TREATMENT FOR VASCULITIS IS AVAILABLE AT BRANCHES:
Treatment of vasculitis in the Primorsky region
Address: St. Petersburg , Primorsky district, st. Repisheva, 13
Treatment of vasculitis in the Petrograd region
Address: St. Petersburg , Petrogradsky district, st. Lenina, 5
The disease is usually accompanied by complications. Intestinal bleeding may occur from the gastrointestinal tract. Vasculitis can also cause liver damage. In the cardiovascular system, disorders such as cardiomyopathy and disruption of the heart valves can form. The most dangerous consequence of vasculitis is stroke. In the excretory system, a possible complication is glomerulonephritis.
Thromboangiitis obliterans
Diagnostic criteria (HJ Leu et al., 1985):
- Onset of the disease in men under 40 years of age
- Smoking
- Foot pain at rest
- Distal gangrene/ulcers of the upper and lower extremities
- Symptoms of intermittent claudication
- Migrating phlebitis
- Changes in the arteries of the upper extremities
- Distal type of arterial lesion
- Characteristic data from arteriography
- Histological examination data
- No signs of other diseases
Vasculitis - Causes and risk factors
Vascular inflammation is believed to be initiated by immune processes (associated with hypersensitivity reactions to antigens). For example, some diseases classified as systemic small vessel inflammation are associated with the presence of antineutrophil cytoplasmic antibodies. Allergic vasculitis is provoked by allergic reactions of the body. Cerebral vasculitis can occur as a complication of an infectious disease, tumor, or as a result of isolated damage to the blood vessels of the brain.
Vasculitis - types
1. Systemic vasculitis of small vessels (arterioles, capillaries and veins)
- Wegener's granulomatosis is a necrotizing vasculitis affecting the respiratory tract, eyes, kidneys and other organs.
- Microscopic polyangiitis - necrotizing vasculitis with damage to the lungs and kidneys, without the formation of granulomas
- Eosinophilic granulomatous vasculitis (Churg-Strauss syndrome)
- Hemorrhagic vasculitis associated with the deposition of IgA immunoglobulins (Henoch-Schönlein purpura) is characterized by damage to the skin, intestines and kidneys, accompanied by arthritis and arthralgia. This type of vasculitis most often occurs in children aged 4-7 years.
- Cutaneous leukocytoclastic vasculitis - isolated vasculitis without systemic involvement
2. Systemic vasculitis of medium vessels (visceral vessels, mesenteric, renal arteries, etc.)
- Polyarteritis of the arteries is a focal lesion of the arteries, which occurs with rupture of aneurysms and bleeding; infarction of organs and tissues is possible.
- Kawasaki disease is a vascular inflammation with mucocutaneous lymphatic syndrome that can affect the coronary arteries.
3. Systemic vasculitis of large vessels (aorta and large branches)
- Giant cell arteritis (Horton's disease) is a granulomatous arteritis, combined with polymyalgia rheumatica (pain in the shoulder and pelvic girdle), in patients over 50 years of age.
- Takayasu arteritis is a progressive inflammation of the aorta that often occurs in young women.
4. Mixed vasculitis (Behcet's syndrome)
In addition, vasculitis is divided into:
- Primary - the cause of the disease is unknown
- Secondary - changes in blood vessels are caused by other diseases (for example, rheumatoid arthritis, systemic lupus erythematosus) or are a side effect of medications
Etiology and pathogenesis of SV
The etiology of WS remains unknown. The possible role of viral or bacterial infection is actively discussed. However, there is not sufficiently convincing evidence of the etiological connection of SV with any viral or bacterial agent. The pathogenesis of WS appears to be complex, involving many mechanisms. Currently, the following leading factors are assumed to be involved in the development of SV:
- formation of pathogenic immune complexes (IC) and their deposition into the vascular wall and/or formation of IC in situ;
- formation of autoantibodies to ANCA (antineutrophil cytoplasmic antibodies) with activation and adhesion of neutrophils to endothelial cells, inducing damage to the latter;
- formation of autoantibodies to vascular wall antigens;
- immune responses mediated by T lymphocytes;
- direct impact of various infectious agents on the vascular wall;
- diverse local and systemic effects of released inflammatory mediators and cytokines;
- coagulation and vasospastic disorders;
- processes of interaction between endothelial cells and leukocytes with the release of a wide range of reformed and newly synthesized adhesive molecules.
