The article was checked by a neurologist, chiropractor V.V. Oganov. , is for general informational purposes only and does not replace specialist advice. For recommendations on diagnosis and treatment, consultation with a doctor is necessary.
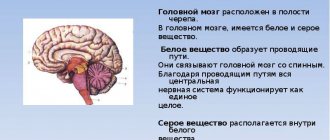
Dyscirculatory encephalopathy is a heterogeneous condition that depends on many causes; literally translated, it means “impaired functioning” of the brain. We are talking about a common chronic form of cerebrovascular pathology, which is characterized by multifocal or diffuse brain damage and leads to disruption of its functions, which is manifested by a combination of neurological and psychological disorders.
Discirculatory encephalopathy - what is it?
Dyscirculatory encephalopathy (DEP) is a common disease that affects many patients with arterial hypertension. Due to impaired blood supply to the brain, changes begin to occur in the tissues, which ultimately lead to disruption of brain functions.
Unfortunately, the manifestations of DEP in the early stages (headache, tinnitus, nausea) are such that patients may not consult a doctor about them, considering them to be the result of fatigue or stress. As DEP develops, decreased visual and hearing acuity, impaired coordination, and autonomic disorders may appear. With severe brain damage and significant microcirculation disorders, patients may experience mental disorders. In the Department of Neurology of the Yauza Clinical Hospital, doctors conduct a comprehensive diagnosis of DEP and prescribe comprehensive treatment that takes into account the causes of the development of the disease in a particular patient.
Classification
Taking into account the cause of development, the disease can be atherosclerotic, venous, hypertensive and mixed. Depending on the characteristics of the course, classic, galloping (rapidly progressing) and remitting varieties of the disease are distinguished. To clarify the severity of the process, a general three-stage classification is used, where:
- Stage 1 (initial). There are minor disorders of the emotional sphere and cognitive activity, there is no neurological deficit.
- Stage 2 (moderate). Cognitive-emotional dysfunction worsens and is accompanied by motor symptoms.
- Stage 3 (decompensation). The ability to work and the ability to self-care are lost, and dementia develops.
Causes of development of dyscirculatory encephalopathy and stages
Gradually increasing circulatory failure leads to the appearance of small-focal multiple necrosis of brain tissue. Discirculatory encephalopathy is the result of this process.
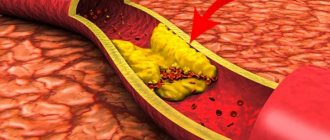
The basis of the disease is atherosclerotic damage to the intracerebral arteries, hypertensive stenosis, which provokes disruption of blood flow in the blood vessel basin. Long-standing encephalopathy often precedes stroke. The likelihood of the disease increases with the patient's age.
This concept is not used abroad. Stages of chronic cerebral ischemia that have gone far in their development are designated by the term “vascular dementia.” The problem is of social significance, since neurological and mental disorders in this pathology can lead to severe disability in patients.
DEP can develop with atherosclerosis, hypertension, and disorders of the venous outflow of the brain. The heterogeneity of discirculatory encephalopathy is reflected in the etiology, clinical, morphological and neuroimaging characteristics of its individual forms.
Having high blood pressure automatically puts a person at risk. With its systematic increase to 160/90, the likelihood of developing encephalopathy increases several times.
Accordingly, there are several types of DEP:
- atherosclerotic (mainly the main vessels of the head are affected)
- hypertensive;
- mixed;
- venous;
- developed as a result of other reasons (vegetative-vascular dystonia, rheumatism, vascular diseases, etc.).
The most common causes of the development of DEP are atherosclerosis, arterial hypertension, and their combination. Smoking, alcohol abuse, and various stressful situations also contribute to the onset of the disease.
Osteochondrosis can indirectly contribute to the development of dyscirculatory encephalopathy - in this disease, due to deformation of the intervertebral discs, the vertebral arteries that supply the brain with blood can be compressed.
Degrees of DEP
Stage classification is used to assess the patient's condition. The course of the disease is divided into three stages:
Stage I (mild)
The main complaints are headache, dizziness, noise in the head, fatigue, decreased attention, instability when walking, sleep disturbance. Doctors also note slight impairments in memory, attention, and cognitive activity. In this case, patients can lead a normal life, receiving the necessary therapy.
