To restore the hand after a stroke - this problem is solved by a set of rehabilitation measures carried out by specialists in the clinic and the patient at home in order to return the previous motor function as soon as possible. If after the “impact” the left upper limb fails, then a lot of time will pass before its partial or complete recovery.
When a cerebral hemorrhage occurs, no matter how mild or severe it is, some areas of the brain tissue are affected, leading to disruption of certain functions in the human body. The structure of the central nervous system is such that if your arm hurts after a stroke, it means that the area near the right hemisphere was damaged, because it contains the centers that control motor activity.
Consequences of a stroke
Basic Concepts
Movement is carried out by skeletal muscles, which consist of fibers that have the properties of excitability and contractility. Excitation (like contraction) occurs under the influence of nerve impulses from the central nervous system. The participation of muscles in movement can be different, depending on the place of attachment to the bones of the skeleton, on the structure of the joints, muscles can produce different movements.
The approach of one part of the body to another (for example, the forearm to the shoulder, the palmar surface of the hand to the forearm, the fingers to the palm, the shin to the thigh, the plantar surface of the foot to the shin) is called flexion. Therefore, the muscles that produce this movement are called flexors. It should be noted that quite often muscles are named not by their main functional properties, but by their place of attachment or location. Sometimes the names of muscles reflect their shape or composition.
For example, the main flexor of the forearm is the biceps brachii muscle. The muscles that flex the hand and fingers are called flexors, respectively, of the hand and fingers. Flexion of the lower leg is carried out by three muscles at once: the biceps femoris, semitendinosus and semimembranosus muscles, which make up the posterior group of femoral muscles. Plantar flexion of the foot is performed by the triceps surae muscle.
The opposite movement to flexion is extension (for example, arms at the elbow, legs at the knee). The muscles that perform this movement are called extensors. The hand and fingers are extended by the extensors of the hand and fingers, respectively.
The main extensor of the forearm is the triceps brachii muscle. The leg at the knee is extended by the powerful quadriceps femoris muscle, and the dorsiflexion of the foot is done by the tibialis anterior and peroneus longus muscles (named after the shin bones along which they are located).
In addition to flexion and extension, there are other types of movements. So, when a part of the body moves away or approaches in relation to its midline, they speak of abduction or adduction. For example, abduction of the arm to the side, adduction of the arm to the body, abduction (dilation) and adduction of the hips. The muscles involved in these movements are abductors or adductors, respectively. So, the pectoralis major and latissimus dorsi muscles bring the arm to the body, and the deltoid muscle abducts it. Adduction of the hip is carried out mainly by the adductor longus muscle, and abduction by the gluteus minimus muscle.
This phenomenon should also be taken into account. As mentioned, the flexion of the forearm towards the shoulder is carried out mainly by the biceps brachii muscle. But the brachioradialis muscle is also involved in flexing the forearm. When bending the forearm to the shoulder, these muscles act as synergists (producing the same movement). The same muscles that produce oppositely directed movements (for example, one is flexion and the other is extension) are called antagonists. And the triceps brachii muscle, which extends the forearm (from the shoulder), is an antagonist of the biceps muscle. Working as antagonists, muscles can in many cases act as synergists in another movement.
Muscles perform two types of work: dynamic (moving the body in space or parts of the body relative to each other) and static (providing a certain position of the body in opposition to external forces seeking to change this position). At the same time, long-term, tireless muscle tension, called tone, provides resistance to gravity and maintains a certain body position in space (for example, standing or sitting).
Meanwhile, movement is not reduced to a simple contraction of individual muscle fibers or even muscle groups. From the moment of birth, their improvement and development occurs: from the chaotic movements of a newborn to the highly differentiated movements of an adult. In parallel and in conjunction with this, the structures and functions of the cerebral cortex as a whole are being improved.
It is important that the muscles not only perform movements, but also have unique sensory functions. The presence of a particularly sensitive apparatus in the muscular system allows the central nervous system to constantly monitor the correctness and accuracy of movements, and, on the other hand, regulate the state of muscle tone.
