Arterial hypertension. Relevance
Information
About the locations of the republican medical and educational campaign
“A healthy heart means a successful future”
| No. | Health care institution | Location | Address | Date tested | Responsible |
| 1 | Healthcare institution "9th city clinic" | Pharmacy No. 25 | St. O. Koshevoy -10 | 26.05.2016 | Rud Olga Semyonovna Acting head of the OMP t. 398-94-81 |
| 2 | Healthcare institution "9th city clinic" | MOH | St. Radial, 7 | 26.05 .2016 | Kastenkova Galina Petrovna paramedic at the health center t. 296-00-22 |
| 3 | Healthcare institution "9th city clinic" | Trolleybus Park No. 5 State Enterprise "Minsktrans" | St. Soltysa 26 | 26.05.2016 | Matyushenko Maria Vyacheslavovna paramedic at the health center t. 246-59-74 |
| 4 | Healthcare institution "9th city clinic" | UE "MGMC" | St. Dolgobrodskaya, 41 | 26.052016 | Shitikova Nina Ivanovna paramedic at the health center t. 230-57-03 |
| 5 | Healthcare institution "9th city clinic" | State Institution “Department Store Start “X” | Dolgobrodskaya street, 26 | 26.05.2016 | Parmon Irina Frantsevna valeologist 9GP t. 398-94-81 |
The qualitative component of a person’s life, his longevity and preservation of working capacity are directly related to the functional activity of the cardiovascular system, the accumulated “baggage” of diseases affecting the heart and blood vessels. The greatest contribution to premature mortality of the population is made by: arterial hypertension, hypercholesterolemia, smoking, insufficient consumption of vegetables and fruits, excess body weight, excess alcohol consumption and physical inactivity.
Arterial hypertension is the most common controllable factor in cardiovascular morbidity and mortality in most countries of the world. About half of the cases of myocardial infarction and about 80% of stroke cases are associated with high blood pressure, which determines the high socio-medical significance of measures aimed at lowering blood pressure. European experts predict that by 2025, 29.0% of men and 29.5% of women worldwide will have hypertension, but the prevalence may vary significantly in different regions of Europe and the world.
It is known that the incidence of death from stroke and coronary heart disease increases progressively and linearly, starting from a blood pressure level of 115/75 mm Hg. in the age group 40-80 years. For every 20 mm Hg. increase in systolic blood pressure or 10 mm Hg. An increase in diastolic blood pressure from the indicated figures increases mortality from coronary heart disease and stroke by 2 times.
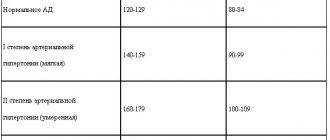
Arterial hypertension is a chronic stable increase in blood pressure, in which systolic blood pressure is 140 mmHg. or higher and/or diastolic blood pressure equal to 90 mmHg. or higher.
It should be kept in mind that when visiting a doctor, the diagnosis of arterial hypertension is based on data from at least two measurements of office blood pressure, during at least two visits with an interval of 1-2 weeks. If the patient's blood pressure is ≥180/110 mmHg. The diagnosis of arterial hypertension can be established during the first visit. The doctor’s tactics depend on the detected blood pressure level.
In the city of Minsk, the detection of people with arterial hypertension increased from 22.4% in 2008. up to 31.9% in 2013. The share of uncomplicated arterial hypertension in the structure of newly diagnosed arterial hypertension was 37.8%.
Structure of newly diagnosed arterial hypertension:
- essential (primary) arterial hypertension - 96.1%, a decrease of 0.3% (2012 - 96.4%);
- symptomatic arterial hypertension (against the background of diseases of other organs and systems) - 3.9%, an increase of 8.3% (2012 - 3.6%).
The low proportion of symptomatic arterial hypertension in the structure is due to insufficient detection of this pathology, which is associated primarily with the complexity of diagnosis.
It is known that arterial hypertension is asymptomatic for many years and one of the first manifestations of the disease can be a life-threatening complication (heart attack, stroke).