Stage II (moderate)
The main complaints are disturbances of consciousness, memory loss, slowing of mental processes, impaired attention, thinking, ability to plan and control one’s actions, walking disorders, apathy. Such patients already have difficulty socializing, and their performance decreases.
Stage III (severe)
The main manifestations are similar to those of stage 2 disease, but they are more pronounced. Serious cognitive impairments are combined with behavioral disorders (aggression, disinhibition, etc.). Gradually, patients lose the ability to care for themselves.
Reasons for development
The main etiofactor is insufficient blood supply caused by pathological changes in blood vessels. In 60% of cases, DEP is provoked by cerebral atherosclerosis. The second place in prevalence is occupied by increased blood pressure due to hypertension and secondary hypertension due to kidney damage, Itsenko-Cushing's disease, and pheochromocytoma.
Other causes include vertebral artery syndrome, cerebral vascular anomalies, cervical osteochondrosis, spinal injuries, arrhythmias, vasculitis, arterial hypotension and TBI. Diabetes mellitus, complicated by diabetic macroangiopathy, is often cited as the main or complicating factor.
Previously, encephalopathy of discirculatory (vascular) origin was traditionally considered as a disease of the elderly. Now the situation has changed. Heart diseases have become “younger”, which has led to an increase in the frequency of early manifestations of DEP. Experts point out that currently the pathology is often detected in people under 40 years of age.
When systemic metabolic disorders are added, they speak of discirculatory dismetabolic encephalopathy of complex (mixed) origin. This option is more typical for representatives of older age groups.
Symptoms and initial manifestations
Clinical symptoms have certain characteristics depending on the type of dyscirculatory encephalopathy. The development of vestibular-atactic, pseudobulbar, cephalic, and psychopathological syndromes is characteristic.
On examination, mild incoordination and symptoms of anisoreflexia are revealed, indicating a small focal brain lesion. This stage, in addition to diffuse, unexpressed neurological symptoms, is characterized by the presence of a syndrome reminiscent of the asthenic form of neurasthenia.
The main symptoms of the initial stage of DEP progression include:
- insomnia;
- unstable attention;
- increased fatigue;
- irritability;
- memory impairment;
- slight change in gait (instability, shortening of stride);
- decreased productivity of intellectual work.
Patients at stage I of dyscirculatory encephalopathy of the brain often complain of headaches and noise in the head, they are tearful, and their mood is often depressed. To diagnose the disease, complaints must appear at least once a week for three months, that is, last for a long time.
Discirculatory encephalopathy: the danger of pathology and treatment methods
This pathology is a brain lesion that occurs due to constant progressive circulatory disorders of the central nervous system of various etiologies. It affects motor, emotional and cognitive function, and depending on the severity of the symptomatic picture is divided into three stages. To make and confirm the diagnosis, ultrasound, echo-EG, EEG, REG, duplex scanning of cerebral vessels, ophthalmoscopy, MRI are required. Therapy is selected individually and consists of neuroprotective, antiplatelet, antihypertensive, vascular and other drugs.
Clinical picture at stage II-III
Memory deterioration progresses, neurological symptoms worsen. Pathological changes are formed, leading to maladjustment of the sick person.
Characteristic symptoms of grade 2 dyscirculatory encephalopathy of the brain are:
- reducing the range of interests;
- fixation on some problem (viscosity of thinking);
- daytime sleepiness and poor sleep at night;
- impaired coordination of movements (staggering when walking, slow movements);
- significant reduction in efficiency.
Clinically significant depression, fear, anxiety, phobias, intolerance to stuffy rooms and physical activity can be noted.
With the third degree of progression, intellectual-mnestic, psychoorganic and coordination disorders intensify. Symptoms of dyscirculatory encephalopathy become even more pronounced. At this stage, repeated strokes, hypertensive crises, and transient changes in cerebral circulation are not uncommon.
Leading manifestations:
- weakening criticism towards oneself;
- pronounced deterioration in balance;
- epileptic seizures;
- limiting daily activity;
- severe parkinsonism;
- dementia;
- urinary incontinence.
Patients gradually lose their professional fitness, ability to self-care and need outside care.
