Deep vein thrombosis, along with thrombophlebitis of the saphenous veins and thromboembolism of the pulmonary arteries, are combined into a single concept - venous thromboembolic complications (VTEC).
Venous thrombosis is an acute disease characterized by the formation of a blood clot in the lumen of a vein with a more or less pronounced inflammatory process and disruption of blood flow. The presence of an inflammatory component in the area of thrombosis determines another name for this disease - thrombophlebitis.
Most phlebologists, understanding the conventions of such a division of venous thrombosis, use the term “thrombophlebitis” to denote damage to the saphenous veins (in which symptoms of inflammation are pronounced), and the terms “thrombosis”, “deep vein thrombosis”, “phlebothrombosis” to denote damage to the deep veins .
Deep vein thrombosis (DVT) is a disease that negatively affects not only the venous and lymphatic return system, but also worsens the function of the cardiovascular system as a whole.
If you do not take active steps to eliminate this pathology, the further course of the pathological process becomes persistent, prone to self-development and irreversible.
The disease does not have strictly characteristic symptoms and has many risk factors and triggering factors, which requires the additional use of additional high-precision modern instrumental diagnostic tools to clarify its presence and type of course, the main of which in modern clinical conditions is the method of ultrasound angioscanning with color mapping.
- According to the International Consensus Statement, the incidence of deep vein thrombosis in the general population is approximately 160 cases per 100,000 population, with the incidence of fatal pulmonary embolism being 60 per 100,000 population.
- In Russia, venous thrombosis affects 240,000 people annually, and pulmonary embolism, including fatal ones, develops in 100,000 of them, which significantly exceeds the incidence rates of tuberculosis, viral hepatitis, and HIV infection.
- In the United States, approximately 200,000 people are hospitalized each year for deep vein thrombosis. In this case, 1/3 is accounted for by repeated thromboses. Among Italian residents of the most active working age (from 20 to 55 years), deep vein thrombosis is diagnosed within 1%.
- Venous thrombosis occurs in a wide variety of clinical situations and complicates the course of many diseases. The incidence of postoperative thrombosis, according to various authors, is 20-59%.
Possible reasons
The reasons for the formation of blood clots and emboli in the arteries can be divided into several groups:
· pathological changes in the walls of the arteries (endarteritis, atherosclerosis, vasculitis);
· changes in blood flow that occur with aneurysms, vascular stenosis, as well as their damage (bending, compression, etc.);
· diseases that negatively affect blood clotting.
The source of arterial thromboembolism often becomes the heart in the presence of pathologies associated with cardiac arrhythmias, left ventricular aneurysm, endocarditis, etc.
Also, the formation of blood clots may be preceded by a surgical operation to replace the valve apparatus with an artificial prosthesis.
Another common source of the disease are vessels with atherosclerotic plaques.
In the development of arterial thrombosis and embolism, special attention should be paid to the functional neurovascular factor. The human central nervous system is directly involved in the regulation of blood circulation in certain areas, which is why nervous shocks and disorders often cause disturbances in coronary and cerebral circulation.
Thrombophilia
If the patient has suffered a stroke, myocardial infarction, pulmonary embolism or thrombosis of the veins of the lower extremities, then it is highly likely that thrombophilia can be assumed - a predisposition to the formation of blood clots, that is, blood clots localized in the vessels or cavity of the heart. Thrombophilia does not always lead to thrombosis, but it significantly increases the risk of its occurrence. This is not a disease, but a pathological condition leading to illness.
Manifestations of thrombophilia are associated with the formation of blood clots in the veins and/or arteries, which disrupt the functioning of internal organs and pose a serious danger to the health and life of the patient. Thrombosis is essentially a normal, physiological process that prevents excessive blood flow at sites of vessel damage. However, when the thrombotic process is excessive, then it becomes pathological. Despite the fact that thrombotic conditions are much more common in older people, the presence of thrombophilia can occur in childhood, starting from the neonatal period.
Types of thrombophilia:
- hereditary (genetically determined)
- acquired (as a result of surgery, serious injuries, long-term use of medications - for example, oral contraceptives).