In 2013, 3,292 cases of myocardial infarction were registered among patients with arterial hypertension in the city of Minsk. 210 patients (6.4%) died from acute myocardial infarction. In 3619 cases, acute cerebrovascular accidents developed in patients with arterial hypertension. Lethal acute cerebrovascular accidents 1083 cases (29.9%). 1867 patients died from other complications of arterial hypertension, and in 2012 - 1642 patients.
Arterial hypertension: misconception and truth.
Misconception: There is “working pressure”, and if it is elevated, then there is no need to reduce it.
Truth: There is no such thing as “working pressure.” If a patient, while measuring his blood pressure, finds at least twice that the numbers are greater than 140/90 mmHg, then with a high degree of probability this means that he has arterial hypertension. In this case, it is necessary to clarify the diagnosis with a doctor.
Misconception: if nothing bothers you, then there is no arterial hypertension.
Truth: Hypertension is called the “silent killer.” The insidiousness of the disease lies precisely in the fact that it can occur unnoticed by the patient himself. Even if there are no complaints, high blood pressure (without treatment) inevitably has a destructive effect on the “target organs”: heart, kidneys, blood vessels, brain. Thus, without measuring blood pressure it is impossible to determine the disease. It is important to measure your blood pressure even if you feel well.
Misconception: If blood pressure has returned to normal, drug therapy should be discontinued.
Truth: the goal of treating arterial hypertension is not just to reduce blood pressure numbers, but also to prevent adverse consequences (heart attack, stroke, kidney failure) and also to protect target organs. Since arterial hypertension is a chronic disease, if drug therapy is discontinued, blood pressure will increase again, which can lead to complications such as heart attack and/or stroke. Antihypertensive drugs are not intended for a course of treatment. Only constant use of medications provides a lasting therapeutic effect.
Misconception: You can choose medications to lower blood pressure on your own.
Truth: even with the same pressure values in different people, treatment should be selected strictly individually. The choice of drug is made by the doctor taking into account the level of increase in blood pressure, the presence of concomitant diseases, risk factors, possible interactions with other medications that the patient is taking, as well as the presence of contraindications to the prescription of this drug.
Misconception: Arterial hypertension is a disease of older people.
Truth: Arterial hypertension has become “younger” in recent years. People who have barely reached the age of 30 suffer from high blood pressure. And in young people the disease can take more severe forms.
Arterial hypertension develops according to its own laws, regardless of whether the patient knows about it or not: over time, an increase in the mass of the heart occurs - hypertrophy, the walls of blood vessels lose their elasticity and thicken, and their lumen narrows, as a result of which less and less blood flows to the organs and tissues. Atherosclerosis develops at an accelerated pace, which further impairs the blood supply to organs. First of all, the so-called “target organs” are affected: the brain, heart, kidneys, retina. Against the background of long-term arterial hypertension, various mechanisms of development of not only acute, but also chronic forms of cerebrovascular pathology are realized, leading to severe cognitive impairment up to dementia.
Thus, arterial hypertension requires a very disciplined and responsible approach to fulfilling prescriptions and the patient’s attitude towards strict normalization of blood pressure. Even the best doctor will not be able to effectively combat hypertension if the patient is not interested in it. Keeping patients informed about their illness will not only prolong years of activity, it can even save lives.
Treatment of arterial hypertension.
What is the modern treatment of arterial hypertension? There are two groups of treatment methods – non-drug and medicinal.
The non-drug method involves measures aimed at combating risk factors (lifestyle modification). Appropriate lifestyle changes are important, although lifestyle changes should never be a reason to delay drug therapy in high-risk patients.
Recommended lifestyle changes with proven blood pressure-lowering effects include limiting salt, high consumption of vegetables and fruits, low-fat and other diets, losing and maintaining weight, and regular exercise. In addition, a strong recommendation to quit smoking is absolutely mandatory.