The performance of any movement is accompanied by a flow of impulses entering the cerebral cortex not only from sensitive muscle receptors, but also from other receptors, signaling the need to change the movement if it does not produce the desired results. However, information from sensory muscle receptors plays a major role in the regulation, coordination and control of movements.
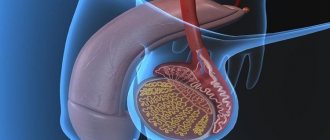
With a stroke, damage most often occurs to the overlying spinal cord (supraspinal) segment of the motor pathway, which leads to the development of central paralysis or paresis. Impaired movement of the limbs is observed, as a rule, on one side of the body (hemiparesis or hemiplegia). A characteristic sign of central paralysis, in addition to the absence or limitation of movement, is increased muscle tone (spasticity) and increased tendon reflexes.
The tone is not increased in all muscles, but only in certain ones (usually the so-called anti-gravity muscles). These are the postnotonic muscles, which ensure the vertical position of the body, the pectoralis major, the biceps brachii, the flexors of the hand and fingers, the long adductor femoris, the quadriceps femoris and the triceps surae muscle. The tone of the antagonists of these muscles (deltoid, triceps brachii, extensors of the hand and fingers, posterior femoral group, tibialis anterior and peroneus longus) is usually not increased, but paresis is much more pronounced.
One of the main goals of rehabilitation treatment of patients with movement disorders due to central paresis is to reduce the excessive flow of nerve impulses from spastic muscles and to increase sensory signals from their antagonists.
For this purpose, from the very first days after a stroke and during the entire time the patient is in bed, it is recommended to use a special positioning of paretic limbs, which is called “positional treatment.”
Psychological support
The patient’s relatives need to provide a positive environment at home, demonstrate their willingness to help, support the patient, and assure that his condition is temporary and changes for the better are inevitable. If the patient’s condition allows, he should be involved in feasible household chores, making him feel important and not removed from everyday worries.
A psychologist or psychotherapist will help you cope with panic attacks and depression. If the patient experiences acute conditions, aggression, or suicidal thoughts, the help of a psychiatrist and the prescription of medications may be required.
The duration of the recovery period depends on many factors: the extent of the damage, the age of the patient, and the presence of concomitant diseases. In patients who have suffered a mild form of stroke, partial recovery requires 1-2 months, and complete recovery takes about 3 months. In severe forms with persistent impairments, partial restoration of lost functions occurs after at least six months, and the chance of returning all lost skills is minimal.
According to statistics, after the first year after a stroke, 60% of patients do not need outside help. 30% can return to their previous work. Help with complex tasks is required during this period by 20% of patients. 15% of those who have suffered a stroke remain dependent on outside help, 5% need constant care.
Treatment by positioning on the back and on the healthy side
The paretic limbs are positioned with the patient in a supine position so that the muscles in which tone usually increases after a stroke (shoulder adductors, arm flexors, hip adductors, leg extensors and dorsal flexors of the foot) are stretched. To do this, place a chair with a pillow at the patient’s bedside, on the side of the paralyzed limbs, on which the sore hand is placed, palm up.
The arm is straightened at the elbow and moved to the side at an angle of 90 degrees. A cotton swab covered with oilcloth is placed under the patient's armpit. The fingers are extended. The hand and forearm are bandaged to a splint, which can be cut out of some hard material (for example, plywood) and covered with gauze.
To fix the position of the hand, place a bag of sand or salt (weighing 0.5 kg) on it. The paralyzed leg is bent 15-20 degrees at the knee, under which a bolster is placed. The foot rests against a wooden box (“boot”) covered with soft material. It is recommended to put a small pillow in the boot to better support the foot.
The patient can remain in the supine position for 1.5 to 2 hours. Then it should be turned onto its healthy side.
When laying the patient on his healthy side, as opposed to laying him on his back, the paralyzed limbs are given a flexion position. The sore arm is bent at the shoulder and elbow joints and a pillow is placed under it, and the paralyzed leg is bent at the knee and hip joints and also placed on a pillow. Just as in the supine position, it is very important to ensure the correct position of the hand and foot. The fingers of the hand should be straightened, the hand should be tied to the splint and lie on the pillow, palm down. The foot should rest against the box. The patient can remain in a lying position on the healthy side for 30 to 50 minutes.
