with a complete blockade is 70%. In other situations - proportionally lower. Occurs without preliminary symptoms and requires urgent resuscitation.
- Cardiogenic shock. Generalized hemodynamic disturbances. Mortality is maximum, close to 100%.
- Respiratory failure. Up to asphyxia and death in the later stages. It is developing rapidly.
- Heart attack. As a result of insufficient nutrition of cardiac structures.
- Dangerous forms of arrhythmia. Atrial fibrillation or extrasystole. Involves cardiac arrest without the possibility of effective recovery.
- Stroke. Acute malnutrition of cerebral tissues with the formation of a severe neurological defect. Death occurs a little less often.
- Multiple organ failure. As a result of general hemodynamic disorders. The liver and kidneys suffer. The brain is not the least important.
With a significant amount of impairment, the risk of vascular dementia increases—a sharp, severe weakening of mnestic and cognitive functions.
Classification
Depending on the number of elements of the His bundle, in which a violation of the impulse conduction is observed, the blockade occurs:
Single-bundle, when impulse conduction through one element of the His bundle is impaired with blockade:
- right bundle branch;
- anterior branch of the left bundle branch;
- posterior branch of the left bundle branch.
Double-bundle, when the conduction of cardiac impulses along two elements of the His bundle is impaired with blockade:
- anterior and posterior branches of the left bundle branch;
- right leg and anterior branch of the left bundle branch;
- the right bundle and the posterior branch of the left bundle branch.
- Three-bundle with blockade along all elements of the His bundle.
The blockade can be complete or incomplete, constant or intermittent (appears and disappears when recording one ECG), transient (not recorded in the ECG), or alternating (when different legs are blocked when recording one ECG).
Symptoms of complete LBBB
Characterized by the maximum possible clinical picture. It is considered the most severe type of pathological process.
- Constant arrhythmias. As myocardial contractility decreases, the likely scenario is bradycardia with a beat rate of about 40-50 beats per minute, possibly less. In addition to heart rate disturbances, other abnormalities also occur. Group-type extrasystole often occurs, when the left ventricle begins to produce a signal and contract chaotically on its own.
- Chest pain. Non-specific sign. Characterized by mild discomfort. There are no attacks as such, except for cases of coronary insufficiency.
- Shortness of breath during prolonged physical activity or at rest. Depends on the degree of development of the underlying pathological condition. Severe disability is possible with the inability to even serve oneself at home, not to mention professional activities.
- Weakness, feeling of body weakness, periods of apathy. Included in the picture. They represent general manifestations.
- Paleness of the skin.
- Cyanosis of the nasolabial triangle.
- Sweating, especially at night.
- Mental disorders. Like aggressiveness, irritability, long periods of depression or low emotional levels.
- Fainting. May be repeated over the course of one day.
- Headache.
- Vertigo.
- Impossibility of orientation in space.
- Blood pressure surges.
The clinical picture may vary, depending on the underlying diagnosis and the degree of blockage.
Symptoms
Right bundle branch block is asymptomatic and is an incidental finding detected based on the results of an ECG study during a routine medical examination, medical examination or treatment for other diseases. Single-bundle (anterior or posterior) left blockades also do not have clinically significant manifestations.
Left bundle branch block has symptoms of the disease that caused it, most often these are:
- decreased exercise tolerance;
- shortness of breath with slight physical exertion;
- interruptions in heart function;
- palpitations;
- pain in the heart area;
- change in heart sounds during auscultation [weakened or prolonged 1st tone (in 70% of cases), less often (16% of cases) - its splitting, splitting of the 2nd tone (80%)].
Three-fascicle blockade has the most severe clinical manifestations:
- extremely low heart rate – 20–40 beats/min;
- severe shortness of breath at rest;
- interruptions in heart function;
- heart rhythm disturbances;
- dizziness;
- short-term episodes of loss of consciousness;
- cyanosis of the skin.
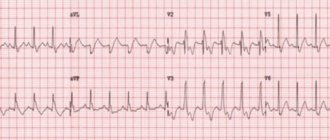
What does bundle branch block look like on an ECG?
ECG signs characterizing a complete block of the right bundle branch include:
- An increase in the duration of the QRS complex beyond 0.120 seconds.
- The presence of a deformed long S wave in leads V4-V6.
- The presence of a three-phase (similar to the letter “M”) QRS in leads V1-V3.