Prevention
Dealing with stage 2 DEP is difficult, but possible. The prognosis of the syndrome is quite favorable in case of timely diagnosis and initiation of treatment. If the patient carefully monitors his condition and follows the doctor's recommendations, this will provide him with several years or even decades of a good standard of living. It is important to visit a neurologist regularly so that he can assess the patient’s condition and, if necessary, make timely adjustments to the treatment plan.
Assignment of disability
Many patients at the second stage of dyscirculatory encephalopathy can be given disability group 2 or 3.
The disability group depends on the severity of symptoms:
- Group 3 is issued to patients diagnosed with stage 2 DEP who have a list of symptoms that interfere with their ability to work. The patient at this stage is able to care for himself independently and rarely needs outside help in everyday life.
- Group 2 includes patients diagnosed with stage 2 or 3 DEP. The patient’s life activity is limited due to the severity of the symptoms as a result of a micro-stroke suffered as a result of the disease.
What aggravates the course and stimulates the progression of dyscirculatory encephalopathy?
The condition worsens when exposed to the following factors:
- Chronic and/or acute psycho-emotional stress (frequent stress at work or in the family, insufficient time to sleep, working without rest or at night).
- Hypokinesia (lack of dosed exercise and walks in the air).
- Obesity or overweight.
- Alcohol abuse and smoking.
- Diabetes mellitus, which causes inflammation of the inner walls of blood vessels.
- Dysfunction of the thyroid gland, causing disruption of metabolic processes in the body.
- Diseases of the cervical spine that impair blood flow in the vertebrobasilar region.
Predisposing factors that worsen the condition also include blood diseases (increased platelet levels or hematocrit), heart disease (rhythm disturbances) and vasculitis (vascular inflammation). Also to this list should be added congenital hypoplasia (narrowed diameter) of the cerebral arteries.
Features of DEP In the clinical hospital on Yauza
To clarify the etiology and pathogenesis of DEP, specialists from the Department of Neurology of the Yauza Clinical Hospital conduct the following examinations:
- general and biochemical blood tests with determination of platelet count, glucose, cholesterol, bilirubin, fibrinogen, urea, creatinine, electrolytes, triglycerides and lipoproteins, homocysteine;
- MRI of the brain (including with intravenous contrast);
- MSCT of brain and neck vessels with contrast;
- MR angiography of intracranial arteries and vessels of the neck;
- triplex scanning of the extracranial (neck) and intracranial (head) sections;
- electrocardiography, echocardiography, Holter monitoring of ECG and blood pressure;
- consultations with an ophthalmologist, cardiologist, endocrinologist.
Methods for diagnosing DEP
It is very important to make a diagnosis as early as possible in order to promptly begin vascular therapy to compensate for neurological disorders. Therefore, all patients at risk for discirculatory encephalopathy must be regularly examined by a neurologist. The risk group includes:
- People suffering from atherosclerosis;
- Diabetics;
- Hypertensive patients;
- Aged people.
To identify cognitive impairment, special tests are required. Tasks may include the need to remember and repeat a list of words named by the doctor, draw a dial with a given time, or repeat certain words.
In addition, consultation with an ophthalmologist and ophthalmoscopy, determination of visual fields, will be required. The following hardware diagnostic methods are shown:
- Echo-EG;
- EEG;
- REG;
- ECG and daily ECG monitoring;
- Doppler ultrasound of head and neck vessels;
- MRA of cerebral vessels;
- Duplex scanning;
- MRI of the brain.
MRI of the brain will help distinguish DEP from other pathologies: Alzheimer's disease, Creutzfeldt-Jakob disease, disseminated encephalomyelitis. Magnetic resonance imaging makes it possible to visualize foci of silent infarctions, while areas of leukoaraiosis and cerebral atrophy also occur in other neurodegenerative pathologies.
To detect etiological factors, consultation with a cardiologist and nephrologist, blood pressure monitoring, a coagulogram, determination of lipoproteins and cholesterol in the blood, and a blood sugar test are required.
Treatment of DEP in the clinical hospital on Yauza
Comprehensive diagnostics allows specialists to prescribe adequate drug treatment. It should be aimed primarily at normalizing blood supply to the brain and blood pressure, correcting symptoms and preventing further damage to blood vessels and brain tissue. It is also important to use drugs that normalize the metabolism of brain cells and increase vascular tone.