During the first days after the disease, they regularly alternate between placing the paretic limbs in the position of the patient on the back and the healthy side. Treatment by position is not performed during meals, sleep at night, or other therapeutic measures.
Styling paretic limbs prevents the development of muscle contractures, helps reduce muscle tone and prevents the development of pain in the joints (especially in the shoulder). In addition, changing the patient's position in bed every 1-2 hours prevents the development of bedsores.
Walking with a cane
Buy a good, comfortable cane that fits your height with a comfortable handle.
Rehabilitation after a stroke physical therapy includes training in walking patterns. First, the stick is rearranged, after which a step is taken with the injured leg. And only then does the healthy one walk. Make sure there are always two points of support.
The affected leg usually turns outward. To correct this, ask the patient to place emphasis on the knee, bending it slightly. Healthy people do this without even thinking. When rehabilitating after a stroke at home, exercises involve learning this process almost from scratch.
Passive movements and massage
Simultaneously with positional treatment, they begin to engage in passive gymnastics (movements in the joints of paretic limbs, which are carried out by a physical therapy methodologist or a person replacing him). Passive movements are carried out without active muscular assistance from the patient. They are performed carefully, at a slow pace.
Passive movements are carried out as fully as possible, isolated in each joint. To do this, the person working with the patient clasps the paretic limb above the joint being worked on with one hand, and with the other below this joint. And the development is carried out in the following sequence: shoulder, elbow, wrist joints and fingers, hip, knee, ankle joints and toes. The volume and tempo of movements gradually increase, their number for each joint can be from 5 to 10. Passive movements in the first days after a stroke are recommended to be carried out 2-3 times a day for all joints of the limbs.
When performing movements, the initial position of individual parts of the limbs is of great importance.
For example, during passive movements in the shoulder joint, the patient is placed on his healthy side, and the affected arm is bent at the elbow. With one hand they fix the shoulder joint of the sore arm, with the other they clasp the arm bent at the elbow joint and make circular movements, pressing towards the shoulder joint, as if screwing the head of the humerus into the glenoid cavity. Abduction of the hip is more complete when the leg is bent (at the hip and knee joints), since this reduces muscle tension in the adductor muscles of the thigh, and the resistance of these muscles decreases.
On these same days, you should begin to do a light massage of both healthy and paretic limbs. If you can use a variety of massage techniques when massaging healthy limbs, then when massaging paretic limbs you need to be very careful. The fact is that excessive massage can lead to a sharp increase in the tone of certain muscle groups, which is undesirable. Therefore, when massaging paralyzed limbs, it is recommended to use the following rules.
Massage on the arm should begin from the shoulder, and on the leg - from the buttocks and thigh (the patient's position is lying on his back or on his healthy side). Then they move on to massage other parts of the limbs.
When massaging muscles in which the tone is usually increased (pectoralis major muscle, biceps brachii, flexors of the hand and fingers, quadriceps femoris, triceps surae), only light stroking should be used. In this case, the pace of massage movements should be slow. When massaging their antagonists, in which the tone is usually also increased (extensors of the forearm, hand and fingers, posterior femoral group, tibialis anterior and peroneus longus muscles), you can still use other massage techniques: rubbing and shallow kneading. These muscles can be massaged comparatively more energetically and at a faster pace.
Exercises while sitting
After a stroke, rehabilitation at home, exercises should be performed in different positions to vary the load. It is important to include the muscles of the sore side in the work. Their relaxation will lead to delayed rehabilitation and even injury. It is better if they are insured by a healthy person rather than by pillows and other devices.
When the patient is already sitting upright, specifically rock him. This way the body will get used to the load. We gradually complicate the task. Such gymnastics after a stroke will help a person move on to more complex exercises as soon as possible.
Active gymnastics
Passive movements and massage are preparatory measures before active gymnastics, which plays an important role in developing isolated movements in paretic limbs.