Speaking about the signs of incomplete blockade of the right bundle branch, it is worth noting the absence of a pathologically long QRS complex on the ECG (its length is either normal or is at the upper limit of normal in the range from 0.090 to 0.110 seconds), but the presence of triphasicity when visually assessing the shape of the ventricular complexes.
Visual signs of complete (affecting both branches) blockade of the left leg on the ECG include:
- There may be a prolongation of the ventricular complex beyond 0.120 seconds.
- The presence of deep long S waves in leads V4-V6.
- The presence of long and deformed R waves in leads I, aVL and V5-V6.
- Absence of Q on graphs I, V5-V6.
The blockade of the anterior branch of the left bundle branch of His looks like this:
- A pronounced deviation of the heart axis to the left side (from -30 to -90 degrees).
- Ventricular complex of normal duration.
- Small R waves combined with deep S waves in II, III and aVF.
- Small Q waves in I and aVL.
Blockade of the posterior branch of the left leg of His looks like:
- A pronounced deviation of the heart axis to the right side (from +120 to +180 degrees).
- Ventricular complex of normal duration.
- Small Q waves in combination with high-amplitude R waves in II, III and aVF.
- Small R waves in I and aVL.
If the above-mentioned signs that fit the description of a blockade of the legs are detected on the ECG, the doctor must identify the root cause of this rhythm disturbance and make a diagnosis in accordance with government recommendations, and consider the blockade itself to be a manifestation of the disease.
Left bundle branch block
Right bundle branch block
Blockade of the right leg together with the left posterior branch of the His bundle
Severity
Staging of the pathological process has not been developed with sufficient accuracy. Based on the national recommendations of individual communities, we can talk about four degrees of severity of the blockade:
| Degree | Description |
| First or easy. | There is a conduction disturbance in one leg. There are no symptoms at all, a minimal nonspecific clinical picture is possible. Typically, this stage corresponds to the initial forms of cardiac diseases. |
| Second, moderate. | The block affects one or two bundles of the left bundle branch. The severity of the symptoms is sufficient to consult a doctor. Usually, disorders are diagnosed at this stage, but not always. The prospects for a cure are still good. |
| Third, heavy. | Complete blockades are noted. The symptoms are painful for the patient, and the quality of life decreases significantly. High risk of death. Organic deviations from remote systems are observed. Recovery is carried out urgently, in a hospital setting. |
| Fourth or terminal. | It is provoked by a long course of both the underlying disease and the blockade. The treatment is ineffective and there are no prospects. Palliative care is possible. |
In order not to miss the moment, it is recommended that at the first suspicion you go to a cardiologist or at least a therapist.
Consequences
Bundle branch block requires timely diagnosis, since if left untreated, the disease causes serious consequences, sometimes incompatible with the patient’s life. Among them are:
- tachycardia;
- ventricular fibrillation;
- thromboembolism;
- heart failure;
- heart attack;
- stroke;
- sudden death.
To prevent these complications, it is recommended to undergo regular preventive medical examinations. If heart pain, shortness of breath and other signs of the disease appear, you should contact a specialist immediately.
Treatment for bundle branch block
Treatment of the pathology depends on the type and electrocardiographic indicators at the time of diagnosis. Special treatment for damage to the right bundle branch is most often not required. In this case, the patient is recommended to follow measures aimed at preventing complications of the pathology.
To do this, the patient should adhere to the following rules:
- harden, douse yourself with cold water;
- respond adequately to stress;
- introduce teas into the diet, including soothing herbs (valerian, motherwort, elderberry, linden, nettle, oregano);
- give up heavy physical work and strength sports;
- maintain proper nutrition, avoid foods that increase cholesterol levels in the blood;
- exclude fatty, spicy, fried, smoked foods, mayonnaise, sauces, marinades, ketchups.