Preventing excess weight or reducing existing weight is an important goal. Weight loss is strongly recommended for obese individuals (body mass index greater than 30 kg/m2) and overweight individuals (body mass index greater than 25 and less than 30 kg/m2), as well as patients with increased abdominal adipose tissue, as measured by circumference waist (for men – more than 102 cm, for women – more than 88 cm).
Food should be varied and energy intake should be optimal to maintain ideal weight. In your diet, it is recommended to limit the consumption of animal products rich in cholesterol and saturated fat. These products include: fatty meats, lard, butter, sour cream, egg yolk, fatty cheese, sausage, sausages, all offal. It is recommended to replace animal fat with vegetable fat, since the latter is rich in anti-atherogenic unsaturated fats.
Another important principle of nutrition is to increase the consumption of plant-based foods that can bind and remove cholesterol from the body. Recommended to use:
- dietary fiber (at least 30 g per day). They are found in large quantities in fruits (pears, apples, oranges, peaches), berries (raspberries, strawberries, blueberries), vegetables (cauliflower, broccoli, green beans), legumes (peas, lentils, beans);
- pectins (at least 15 g per day). Contained in fresh fruits (apples, plums, apricots, peaches), berries (black currants), vegetables (carrots, beets).
There is evidence of a cause-and-effect relationship between salt intake and blood pressure. In addition, excess salt intake may play a role in the development of resistant hypertension. You should limit your daily salt intake. This can be achieved if you salt your food less and avoid eating canned food, semi-finished products, and fast food products.
In the non-drug treatment of arterial hypertension, physical exercise plays a very important role. It is necessary to exercise at least 3 times a week for an hour. Before starting exercise, you should consult with a cardiologist who can recommend a set of approved exercises for each patient. It is necessary to start classes gradually, very slowly increasing the load.
It is extremely important to convince the patient to stop any form of smoking, using all the necessary arguments. Quitting smoking for two years reduces the risk of coronary death by 36% and non-fatal myocardial infarction by 32%.
There are 5 principles that will help you cope with the difficult task of quitting your addiction to tobacco:
- ask – systematically identify smokers (at every call);
- assess – determine the patient’s degree of addiction and his readiness to quit smoking;
- advise - convince all smokers to categorically quit smoking;
- help – promote a smoking cessation strategy, including advice on lifestyle changes, nicotine replacement therapy and/or pharmacological intervention;
- long-term monitoring, with mandatory regular visits to the doctor by the smoking patient.
Currently, there are many antihypertensive drugs: diuretics (indapamide, hydrochlorothiazide), ACE inhibitors (lisinopril, ramipril, perindopril), calcium ion antagonists (amlodipine, nefidipine), beta blockers (bisorolol, metoprolol, carvedilol), angiotensin receptor antagonists (losartan, irbesartan, valsartan), combinations of various drugs in one tablet, others. Their effectiveness has been proven by studies conducted in different countries of the world. Modern manufacturers produce drugs that meet the principle of maximum convenience for humans - one, maximum two doses of one tablet per day. There are depot drugs (the names contain the letters R, XL, SR), they do not act sharply, but are released into the blood gradually and over a long period of time so that the concentration of the drug remains constant for 12-24 hours to prevent a rise in blood pressure. It is rational to use combinations of fixed doses of two antihypertensive drugs in one tablet, since reducing the number of tablets that the patient must take daily improves adherence to treatment (which, unfortunately, is low in hypertension) and improves blood pressure control.
The choice of drug is made taking into account the level of increase in blood pressure, the presence of other diseases, risk factors, possible interactions with other drugs, and the presence of contraindications. Finding the right treatment may take some time and several appointments with your doctor.
Arterial hypertension requires a very disciplined and responsible approach to fulfilling prescriptions and the person’s attitude towards strict normalization of blood pressure. It is important to know that the concept of “working pressure” does not exist. The main thing is to take your medications constantly and regularly.
New views on arterial HYPERTENSION
At the end of the twentieth century, many positions on hypertension that were considered unshakable for many years were subjected to critical revision. New epidemiological data, new results from clinical trials and new evidence-based international standards have essentially challenged traditional ideas about hypertension. As a result, over the past 5-10 years, very significant changes have occurred in views on the origin, diagnosis and treatment of hypertension.