Active gymnastics begins with exercises for healthy limbs, alternating them with gymnastics for paretic ones, as well as breathing exercises. The load on the cardiovascular and respiratory systems should increase gradually, otherwise the patient may become overfatigued. It is recommended to monitor the pulse after each exercise performed 1-5 times. Exercises should be separated by rest breaks lasting 1-2 minutes.
Active gymnastics begins with exercises in isometric mode. Isometric muscle contraction is a contraction without shortening, that is, without movement in the joints. When performing exercises in this mode, it is often necessary to provide assistance to the patient.
To achieve isometric contraction of the extensors of the hand and fingers, the patient is placed on his back, the arm is bent at the elbow and the forearm is placed in a vertical position. Then you should extend (straighten) the hand and fingers (so that they are 180 degrees with the forearm). Holding the paretic arm by the forearm, the patient is asked to keep the hand and fingers in this extended position. In the same starting position, but holding the paretic arm by the hand, the patient is asked to hold the forearm in a given vertical position.
This exercise is aimed at training the forearm flexors in an isometric manner. To train the forearm extensors, the patient’s paretic arm is extended at the elbow and raised vertically upward. When fixing the patient's shoulder, they are asked to hold the arm in a raised position. To do this, he must tense the extensors of the forearm.
Isometric contraction of the abductor muscles of the shoulder is carried out with the patient positioned on the healthy side. The paretic arm is raised up and bent at the elbow at an angle of 90 degrees. While supporting the forearm, ask the patient to hold his hand in this position.
The hip flexors are trained isometrically with the patient in the supine position. The paretic leg is bent at the knee, lightly holding it by the shin. And the patient is asked to hold the leg in this position, not allowing it to straighten at the knee. In the same starting position, you can train the hip abductors. Slightly moving the leg bent at the knee to the side, ask the patient to hold it in a fixed position.
These exercises make up the initial complex of active gymnastics. In the first days of classes, they should be performed 2-3 times, gradually increasing the number of exercises to 5-10 times.
When patients begin to develop independent isolated movements, they begin to train them. For this purpose, light exercises are used, the purpose of which is to eliminate the unwanted influence of gravity. “It is best to carry them out using various suspensions, hammocks and blocks.
Lightweight exercises should not cause pain. They are performed at a slow pace, in a volume accessible to the patient. First of all, exercises are carried out for muscles whose tone usually does not increase. So, for example, supporting a paretic arm with a hammock, the patient is asked to perform those active movements that he has already developed.
This includes abduction and adduction of the shoulder, flexion and extension of the forearm, and extension of the hand. Facilitated abduction and adduction of the hip is trained with the patient in the supine position. And by turning the patient onto the healthy side and supporting the affected leg, they train the extension and flexion of the lower leg.
As the range of active movements increases over time, you should add exercises with light, measured resistance. It works like this; for example, when actively extending the lower leg, you should try to slightly impede this movement by pressing on top of the lower leg and not allowing the leg to extend at the knee. Exercises with light resistance are carried out similarly for the remaining muscle groups.
It must be remembered that resistance exercises are included in the complex of active gymnastics only when active isolated movements appear in a sufficiently large volume.
These exercises are recommended mainly for muscles in which the tone does not increase. The person performing them needs to pay special attention to breathing. The patient should not delay him. Resistance exercises should be combined with passive relaxation exercises.
How to teach sitting, standing, walking
Already in the first days after a stroke, if the general condition is satisfactory, it is recommended to teach the patient to sit and stand. It is necessary to prepare in advance a scarf for fixing the arm, a rubber traction for the leg, and also choose comfortable shoes with low wide heels that fix the ankle joint (for example, weightlifting shoes, light men's shoes).
They begin to put the patient in bed as soon as his well-being and the state of the cardiovascular system allow. These periods can range from 3-5 days to 2-3 weeks from the onset of the disease and are determined by the attending physician.