There are primary and secondary vasculitis. Primary vasculitis is considered to be an independent disease. Vasculitis associated with other diseases, exposure to drugs or various toxic agents is considered secondary.
Symptoms of vasculitis
Manifestations of vasculitis depend on the characteristics of the course of the disease.
With periarteritis nodosa, muscle pain, sharp abdominal pain, vomiting, high fever, and weight loss may occur. Wegener's granulomatosis causes purulent and bloody nasal discharge, the nasal mucosa becomes covered with ulcers, and coughing up blood may occur. Giant cell arteritis is accompanied by weakness, fever, headaches, and weight loss. Ulcers on the genitals, stomatitis, and inflammation of the eyes (Behcet's syndrome) may occur.
With vasculitis affecting the skin, a rash occurs on the legs and other parts of the body. When the nervous system is damaged, sensitivity is impaired.
Treatment of the disease is complicated by diabetes mellitus, hypertension and venous insufficiency.
Secondary vasculitis or vasculopathy:
- For infections
- bacterial (infective endocarditis, sepsis)
- viral (chronic active hepatitis)
- rickettsial
- For parasitic diseases
- For drug (serum) sickness
- For malignant tumors (hairy cell leukemia, lymphomas, solid tumors)
- For DBST (diffuse connective tissue diseases) and RA
- For occupational diseases (berylliosis, silicosis, arsenic intoxication)
- Other reasons
To diagnose systemic vasculitis, an integrated approach is used with evaluation of research data:
- Clinics
- Laboratory methods (immunology)
- Biopsy results
- Instrumental methods
- Diagnosis criteria
Clinical signs suggestive of a diagnosis of vasculitis:
- Fever of unknown etiology or general (constitutional) symptoms that cannot be otherwise explained (weakness, weight loss, decreased performance)
- Symptoms of unexplained ischemia in various organs, especially in young patients or in the absence of risk factors for atherosclerosis
- Sudden or sequentially appearing visceral symptoms of vasculitis associated with damage to many organs, the clinical manifestations of which will be determined by the caliber of the affected vessel:
- Multiple mononeuritis
- Damage to the central nervous system - stroke, development of blindness
- Skin lesions (purpura, livedo reticularis, necrosis, nodules, fingertip infarctions)
- Non-destructive oligoarthritis
- Kidney damage
- Gastrointestinal lesions
- Changes in the lungs
- Changes in the cardiovascular system
Clinical manifestations of lesions of various sizes of vessels:
| Localization | Clinical manifestations |
| Damage to large and medium-sized vessels | |
| Common carotid arteries | Dizziness, headache, syncope |
| Maxillary arteries | Jaw pain when moving |
| Ocular arteries | Visual impairment |
| Subclavian arteries | Paresthesia or hyperesthesia of the hands, dysfunction of their hands, absence of pulse or pulse of different filling and height on a. radialis, different blood pressure levels in the arms |
| Renal arteries | hypertension, renal failure |
| Mesenteric arteries | Ischemic intestinal lesions (pain, perforation, bleeding) |
| Coronary arteries | Angina pectoris, myocardial infarction |
| Pulmonary arteries | Cough, bloody sputum, shortness of breath, pulmonary infarctions |
| Localization | Clinical manifestations |
| Damage to medium and small vessels | |
| Leather | Livedoreticularis, subcutaneous nodules, skin rash, ulcers, necrosis of fingertips and toes |
| Peripheral nerves | Multiple mononeuritis |
| Muscles | Myalgia, myositis |
| Joints | Arthritis, arthralgia |
| Kidneys | Necrotizing (crescentic) rapidly progressive glomerulonephritis |
| Gastrointestinal tract | Erosions, ulcers of the gastrointestinal tract, perforation, bleeding |
| Heart | Myocarditis, arrhythmias |
| Lungs | Pulmonary alveolar hemorrhages |
| Serous membranes | Pleurisy, pericarditis |
| Eyes | Retinal hemorrhages, scleritis |
Diagnosis is made difficult by the presence of common symptoms in various pathological conditions. Thus, pulmonary-renal syndromes can occur in the following conditions:
- Microscopic polyangiitis
- Churg-Strauss syndrome
- Granulomatosis with Wegener's polyangiitis
- Hemorrhagic vasculitis
- Goodpasture's syndrome
- SLE
- Rheumatoid vasculitis
- Systemic sclerosis
- Antiphospholipid syndrome
- Congestive heart failure
- Renal failure complicated by pneumonia (especially due to Legionella)
- Nephrotic syndrome with renal vein thrombosis and pulmonary embolism
- Liver cirrhosis with severe portal hypertension and ascites
It must be remembered that the most common interstitial lung diseases of known and unspecified etiology have the same clinical and radiological picture. These include:
- Pulmonary mycoses
- Disseminated pulmonary tuberculosis
- Parasitic lesions of the lungs
- Respiratory distress syndrome
- ILD in HIV infection
- Pneumoconiosis
- Exogenous allergic alveolitis
- Medicinal (MTX, D-PA, amiodarone, etc.)