The pathogenesis of thrombosis is almost always complex. Episodes of thrombosis occur due to the combined effects of hereditary and acquired factors.
Hereditary factors include :
- Deficiency of Antithrombin-III – the main plasma protein factor that has an inhibitory effect on the process of blood clotting.
- Deficiency of protein C - the main physiological anticoagulant, an activated clotting factor.
- Deficiency of protein S – a cofactor of protein C, which enhances its effect.
- The Leiden mutation is a change in some areas in the gene encoding the activity of coagulation factor V.
- Prothrombin gene mutation G2021OA
- Hyperhomocysteinemia is a complex pathology characterized by increased levels of homocysteine in the blood.
- Dysfibrinogenemia
The main provoking prothrombotic factors are:
- installed vascular catheter;
- infectious diseases;
- vascular malformation or damage;
- chemotherapy;
- heart disease;
- heart valve replacement;
- systemic lupus erythematosus;
- rheumatoid arthritis;
- Crohn's disease;
- ulcerative colitis;
- primary antiphospholipid syndrome;
- polycythemia;
- sickle cell anemia and other hemoglobinopathies;
- kidney disease;
- diabetes;
- inflammation.
Important:
- The most common hereditary thrombophilias include carriage of the Leiden mutation, prothrombin mutations, deficiency of protein C, protein S or antithrombin.
- The most significant acquired thrombophilias are antiphospholipid syndrome, myeloproliferative diseases, and paroxysmal nocturnal hemoglobinuria.
Thrombophilia during pregnancy
Often, genetically determined thrombophilia first manifests itself during pregnancy. This is due to the emergence of the third circle of blood circulation - the placental, which has its own specific characteristics and puts an additional burden on the body. That is why pregnancy and thrombophilia is a dangerous combination that requires increased attention from women and doctors. This condition is corrected with medications and allows you to carry and give birth to a child.
In such cases, it is necessary to control the level of RFMC, D-dimer, fibrinogen, antithrombin III, protein C, protein S, as well as determine genetic polymorphisms of folate cycle genes (MTHFR (1298A>C), MTHFR (677C>T), MTR, MTRR, SLC19A1 (RFC-1)), as well as thrombophilia genes (F2, F5, F7, F13, PAI-1, FGB, ITGA2, ITGB3, SERPINE1). A comprehensive diagnosis of antiphospholipid syndrome is necessary: identification of lupus anticoagulant and determination of antibodies to cardiolipin and beta-2-glycoprotein-1.
To diagnose thrombophilia use:
- analysis of the clinical picture and risk factors, medical history of the patient’s coagulation system and family history;
- instrumental diagnostic methods (ultrasound Dopplerography, CT and MRI, angiography);
- laboratory research methods.
Who is at risk?
- People over 60 years old
- People whose relatives had thrombophilia
- Pregnant
- Women taking oral contraceptives
- Patients with cancer, autoimmune, metabolic diseases
- Recent severe infections, injuries, surgeries
Laboratory tests for diagnosing thrombophilia:
1. Level I. Base Rating:
- General blood analysis
- Fibrinogen (increased)
- APTT (reduced)
- Thrombin time (reduced)
- Factor V Leiden mutation G1691A
- Prothrombin factor IIG2021OA mutation
- Antithrombin III deficiency
- Activated protein C resistance
- Protein C deficiency
- Protein S deficiency
- Homocysteine (increased)
- Methylenetetrahydrofolate reductase, MTHFRT677T
- Antiphospholipid antibodies IgG (increased)
- Lupus anticoagulant (detection)
- Genetic research. Detection of abnormalities in the genes of blood clotting factors V and prothrombin.
Deficiency of AT-III, proteins C and S, or positive results of all these tests are characterized as high-risk thrombophilia, and carriage of factor V Leiden or factor II prothrombin mutations is characterized as low-risk thrombophilia.