In addition, neurologists at the Yauza Clinical Hospital offer each patient an individual complex of non-drug therapy, which includes reducing alcohol consumption, quitting smoking, and regular dynamic physical activity. It is also important to follow nutritional recommendations: limiting the consumption of table salt, saturated fats, sufficient consumption of potassium, magnesium and calcium salts, eating foods that improve the functioning of the circulatory system.
You can see prices for services in the price list or check by calling the phone number listed on the website.
Impact on key risk factors
Due to the high importance of recurrent strokes for the progression of motor and cognitive disorders in patients with DEP, a higher priority is the prevention of vascular complications. Correction of existing symptoms is secondary. In such patients, “aggressive” prophylaxis is necessary.
Antihypertensive therapy
Maintaining normal blood pressure levels can help prevent or slow the progression of DEP. Most often, in the presence of chronic cerebral circulatory failure, doctors recommend the use of drugs belonging to the groups of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers. These medications are believed to have protective properties against the brain, blood vessels, heart and kidneys.
If these drugs are not enough to control blood pressure, they are combined with other drugs - diuretics, beta blockers, calcium channel blockers. Only a doctor can prescribe medications suitable for patients with DEP.
Correction of carbohydrate metabolism
There are no doubts about the cause-and-effect relationship between dysfunction of carbohydrate metabolism and the development of circulatory disorders in the brain. To correct the pathological process, an appropriate diet and medications that lower blood sugar levels are prescribed.
Lipid-lowering therapy - statins
Since the other main cause of DEP is cerebral atherosclerosis, patients with this disease are often prescribed drugs that lower blood cholesterol levels. The most commonly used drugs are statins, which in addition to lowering cholesterol levels also improve the condition of the inner layer of blood vessels (endothelium), reduce blood viscosity, stop or slow down the progression of atherosclerosis and have an antioxidant effect.
Antithrombotic therapy
One of the mandatory components of the treatment plan for patients with DEP. Antiplatelet agents affect platelets, preventing them from sticking together (aggregation), which improves cerebral circulation. Low-dose aspirin is most often prescribed.
Reduced homocysteine levels
Elevated levels of homocysteine (a sulfur-containing amino acid) are a risk factor for the development of vascular disease and dementia. To correct indicators, folic acid and B vitamins (B12, B2 and B6) are prescribed.
Healthy lifestyle and exercises for memory development
Bad habits, lack of physical activity and poor nutrition have an impact on the deterioration of cognitive functions over the years. This confirms the benefits of a healthy lifestyle in preventing the development of mixed and vascular dementia.
Thanks to the conducted research, it was possible to confirm the relevance of the concept of “cognitive reserve”. According to this concept, a healthy lifestyle significantly reduces the likelihood of developing dementia. Receiving higher education does not have any effect on the prognosis of the disease.
Dementia drugs
To reduce the severity of clinical symptoms in dementia, drugs are prescribed whose action is aimed at improving the transmission of signals between neurons through synapses. Active substances prevent neuron death: glutamate NMDA receptor antagonists and acetylcholinesterase inhibitors.
Antidementia drugs reduce the severity of behavioral (aggression, agitation) and cognitive (problems of attention, speech and memory) disorders. Medicines do not improve the general condition of the patient, but significantly slow down the rate of deterioration of symptoms.
Nootropic and vasoactive drugs
The use of vascular drugs to combat vascular lesions is unjustified. The effectiveness of the use of Ginkgo Biloba, ergot alkaloids and methylxanthines is controversial.
Physiotherapy
Complex therapy, which combines drug and non-drug methods of combating the disease, is more effective. Among the effective physiotherapeutic methods for treating DEP, the following should be highlighted:
- Exercise therapy (a set of exercises is prescribed individually by a doctor);
- transcranial magnetic stimulation;
- acupuncture;
- massage of the collar area;
- vortex fields;
- electromyostimulation.
Surgery
The need for surgery arises if the pathological process develops against the background of rapid progression of narrowing of the lumen. Surgery is also necessary if serious complications develop.
The following types of operations are widespread:
- Stenting. It involves inserting a special dilator into the vessel to improve blood flow in the part of the artery that has been narrowed.
- Carotid endarterectomy. It is carried out for atherosclerosis in order to cleanse the internal walls of the carotid artery.
Surgical intervention does not completely eliminate the disease, but it makes it possible to improve the patient’s condition and slow down the progression of the disease.