Etiology and pathogenesis of hypertension
First of all, it is worth noting the final recognition of the polygenic nature of essential hypertension, which means the need to consider it not only as a disease of chronically elevated blood pressure, but also as a complex set of interrelated hemodynamic, metabolic, and neurohumoral disorders. The following, modified illustration of Page's mosaic theory (Fig. 1), demonstrates modern understanding of the main pathogenetic mechanisms of hypertension. The practical significance of this scheme is to demonstrate the difficulty of selecting a single, even the most modern, drug that corrects disorders in all these mechanisms. It should be borne in mind the possibility of transformation of the disease from one variant to another, both as it progresses and under the influence of drugs. Looking ahead, we will say that this scheme confirms the need for combined antihypertensive therapy in most patients. The situation remains problematic, and despite the fact that we know a lot about the mechanisms involved, we do not have prognostic criteria to determine the path along which the development of hypertension will take place in a particular patient. Great hopes are associated with studying the genetic aspects of hypertension. Rare monogenic forms of hypertension have been identified. As for essential hypertension or hypertension, the most documented role of the genes of the renin-angiotensin system, in particular the angiotensinogen gene and its receptor, the ACE gene. Alleles 6A and 235T of the angiotensinogen genes are parameters used in a number of countries to determine genetic predisposition to hypertension.
| Figure 1. Mosaic theory of the pathogenesis of hypertension |
The α-aducine gene, the insulin receptor gene, and the transforming growth factor 1 gene are also significant. Noticeable advances have been made in gene therapy of experimental hypertension.
Next up is the epidemic of the metabolic variant of hypertension, also known as the “deadly quartet” or “modern lifestyle syndrome.” The main reason for this epidemic, as is clear from the latest definition, lies in the modern lifestyle with a decrease in physical activity and poor nutrition. This determines the extreme relevance of primary prevention of hypertension. Along with the “old” ones, so-called new metabolic risk factors are being actively discussed today. These include: uric acid, endogenous tissue plasminogen activator, estrogen deficiency, homocysteine, fibrinogen, coagulation factor VII, d-dimer, lipoprotein (a), C-reactive protein. Relatively new hemodynamic risk factors attract no less attention due to their significant role not only in the development of hypertension, but especially in the formation of its complications - for example, the higher the heart rate, the worse the prognosis. Experimental studies suggest the possibility of this exposure being atherogenic as a result of increased vascular stress. Pulse pressure is increasingly considered as one of the most informative integral indicators of blood pressure, especially in the elderly; and with the introduction of the method of 24-hour blood pressure monitoring, indicators such as blood pressure variability and nocturnal hypertension became available. Increased blood pressure variability and the lack of proper nocturnal blood pressure reduction means an accelerated rate of target organ damage and the approach of dangerous cardiovascular complications of hypertension. These factors retain their unfavorable significance even with normalized average blood pressure values. Speaking about what is new in the pathogenesis of hypertension, it should be noted that the focus has shifted from resistive arteries to large main vessels with the study of their distensibility/elasticity. Nowadays, the significant role of the endothelium and nitric oxide in the genesis of cardiovascular complications associated with hypertension is recognized. At the same time, increasing importance is being attached to the vascular endothelium and the search for drug effects on its impaired function. It is no coincidence that the vascular endothelium is considered, on the one hand, as the earliest target organ affected by hypertension, and on the other, as a source of increased blood pressure as such. Its main function is to maintain a balanced state of opposing processes, which regulates the state of the mechanisms that ultimately determine the progression of complications. This is vascular tone, synthesis and inhibition of growth factors, nonspecific inflammation, which determines the prognosis of hypertensive vasculopathy, and a significant effect on hemostasis and thrombolysis. Today, the alternative concept of the pathogenesis of hypertension, promoted in our country by Professor G. G. Arabidze, is sounding more and more convincing. According to this concept, the progression of essential hypertension is based on an imbalance between angiotensin 2 and nitric oxide with an excess of the former and/or a deficiency of the latter. When discussing modern views on the pathogenesis of hypertension, special attention should be paid to recognizing the role of nonspecific inflammation in the progression of hypertensive vasculopathy.