Initially, the patient is in a reclining position for 3-5 minutes. For this purpose, a pillow is placed under his head and back. Gradually, in this way, over 2-3 days, the patient is transferred to a semi-vertical position, but sitting with legs down is allowed only approximately on the 4-5th day of classes. In this case, a pillow is placed under the patient’s back, the paretic arm is fixed with a scarf, and a bench is placed under the legs. The time of sitting in bed with legs down should be gradually increased from 10-15 minutes to 1-2 hours or more, depending on the patient’s well-being.
As soon as the patient begins to sit in bed with his legs down, exercises to strengthen the leg muscles are included in the complex of therapeutic gymnastics: using a rocking roller, an elbow expander or a rubber “frog” to fill air mattresses with air, adapted for training the lower leg muscles and developing movements in the ankle joint
At the same time, they begin to use exercises for the sore hand with various objects (for which some children's toys can be used). It is recommended to assemble and disassemble pyramids, children's construction sets, and various figures from cubes.
An important stage is learning to stand and walk. The patient is brought to him gradually. First, preparatory exercises are performed - passive and active imitation of walking in a lying position.
A passive imitation of walking consists in the fact that the practitioner, clasping the ankles of both legs of the patient with his hands, alternately bends and extends them at the knees, without lifting the feet from the sheet. Active imitation of walking is performed by the patient himself, if he retains the mobility of his paretic leg. If it is not there, then the practitioner helps the patient “walk.” The latter straightens and bends the healthy leg independently.
In agreement with the attending physician, the patient is then taught to stand. The first time he is asked to stand up, holding the bedside frame or headboard with his good hand. The practitioner must help the patient from the side of the paretic limbs. The patient should be supported by the waist, while simultaneously fixing the knee joint of the paretic leg in an extended state.
The patient should stand straight, evenly distributing body weight on the sick and healthy sides. At the very beginning of training, the patient can remain in a standing position for no more than a minute. Gradually, the time of standing on your feet is increased to 5-7 minutes. After the patient can confidently, holding the headboard of the bed, stand independently on both legs, they move on to teaching him how to alternately transfer the weight of the body to the healthy and sore leg.
To do this, the patient is asked to place his feet shoulder-width apart and slightly sway from side to side. In this case, you can use a rubber “frog”, on which the patient presses with the paretic leg: if the load on the sore leg is large enough, a characteristic sound of air escaping will appear. The patient must be supported while performing this exercise.
When the patient has mastered this exercise, it is necessary to teach him to stand on one leg, first on the healthy one. In this case, the paretic leg is in a bent position (with the help of the practitioner). When learning to stand on a sore leg, the student must first fix the knee joint of the paretic leg in an extended state at a right angle. It is better if another person is present to support the patient.
When performing this exercise, it is necessary that the patient has reliable support: a high headboard, a bedside frame, a bracket driven into the wall. There should be a chair behind him for safety or rest.
Teaching a patient to stand is an important and responsible stage in treatment. Do not rush to move on to the next exercises until the patient learns to feel confident on his feet independently, without your help. If you rush, the next stage may be unnecessarily delayed.
Learning to move should begin with the “walking in place” exercise. Then the patient must learn to walk forward, backward, sideways along the bed or table. He must do all this while holding onto the bedside frame or table. In the future, they begin to teach the patient to move without the help of these supports, but with support.
During recovery, at first the patient uses a three- or four-legged crutch when moving, then a stick. When learning to walk, you should pay attention to the position of the foot, check the patient’s stability, make sure that he bends his leg sufficiently at the hip and knee joint, does not lift it to the side, does not touch the floor with his toe, and places his foot correctly.
During training, it is better to fix the sore arm with a scarf to prevent stretching of the shoulder joint bursa, and to eliminate foot sagging, use devices that fix it: a rubber rod (connecting a sock or shoe with a garter located above the knee) or boots with a high rigid fastening.
To consolidate the skill of correct foot placement, it is advisable to walk along a path on which traces of training steps are marked. Another method is used for the same purpose - overcoming obstacles 5-15 cm high (for example, planks that are placed in front of footprints on the same path). You should constantly adjust the position of the foot when resting the entire sole on the floor, as well as when moving the leg.
When the patient begins to move independently around the room, the goal of physical therapy will be to strengthen the leg muscles necessary to restore correct gait.