Spa treatment
With progressive organic changes in brain tissue that occur as a result of chronic vascular insufficiency, sanatorium treatment is recommended. This approach to therapy is possible only in the absence of pronounced changes in the psyche and deterioration of cerebral circulation. Such patients are sent to balneotherapeutic and climatic resorts with hydrogen sulfide and radon waters.
Treatment
According to clinical recommendations, therapy should be comprehensive, aimed at reducing the manifestations of vascular disease, improving cerebral circulation and microcirculatory processes, protecting cerebral structures from ischemia and hypoxia. The doctor explains what kind of disease this is and why it is important to undergo regular therapy.
How to treat is determined individually. Depending on the nature of the underlying pathology, anti-sclerotic, hypoglycemic and antihypertensive drugs are prescribed, and cholesterol levels are corrected using diet or special medications.
To improve hemodynamics, drugs from the groups of phosphodiesterase inhibitors, calcium channel blockers, and alpha-2 adenoceptor antagonists are used. Antiplatelet agents are used to normalize blood clotting. The brain's resistance to a lack of blood supply is increased with the help of neuroprotectors: GABA and pyrrilidone derivatives, membrane-stabilizing drugs, vitamins and cofactors. In some cases, surgical treatment is recommended: reconstruction of the arterial trunks, carotid endarterectomy, creation of an extra-intracranial anastomosis.
Recommendations for the prevention of DEP include timely treatment of vascular pathologies, blood pressure control, and giving up bad habits. How long you can live and what your quality of life will be depends on the time you start treatment and compliance with medical recommendations.
Call our operator at tel. 8(969)060-93-93 and make an appointment at a convenient time.
Preventive measures
To prevent dyscirculatory encephalopathy, a healthy lifestyle and a balanced diet mean a lot. Increased physical activity also provides good preventive results. It is necessary to control the level of blood pressure, the content of cholesterol and its fractions in the blood.
Diseases of the cerebral vessels are considered the most common pathology in the practice of a neurologist. Dyscirculatory encephalopathy is one of the leading causes of cognitive impairment, dementia, and disability in old age. A comprehensive assessment of the patient's condition, the impact on the underlying cause of the disease and symptoms helps to improve the quality of life and prevent serious complications.
FAQ
Which doctor should I contact?
Discirculatory encephalopathy is a neurological disorder. If alarming symptoms occur, you should contact a neurologist. The doctor will order an examination and make an accurate diagnosis, based on the results of which he will prescribe adequate treatment. The sooner treatment measures are taken, the more optimistic the prognosis for the patient will be.
How long can you live with dyscirculatory encephalopathy?
Life expectancy depends on genetics, concomitant diseases, the severity of atherosclerosis or hypertension. Therefore, it is completely different for different patients.
Early symptoms
DEP begins unnoticeably and develops quite slowly. First of all, problems in the emotional sphere are noted. About 65% of patients suffer from depression, which, unlike depressive neurosis, occurs against the background of minor traumatic situations, while patients are not inclined to note depression and low mood. They are fixed on various somatic disorders, like patients with hypochondriacal neurosis. Complaints may include:
- Arthralgia;
- Back pain;
- Neuralgia;
- Noise in the head;
- Tinnitus;
- Pain of various localizations.
Their distinctive feature is that they do not fit into the clinical picture of supposed somatic pathologies. Depression in DEP is difficult to respond to psychocorrection and treatment with antidepressants.
The initial stage of DEP often manifests itself in increased emotional lability, which includes:
- Sudden mood swings;
- Cases of uncontrollable crying for minor reasons;
- Irritability;
- Attacks of aggressive behavior towards others.
In addition, sleep disturbances, fatigue, headaches, and absent-mindedness are noted. The symptomatic picture is similar to neurasthenia, but with dyscirculatory encephalopathy the symptoms are combined with cognitive impairment.
Moreover, in 90% of patients, cognitive impairment occurs at the initial stage of the disease. These include:
- Decreased concentration;
- Memory impairment;
- Reduced speed of thinking;
- Difficulties in planning activities;
- Fatigue with mental effort;
- Problems with speech reproduction of information while maintaining memory.
Movement disturbances, such as dizziness and unsteadiness when walking, may also occur. DEP must be differentiated from vestibular ataxia, since nausea and vomiting may be present, but only during walking.