Blood pressure indicators
A new approach to the problem of hypertension is also associated with a change in views on blood pressure indicators. Within the framework of traditional concepts, hypertension was considered as a disease with a clear pathophysiological determinant in the form of an increased peripheral vascular resistance. The level of DBP was considered a sensitive marker of increased BPSS, which for many years dominated as a diagnostic criterion for the severity of hypertension and an indicator of the effectiveness of treatment. The introduction of the sphygmomanometry method into clinical practice at the beginning of the century - an outstanding discovery of its time - for many years narrowed the view of hypertension to blood pressure numbers. At the present stage of studying hypertension, the emphasis is on the levels of systolic blood pressure and pulse pressure (PP). The Framingham study put an end to ideas about the harmlessness of increasing SBP with age. Later, data on the high predictive value of SBP were confirmed in the SHEP and MRFIT studies. The validity of ideas about the harmlessness of low DBP levels is questionable. A recent analysis of the Framingham Study database revealed an inverse association between the incidence of cardiovascular events and DBP at any SBP level. An independent risk factor is PD. Its influence is especially pronounced in relation to coronary events and heart failure. Increased PP is also associated with a higher incidence of coronary atherosclerosis, strokes, lacunar infarctions, vascular dementia, and chronic renal failure. New versions of old techniques are used to measure PD. Next is the absence of age-specific blood pressure norms. Today we are talking about uniform blood pressure standards for adult patients. Traditionally, it is believed that the most difficult task is to correct the level of DBP, but as a result of large controlled studies, it turned out that SBP is more important. The benefits and safety of a significant reduction in high blood pressure have been proven. The HOT study convincingly demonstrated that in order to significantly reduce the risk of cardiovascular complications and truly solve the problem of antihypertensive therapy, the pressure must be reduced not by 10-12 mm Hg. Art., as we usually do, and to the target level, that is, 26-30 mm Hg. Art. The benefits and safety of treatment of hypertension and isolated systolic hypertension in the elderly and senile have been proven.
Target BP
Despite the apparent reduction in morbidity and mortality among treated patients with hypertension, the rates of cardiovascular morbidity and mortality in this group exceed those in normotensive individuals. This explains the recommendation for mandatory achievement of target blood pressure (Table 1). Target, or required, blood pressure is an innovation that significantly distinguishes modern standards of antihypertensive therapy. What can we say firmly and unambiguously? That the desired level of target pressure in the presence of concomitant diabetes mellitus should be less than 130/85 mm Hg. Art. and an even more pronounced decrease in the presence of chronic renal failure or severe proteinuria. But the issue with target blood pressure in uncomplicated forms of hypertension is not so simple, for which there is no data on the advisability of lowering blood pressure below the level of 140-150/90 mmHg. Art. Additional analysis of the Hypertension Optimal Treatment (HOT) trial, which has been highly debated and has become the basis for current recommendations to lower blood pressure below 135/85 mmHg. Art., did not confirm the beneficial effects of this level of achieved blood pressure in patients without diabetes mellitus. When we re-analyze and divide patients into two groups - with diabetes and without diabetes - we see that while there is a clear benefit in the group of patients with diabetes in terms of cardiovascular mortality and overall mortality, the dynamics in the group of patients without diabetes are the opposite, although statistically inaccurate direction. Therefore, today it makes more sense (safer) to talk about a target pressure of no lower than 140/90 mm. Hg Art. in uncomplicated cases of hypertension.
Diagnostic methods
Changing views on the nature of the disease and the mechanisms of its pathogenesis have contributed to the expansion of the diagnostic spectrum that we must use for a comprehensive assessment of a patient with hypertension. The method of 24-hour blood pressure monitoring has become firmly established in clinical practice. Modern standards define indications when this method is mandatory: high blood pressure variability, suspicion of white coat hypertension, symptoms of hypotension, refractory hypertension. For this method, standard indicators are clearly defined. In connection with the shift of interest from resistive vessels to main ones, there is a return at a new level to old, previously widely used diagnostic methods, such as measuring the velocity of pulse wave propagation and measuring central pulse pressure.