- Radiation
- Post-transplant
Vasculitis - treatment
Treatment of systemic vasculitis (SPb) is primarily accompanied by immunosuppressive (suppressive) therapy, and medications are also used to improve blood flow in the vessels. In cases of severe disease, plasmapheresis is used (a method of purifying the blood of large particles such as immune complexes). Often, treatment of vasculitis requires consultation with a nephrologist, ophthalmologist, laryngologist, neurologist, dermatologist and surgeon.
In our clinic, you can be examined by a rheumatologist, receive qualified advice from doctors in other fields, and diagnose diseases using modern equipment.
Microscopic polyangiitis (MPA)
Diagnostic criteria for microscopic polyangiitis were proposed by the MHLW Vasculitis Study Group and finalized in 2006 in Japan. Main clinical manifestations 1.Rapidly progressive glomerulonephritis 2.Pulmonary hemorrhage or interstitial pneumonia 3.Visceral symptoms/signs other than renal/pulmonary manifestations 4.Purpura, subcutaneous hemorrhages, mononeuritis, etc.
Laboratory data 1. Positive MPO-ANCA 2. Positive CRP 3. Proteinuria, hematuria, increased levels of urea, creatinine 4. Changes on the radiograph: infiltration (alveolar bleeding), interstitial opacities.
Histological changes Necrosis of arterioles, capillaries and post-capillary venules, infiltration of inflammatory cells into the tissues surrounding the vessels.
Definite microscopic polyangiitis A) 2 or more clinical signs and positive histological results B) 2 or more clinical signs (including signs 1 and 2) positive MPO-ANCA
Possible microscopic polyangiitis A) 3 clinical signs B) 1 clinical sign and positive MPO-ANCA
Diseases for differential diagnosis
- Classic polyarteritis nodosa
- Granulomatosis with Wegener's polyangiitis
- Allergic granulomatous angiitis (Churg-Strauss syndrome)
- Goodpasture's syndrome
Typically, MPA has an acute onset and a more aggressive course than granulomatosis with polyangiitis (GPA) or SSS. MPA has many similarities with GPA, differing in the absence of granulomatous inflammation, as a result of which subglottic laryngitis, saddle nose deformity, and periorbital granulomas are not characteristic of MPA.
Cost of treatment for vasculitis:
| Services list | Price in rubles | |
| Saint Petersburg | Vsevolozhsk | |
| Initial appointment with a 1st stage rheumatologist | 1850 | — |
| Repeated appointment with a 1st stage rheumatologist | 1650 | — |
| Initial appointment with a rheumatologist, leading specialist | 2500 | 2000 |
| Repeated appointment with a rheumatologist, leading specialist | 2300 | 1800 |
| MANIPULATION | ||
| Capillaroscopy | 1500 | — |
Periarteritis nodosa, or periarteritis nodosa
Latin name periarteritis nodosa. This is a systemic necrotizing vasculitis of medium and small arteries affecting the skin, joints, peripheral nerves, intestines, heart and kidneys. The triggering of autoimmune disorders involves hepatitis B and C viruses, cytomegalovirus, parvovirus B1 9 and drugs (iodine preparations, sulfonamides, antibiotics). HBs antigen can be detected in 50% of cases.
The pathological process develops according to immune complex type III according to Jell and Coombs. Imprecise infiltration (neutrophils, then macrophages) and fibrinoid necrosis of the adventitia, tunica media and intima occur. Aneurysms form in the affected areas of the vessels. In the classic version of the disease, the vessels of the heart, kidneys and gastrointestinal tract are mainly affected. In the cutaneous benign form, skin vessels are more often affected. Glomerulonephritis is often detected, associated with hematuria and proteinuria.