At the next stage, the patient is taught to walk up the stairs, and one must be especially careful to protect the patient from falling. Since the patient expends significant effort during these exercises, it is necessary to pause from time to time to rest in a sitting position and to perform breathing exercises.
Simultaneously with exercises to restore leg function, exercises for the arm are performed. These are the already mentioned exercises with small objects - cubes, pyramids, plasticine, the use of a rocking table, a spring microexpander in the patient's position sitting at the table, and without objects. Here is one of them: the patient is seated with the affected side of the body on the table, and his outstretched paretic arm is placed on the table. The practitioner takes the patient’s hand, fixing his shoulder near the elbow. Then, shaking lightly, slowly bends the arm at the elbow and straightens it.
Another exercise is recommended. Starting position: sit facing the table, place your feet shoulder-width apart, place the sore arm bent at the elbow at a right angle, palm down (forearm along the table) with fingers straight and spread apart. The practitioner presses the patient’s hand to the table with one hand, and with the other raises the patient’s elbow up, shaking it lightly.
The following exercise helps reduce tone in the flexors of the forearm, hand and fingers. The patient is seated on a chair so that the hand of the affected hand is placed under the sore thigh. The practitioner, holding the shoulder with one hand, clasps the patient’s elbow with the other and straightens his arm at the elbow, shaking it lightly.
Various hanging movements and swinging of the limbs are also used to relax muscles. For example, the patient is seated with the affected side of the body against the back of a chair and the hand of a healthy hand is placed in the axillary area. As a result, the sore arm ends up suspended and is slowly swung, gradually increasing the amplitude. The same exercise can be performed on the couch: the patient lies on his back, with his sore arm hanging down.
To reduce muscle tone in the muscles of the hand, it is recommended to rub its back surface in the direction from the fingertips to the wrist.
The following exercise is also useful. The practitioner clasps the patient’s thumb with one hand, and with the other all the others (four fingers folded together) and performs their maximum extension, while simultaneously abducting and extending the patient’s thumb. The hand should be held in this position for 1-3 minutes until muscle relaxation is observed.
Sometimes the patient experiences involuntary concomitant movements, that is, when the leg is bent at the knee, the arm at the hand and elbow simultaneously bends. The same can be observed when coughing and sneezing. A number of exercises help eliminate friendly movements.
The following can also be recommended. Sit facing the table with your feet shoulder-width apart. Place your hands on the table and press the healthy sore hand. Slowly bend and straighten your leg at the knee (if this is difficult to do, then you should help the sore leg with the help of the healthy one), while simultaneously holding your arm in an extended position. You can also sit on a chair and stretch your arms forward (paretic below, healthy above), put them on a cane, which is located on the side of the sore leg.
It is necessary to keep your arms extended the next time you move your legs. Place the sore leg on the knee of the healthy one, return to the starting position, place the healthy leg on the knee of the sore one, return to the starting position. In addition to exercises for paretic limbs, the complex of therapeutic exercises must include exercises for healthy limbs. Actually, every therapeutic gymnastics procedure from the first days of classes should begin with exercises for healthy limbs.
It should also be borne in mind that throughout the entire recovery period, in addition to active gymnastics (light resistance training, relaxation exercises, and breaking concomitant movements), passive movements continue to be used for the joints of paretic limbs.
Patients will be able to perform some of them independently. For example, for the shoulder joint - lock your arms, raise them up (the healthy arm works, the sick one is passive), then tilt them left and right. Take the gymnastic stick with both hands, lift it up (the healthy arm works, the sick one is passive), lower the stick behind the head. Passive movements for the wrist joint can also be carried out by the patient himself, helping himself with his healthy hand - doing extension, flexion, circular rotation in one direction and the other. Passive movements for a paretic foot can be performed with a healthy hand, placing the bent sore leg on the knee of the healthy one.
When performing both active and passive movements, it is necessary to achieve the greatest possible range of movements. These exercises should be performed rhythmically, at a calm pace. As noted above, all active movements should be alternated with relaxation exercises.