Hypertension and the practice of evidence-based medicine
The gold standard for informed approaches is the evidence base from multicenter clinical trials. In recent years, many large studies in hypertensiology have been completed, including those comparing traditional drugs (diuretics and β-blockers) with “new” classes of antihypertensive drugs.
In the history of “evidence-based hypertensiology”, three main periods can be distinguished: the 60-70s - the “golden” period, which gave a complete understanding of traditional drugs, including data on the effect of diuretics and β-blockers on endpoints; the subsequent 20 years - a “period of stagnation”, when, despite active clinical use, there was no data on the effect of ACE inhibitors and calcium antagonists on the end points; in 1995, the so-called “renaissance period” began, when about 40 major studies were launched to answer the most pressing questions of clinical hypertensiology.
Over the past five years, a number of large studies have been completed (Table 2). The long-acting dihydropyridine calcium antagonist nisoldipine has been demonstrated to be of value in the treatment of this common form of hypertension. As a result, this class of drugs, along with diuretics, is considered to be the drug of choice for the treatment of hypertension in old age. The use of lisinopril is also effective in treating this group of patients. This drug is effective in obese patients, as confirmed by the TROPHY study, and it also slows the progression of retinopathy (EUCLID study). Data from the EUCLID study also suggest that lisinopril reduces microalbuminuria (the study compares lisinopril and nifedipine). The HOT study demonstrated the value and feasibility of achieving target blood pressure, the need for a combined regimen of antihypertensive drugs, and the rationale for using low-dose aspirin in patients with normalized blood pressure for the primary prevention of coronary artery disease. The CAPPP, UKPDS LIVE STOP-HYPERTENSION 2 studies confirmed the high clinical value of traditional antihypertensive drugs compared to new ones. In addition, the following was established: the high value of ACE inhibitors for slowing the progression of complications of hypertension in diabetes mellitus (CAPPP), the paramount importance of normalizing blood pressure (exceeding the value of normoglycemia) to prevent the development of micro- and macrovascular complications of diabetes mellitus (UKPDS); advantages of the diuretic indapamide retard over the ACE inhibitor enalapril in the regression of left ventricular hypertrophy (LIVE); the feasibility of treating hypertension in the elderly using all major classes of antihypertensive drugs (STOP-HYPERTENSION 2).
High risk groups
As a result of epidemiological and controlled clinical studies, it became obvious: the higher the risk of developing cardiovascular complications in hypertension, the greater the benefit from rational, usually individually selected, antihypertensive therapy. As a result, the concept of high-risk groups and the so-called risk strategy emerged, based on individual selection of drugs in accordance with the individual spectrum of risk factors. Problem groups with a high risk of developing complications include: hypertension with kidney damage; hypertension in the elderly; hypertension in diabetes mellitus; hypertension in menopausal women; Hypertension and dyslipidemia. The increase in the incidence of chronic renal failure, including with treated hypertension, is one of the unresolved issues of modern hypertensiology. It has been established that the level of creatinine and the degree of proteinuria are the most valuable prognostic markers of the degree of risk of developing cardiovascular complications. Microalbuminuria has traditionally been considered a marker of renal involvement, while current data convincingly demonstrate that this indicator sensitively reflects both the degree of generalized microvascular damage and the degree of overall risk. This is evidenced by the close positive relationship between microalbuminuria and damage to the main target organs in arterial hypertension (Fig. 2).
| Figure 2. Microalbuminuria is an independent risk factor for cardiovascular complications |
Left ventricular hypertrophy is an independent powerful risk factor that significantly worsens the prognosis of hypertension. The data are encouraging that the implementation of a national program to combat hypertension in the United States, against the backdrop of a significant increase in the frequency of use of antihypertensive drugs, led to a significant decrease in both the prevalence of hypertension and LV hypertrophy in the population. The prevalence of LVH based on ECG criteria was almost halved. However, with regard to the group of patients with hypertension and LVH, the following questions have not yet been resolved: which class of drugs is most effective for regression of LVH; what factors determine regression of LVH (obviously there is no parallelism between the degree of blood pressure reduction and regression of LVH); what is the long-term benefit of regression of LVH; What is the reason for the increase in the incidence of heart failure in patients with hypertension?