Symptoms and complaints
The disease begins with fever and myalgia. Accompanied by malaise, weight loss and arthralgia, the development of infarctions of the intestines, kidneys, heart, and brain. Malignant arterial hypotension develops. Reticular changes in the skin pattern, elements of purpura and urticaria appear on the skin, up to the development of hemorrhages and necrosis. Involvement of peripheral nerves and blood vessels in the process is manifested by pain, paresthesia/paresis. When palpating areas with superficial arteries, nodules are revealed.
Laboratory diagnostics
Neutrophilia, thrombocytosis, elevated ESR and C-reactive protein are detected. Morphological study of biopsy samples of skin, muscles, and kidneys is possible. Markers of hepatitis B and C viruses are often detected.
Treatment
Corticosteroids are used, and less commonly, immunosuppressants (cyclophosphamide, in the absence of infection with hepatitis B and C viruses).
Papulonecrotic
The papulonecrotic type is characterized by the appearance of a small number of inflammatory nodules, within which, after some time, various necrotic changes are observed. As a result, a black crust forms, covering the bleeding ulcers. The healing process is accompanied by the formation of scars. Characteristic of papulonecrotic polymorphic dermal angiitis is localization on the extensor surface near the joints of the limbs. It should be remembered that this form of the disease is very similar to the papulonecrotic type of skin tuberculosis.
Takayasu arteritis
Also known as nonspecific aortoarteritis, or pulseless disease, is an obliterative vasculitis that affects the aorta and the vessels that arise from it.
Immune complexes are deposited in the walls of blood vessels. Inflammatory granulomas develop in the adventitia and outer layers of the middle lining of the vessels, including accumulations of lymphocytes, monocytes and, partially, neutrophils, giant cells, etc. Granulomas become fibrotic. Thrombosis occurs, sclerosis of the middle membrane, proliferation of the intima and, as a result, narrowing of the lumen of blood vessels.
Symptoms
Mostly young women suffer. The pathological process involves the thoracic aorta and its branches. The vessels of the neck and upper extremities are often affected. An aneurysm and thrombosis are formed. Vascular stenosis causes lameness, decreased or absent pulse, hypertension (frequent damage to the renal artery), and a discrepancy in blood pressure between the right and left arms. Fever, myalgia, arthralgia, headache and ophthalmological disorders may develop.
Laboratory diagnosis is not critical. There is an increase in ESR.
Treatment . Corticosteroids (prednisolone) are prescribed.
Causes
Until now, the causes of the development of this disease have not been studied enough. The causes of the manifestation of the primary form of the disease are determined only tentatively. It can develop due to viral and chronic infections, allergies , chronic autoimmune diseases, taking certain medications and contact with chemicals. The factors that provoke this disease are hypothermia, burns, radiation, trauma, and hereditary factors. However, these phenomena are not the causes of the disease, but its triggering factors.
Kawasaki disease
Kawasaki disease is a systemic arteritis of large, medium and small arteries, combined with mucocutaneous syndrome. More common in children than in adults. The arterial endothelium produces autoantibodies that bind to the Kawasaki antigen of endothelial cell membranes. Immune complexes are formed and immune inflammation develops.
Symptoms
Children aged 2-3 years are most often affected. The onset of the disease is acute - a 10-day high body temperature is accompanied by lymphadenopathy in the neck. Dry lips with redness and cracks, bilateral congestion of the conjunctiva, and conjunctivitis are noted. A red rash similar to hives appears on the skin, first on the palms and soles, then on the torso and limbs. Symptoms of systemic vasculitis and myocarditis appear after 2-4 weeks. Then, after 2 weeks, symptoms of fibrosis are added to the decreasing picture of vasculitis. Arthritis, arthralgia, uveitis, and photophobia develop. In subsequent years, aneurysms and blood clots form.
Behçet's disease
This is a chronic, relapsing systemic vasculitis, mainly affecting small and medium-sized arteries and veins, and is associated with HLA-B52. Autoantibodies to the epithelium of the mucous membranes appear, and immune complexes are formed. Lymphocytes infiltrate the walls of blood vessels and perivascular tissues. Swelling of the endothelium and narrowing of the lumen of blood vessels are noted.