There is no specific drug treatment for this conduction disorder. Patients with right bundle branch block in the absence of an underlying disease do not require treatment. For patients with single- or double-fascicular blockade, the following groups of drugs can be prescribed for the treatment of the underlying disease:
- antioxidants – ubiquinone, carnitine, mexidol, preductal;
- vitamins – thiamine (vitamin B1) with lipoic acid, riboflavin (vitamin B2), nicotinic acid (vitamin PP);
- sedatives of plant origin (St. John's wort, motherwort, valerian, sage);
- antiplatelet agents to prevent thrombus formation in the heart and blood vessels - aspirin, cardiomagnyl, thrombo Ass;
- lipid-lowering drugs to normalize cholesterol levels - statins (rosuvastatin, atorvastatin, simvastatin);
- ananginal drugs for the treatment of coronary heart disease - short- and long-acting nitrates (nitroglycerin, isoket, cardiquet, monocinque);
- drugs for the treatment of diseases of the bronchopulmonary system that have caused the development of pulmonary heart disease - inhaled adrenomimetics and glucocorticosteroids (Berotec, Berodual, Spiriva, Beclazone);
- antihypertensive drugs for the treatment of arterial hypertension - ACE inhibitors (perindopril, lisinopril), angiotensinogen II receptor antagonists (losartan, valsartan), beta blockers (bisoprolol, atenolol), calcium channel antagonists (amlodipine, verapamil). The last two groups should be prescribed with caution, as they reduce the heart rate;
- antibiotics, non-steroidal anti-inflammatory drugs for inflammation of the membranes of the heart - penicillin; nimesulide, diclofenac;
- diuretics and cardiac glycosides in the development of chronic heart failure - indapamide, diuver, lasix; strophanthin, digoxin.
In addition to medication, a surgical method of blockade treatment is used, which consists of installing a pacemaker (pacemaker) in the patient. Complete right blockade, especially in combination with left hemiblockade (blockade of one branch of the left leg), and complete left blockade, developed in the acute period of myocardial infarction (10 - 14 days), are an indication for temporary cardiac pacing by introducing an electrode through the central vein into the right ventricle
Three-fascicle blockade with complete atrioventricular block, a rare rhythm of ventricular contractions and with Morgagni-Edams-Stokes attacks (attacks of loss of consciousness) is an indication for permanent cardiac pacing (implantation of an artificial pacemaker or cardioverter-defibrillator).
Forecast
In conclusion, it should be said that bundle branch block is not a disease, but symptoms of heart disease that can manifest themselves clinically or be detected on an ECG. It is necessary to take into account the causes of the blockade, prescribe adequate treatment, and in this case it is possible to assume the consequences of a particular blockade.
If the patient has a single-fascicle right block and there are no pathologies of the heart and lungs, we can talk about a favorable prognosis.
An unfavorable prognosis in the case of a complete block of the left leg due to myocardial infarction, since in this case the mortality rate is 40-50 cases out of 100. In cases where the block is three-fascicle, there is a high probability of developing asystole and the prognosis is also unfavorable.
Diagnostics
The diagnosis of bundle branch block can be established on the basis of a general examination, palpation of the pulse, auscultation (listening) of the heart, general and biochemical blood and urine tests, and analysis of hormonal status - it can reveal causes of blockage not related to heart disease. To make a diagnosis, you will also need electrocardiography (ECG) data, which allows you to identify changes characteristic of each type of blockade. Also necessary are indicators of daily ECG monitoring (Holter monitoring) - a diagnostic procedure that involves the patient wearing a portable ECG device throughout the day. At the same time, a diary is kept in which all the patient’s actions are recorded (getting up, eating, physical activity, emotional anxiety, deterioration in health, going to bed, waking up at night). ECG and diary data are compared, thus identifying intermittent cardiac conduction disturbances associated with physical activity, food intake, stress, or night blockades. Data from an electrophysiological study (stimulation of the heart with small electrical impulses with simultaneous recording of an ECG) can be informative. The procedure is performed through the esophagus (the electrode is inserted through the esophagus; only the atria can be stimulated) or invasively (the electrode is inserted into the heart cavity by inserting a special catheter through a large blood vessel). It is used in cases where ECG results do not provide unambiguous information about the type of blockade, fainting, and also to assess the condition of the conduction system of the heart. Ultrasound examination of the heart can identify cardiac causes of blockade.
Prevention
Preventive measures include:
- avoidance of stressful situations;
- giving up alcohol and smoking;
- daily routine, full and restful sleep;
- refusal of fried, canned and spicy foods;
- taking medications only prescribed by a doctor and under his supervision;
- consumption of foods with a significant fiber content: fresh fruits and vegetables, herbs;
- timely diagnosis and treatment of diseases of all organs, not just the heart;
- mandatory consultation with a doctor if symptoms of the disease appear.
If an operation has been performed to install a pacemaker, a person should exclude the influence of electrical devices and a mobile phone on him. If you become ill, it is important to visit your doctor in a timely manner to assess the condition of the heart and the general well-being of the patient.