The main attention in the practical activity of a doctor - due to the very high risk of complications - should be directed to the group of patients with hypertension and non-insulin-dependent diabetes mellitus. Already a slight increase in blood pressure to the so-called “normal high blood pressure” (SBP 130-139 and/or DBP 85-89 mm Hg) is the basis for drug therapy. In this group, aggressive treatment is indicated to achieve a target blood pressure of less than 130/85 mm. Hg Art. More and more data are accumulating on the benefits of ACE inhibitors in diabetes mellitus and hypertension, but in general the question of first-choice drugs in this large group of patients remains open. The question of the appropriateness of using calcium antagonists in this group is currently widely debated. On the one hand, there is data calling into question the safety of the use of now long-acting dihydropyridine calcium antagonists (ABCD, FACET, MIDAS studies), on the other hand, a significantly larger database in terms of volume and duration of observation obtained in the NOT, INSIGHT and SystEur studies does not confirmed these concerns and demonstrated the safety and high effectiveness of the use of drugs from this group. We will receive the final answer in the foreseeable future, when such major studies as ALLHAT, ASCOT, VALUE are completed.
New WHO-IAS recommendations
New WHO-IAS recommendations were adopted in January 1999. What are their fundamental distinguishing features? For the first time in many years, the fundamental positions of various international standards on hypertension have been agreed upon, a move away from the staged and qualitative approach has occurred, and patient stratification according to risk level has been introduced. Why should we, along with the blood pressure level, necessarily take into account the degree of risk? The more risk factors, the worse the prognosis for a patient with hypertension. With the same blood pressure level, but in the presence of risk factors, the occurrence of severe complications is approximately 20 times more likely than without these factors, while significantly different blood pressure levels with the same range of risk factors lead to complications only two to three times more often.
The emphasis on rational low-dose therapy is practically important. It has been shown that normalization of blood pressure requires an average of three to five medications in approximately three-quarters of patients. It has been established that all six classes of modern antihypertensive drugs effectively reduce blood pressure as monotherapy in only half of the cases. The HOT study demonstrated that 75% of patients required combination antihypertensive therapy to achieve target blood pressure.
Is this data new? In general, no. Having analyzed the database that we refer to when discussing the problem of hypertension, one can see that in most studies the frequency of combination therapy is very high (Fig. 3).
| Figure 3. Frequency of combination antihypertensive therapy |
Rational combination is based on compliance with two principles: drugs with different mechanisms of action and with a different spectrum of influence on tolerability should be prescribed. In table Table 1 shows rational, less rational and irrational combinations of antihypertensive drugs.
The objectives of antihypertensive therapy have undergone a significant evolution, and from the standpoint of current knowledge, it is necessary not only to reduce blood pressure, but also to influence the mechanisms of disease progression. The greatest hopes for solving this problem are associated with the class of drugs that affect the renin-angiotensin-aldosterone system.
Principles of drug therapy
What changed? When prescribing treatment, they are based on the degree of risk, and not just on the level of blood pressure. The choice of drug to initiate therapy should be made from six classes, including angiotensin-2 receptor antagonists. The tactics of step-by-step prescription of drugs gave way to liberal tactics or individual choice of antihypertensive drugs. Modern standards clearly define the criteria for the preferential class selection of drugs. Hopes for the next decades are associated with the active study of two classes of drugs: angiotensin-2 receptor antagonists and vasopeptidase inhibitors.