Symptoms
Behçet's disease is accompanied by damage to the mucous membrane of the mouth (aphthae, stomatitis), the mucous membrane of the eyes (conjunctivitis), and the choroid of the eyes (uveitis). Recurrent ulcers of the external genitalia develop. Ulcers are sharply painful. The development of cutaneous vasculitis (erythema nodosum, papular rash, etc.) is possible.
Laboratory diagnostics
Autoantibodies to the epithelium of the oral mucosa and blood vessels are detected in the blood serum. The levels of certain classes of immunoglobulins, ESR and C-reactive protein levels increase.
Treatment
Colchicine, dapsone and non-steroidal anti-inflammatory drugs may be used.
Hemorrhagic vasculitis (Henoch-Schönlein purpura)
This is a hemorrhagic, necrotizing vasculitis of small and medium vessels, most often developing at the age of 2-10 years. The skin (mainly the lower extremities), gastrointestinal tract, joints and kidneys are affected.
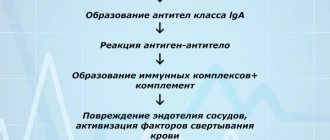
The disease develops according to the immune complex type: immune complexes consisting of antibodies, antigens and complement are deposited on the walls of blood vessels. Neutrophilic infiltrates are noted. As a result, intravascular coagulation develops with complement assets. Due to the increased permeability of the vessel wall, bleeding increases and hemorrhagic syndrome develops.
Symptoms
In sick children, a profuse symmetrical red papular-hemorrhagic rash with a diameter of 3-10 mm) appears on the skin of the extremities, buttocks and torso (palpable purpura), caused by hemorrhages from inflamed capillaries. Pain in large joints and abdomen, nausea, vomiting, fever, and gastrointestinal symptoms (pain, etc.) are noted. In some patients (from 10 to 60% of patients), the kidneys are affected - glomerulonephritis, etc. Proteinuria, micro- or macrohematuria may occur. Kidney lesions are similar to manifestations of IgA nephropathy.
Laboratory diagnostics
In biopsy specimens, granulocytic infiltration of the vessel walls is observed. Using immunocytochemistry, deposits of IgA, the C3 component of complement and fibrinosis are detected in post-capillary venules. The level of IgA and class A rheumatoid factor in the blood serum may increase. The ESR is increased.
Treatment
Non-steroidal anti-inflammatory drugs (ibuprofen, indomethacin) or paracetamol are used, and in more severe cases (abdominal syndrome) - prednisolone. For glomerulonephritis, it is possible to use an intravenous immunoglobulin drug.
Churg-Strauss syndrome
Also known as eosinophilic granulomatous vasculitis (angiitis), allergic angiitis and granulomatosis. This is a systemic vasculitis associated with allergic diathesis, most often affecting the lungs. Accompanied by asthma and eosinophilia. The pathology is close to periarteritis nodosa and Wegener's granulomatosis, but small vessels are more often affected, intra- and extravascular granulomas with a diameter of 1 mm develop, consisting of a central part with destroyed cells, altered collagen fibers and a peripheral part with macrophages, eosinophils and giant cells.
Symptoms
Asthmoid phenomena are noted - difficulty breathing and diffuse wheezing when inhaling. As the disease progresses, signs similar to those of periarteritis nodosa appear. Hemorrhages, papular-necrotic and ulcerative changes are detected on the skin. Arthralgia, abdominal pain, diarrhea, and hypertension develop. The main cause of death due to this pathology is heart disease due to cardiomyopathy.
Laboratory diagnostics
Eosinophilia, elevated IgE levels and, sometimes, rheumatoid factors are detected. When studying biopsy specimens, accumulations of eosinophils are observed in the extravascular space.
Treatment is symptomatic.
Necrotic-ulcerative
Another type of polymorphic dermal angiitis is the necrotic-ulcerative type, which forms a special type of blood clots in the affected vessels, causing necrosis of both individual areas of the skin and the entire skin with the further formation of a black scab. This type of disease is characterized by a severe course with a sudden onset and a sharp deterioration in the patient’s general condition, which can lead to death. Even if the patient does not die, hard-to-heal ulcers form on the affected areas of the skin, which are very difficult to treat.