Despite significant progress in our knowledge of hypertension, many controversial and unresolved issues remain in clinical hypertensiology. Let's list some of them. Is it rational to start drug therapy for high normal blood pressure? Is it advisable to reduce diastolic pressure below 90 mm? Hg Art. in patients without diabetes? Is the reduction in cardiovascular morbidity and mortality caused by agents that block the renin-angiotensin-aldosterone system independent of blood pressure, as suggested by the HOPE study? Are there class-specific organoprotective effects? Is it reasonable to extrapolate data for individual drugs to group and class characteristics? Do new drug classes have additional impact on hard endpoints? Does antihypertensive therapy cause dementia? What is the carcinogenicity of antihypertensive drugs?
Etiology and pathogenesis of hypertension
- Recognition of the polygenic nature of hypertension
- Epidemic of metabolic variant hypertension
- New metabolic risk factors
- New hemodynamic risk factors - heart rate - pulse pressure - blood pressure variability - nocturnal hypertension
- Genetic determinants of hypertension
- Shifting focus from resistive vessels to main ones
- Recognition of the significant role of the endothelium and nitric oxide in the genesis of cardiovascular complications
- Recognition of the role of nonspecific inflammation in the progression of hypertensive vasculopathy
Combined antihypertensive therapy
Rational combination
- Diuretic + β-blocker
- Diuretic + ACE inhibitor
- ACEI + calcium antagonist
- β-blocker + calcium antagonist
- β-blocker + α1-blocker
Less rational combinations
- Calcium antagonist + diuretic
- β-blocker + ACE inhibitor
Irrational combinations
- β-blocker + calcium antagonist such as verapamil or diltiazem
- Calcium antagonist + α1 blocker
Endothelium: the main function is to maintain an equilibrium state of opposing processes
VASCULAR TONE
Vasodilators
- Nitric oxide
- Hyperpolarizing factor
- Prostacyclin
- C-type Na-uretic peptide
Vasoconstrictors
- Endothelin
- Angiotensin II
- Thromboxane A2
- Prostaglandin H2
GROWTH FACTORS
Stimulants
- Superoxide radicals
- Endothelin
- Angiotensin II
Inhibitors
- Nitric oxide
- Prostacyclin
- C-type Na-uretic peptide
INFLAMMATION
Stimulants
- Superoxide radicals
- TNF-A
Inhibitors
- Nitric oxide
HEMOSTASIS AND THROMBOLYSIS
Prothrombotic
- Inhibitor activator
- Plasminogen
Antithrombotic
- Tissue activator
- Plasminogen
Table 1. Target blood pressure
| Patient Population | Target BP |
| Diabetes | <130/85 mmHg Art. |
| Renal failure and proteinuria >1 g/day | <125/75 mmHg Art. |
| Essential | AH<140/90 mm Hg. Art. |
Return
Table 2. The largest studies in hypertensiology
| HOT | 1998 |
| SYST-EUR | 1997 |
| CAPPP | 1998 |
| UKPDS | 1998 |
| STOP-Hypertension-2 | 1999 |
| INSIGHT | 2000 |
Return
WHO/IAS Recommendations, 1999: main provisions
- Coordination of fundamental provisions with recommendations of PSC VI
- Moving away from the “staged” and “qualitative” approaches
- Stratification of patients by risk level
- Lower “target” blood pressure levels
- Replacement of the tactics of “stepped” prescription of drugs with “liberal” ones. Situations of preferential “class” choice of drugs have been established. Selecting a drug to initiate therapy from six main classes
- Emphasis on rational low-dose combination therapy
Blood pressure indicators
- Lack of age-related blood pressure norms
- Equivalence of SBP and DBP in the treatment of hypertension
- Shifting the focus from DBP to SBP
- Recognition of the leading role of SBP as a prognostic criterion for the development of complications
- Inverse relationship between DBP and the incidence of cardiovascular complications over 50 years of age
- Relationship between pulse pressure and the incidence of cardiovascular events
- Proven benefits and safety of significant reduction in high blood pressure
- Proven benefits and safety of treatment of hypertension and ISAH in elderly and senile age