2. Level II . I studies and recurrent thrombosis, a family history of thrombosis, or severe thrombosis:
- Dysfibrinogenemia
- Plasminogen activator inhibitor I (PAI-1)
- Tissue factor pathway inhibitor (TFP1)
3. Level III . Proposed markers of thrombophilia:
- Factors VIII, IX, XI, XII
- von Willebrand factor
- Platelet receptor polymorphism
- Spontaneous platelet aggregation
Treatment of thrombophilia
There is no specific treatment for thrombophilia. The treatment tactics for thrombophilia are selected individually, but the goals it pursues are always aimed at solving the following problems:
- Elimination of blood clots
- Treatment of the underlying pathological condition
Conservative techniques that are used in the process provide an integrated approach and include the following:
- A diet that excludes the consumption of fatty and fried foods, as well as foods high in cholesterol
- Taking pharmacological agents: disaggregants, anticoagulants and vasodilators
The issue of the need to use preventive therapy aimed at preventing the formation of blood clots is decided individually for each patient. If the risk of thrombosis is high, prophylactic treatment can prevent a number of serious complications.
The prognosis of thrombophilia depends on its type, the presence and severity of previous cases of thrombosis, as well as comorbidity.
Other news All news
27.12.2021
Very soon we will open new branches in Kyiv and Nikolaev!
24.12.2021
Dila's work schedule on holidays
22.12.2021
Vaccinated? Find out the exact amount of antibodies against coronavirus at a special price!
0 0
Symptoms of the disease
With arterial thrombosis or embolism, an acute cessation of blood circulation occurs in those tissues for which the affected vessel is responsible for the blood supply. In this case, you may feel severe pain in one or another organ (limb, abdomen, etc.). Gradually, in the absence of medical care, the tissues in the affected area die and gangrene develops.
If there are no alternative routes for bypass blood flow, as, for example, with damage to the femoral artery, the disease will be severe. The disturbances will not be so severe if there are other vessels capable of supplying blood to the affected organ.
Thromboembolism in most cases is characterized by a sudden onset . If we are talking about damage to the arteries of the lower extremities , you will feel acute pain and gradually increasing numbness. As sensitivity is lost, the limb becomes immobile. Embolism of large arteries is accompanied by a state of shock with cold sweat, nausea and vomiting. The skin on the affected area first turns pale, but then the pallor gives way to patchy cyanosis. The pulse of the peripheral arteries located below the affected area is not determined. With long-lasting spasm and lack of blood circulation, gangrene .
With thromboembolism of the abdominal aorta, the clinical picture is determined by the completeness and speed of its blockage. The first sign of pathology is a sharp and very severe pain in the abdomen, radiating to the lower extremities. The skin turns pale, the patient falls into a state of shock. The pulse in the vessels of the lower extremities cannot be felt, and rapidly developing gangrene can lead to death within a few days. If the disease develops gradually, the symptoms do not appear so clearly and do not develop so rapidly.
Blockage of the mesenteric artery is accompanied by an infarction of the affected area of the intestine, which manifests itself with signs characteristic of an acute surgical abdomen: acute pain, increased body temperature, shock, vomiting.
Diagnosis of arterial thrombosis and arterial embolism
In our department of vascular surgery, the diagnosis of arterial thrombosis and arterial embolism is performed in accordance with the highest medical standards. Diagnostic measures include:
· collection of anamnesis and analysis of patient complaints;
· visual inspection;
· a number of laboratory tests;
· performing ultrasound examination of blood vessels;
angiography;
· computed tomography using a contrast agent.
Based on the results of the studies, the degree of the disease is determined: first degree (A, B), second degree (A, B) or third degree (A, B). After making an accurate diagnosis, our specialists decide on further treatment tactics.
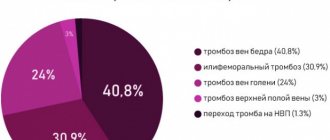
Diagnosis of deep venous thrombosis
Diagnosis of thrombosis is extremely difficult. This is primarily due to the absence of clinical symptoms. According to some data, out of 1000 venous thromboses, only 100 have any clinical manifestations. Of these, 60 patients will develop PE, but only 10 will have clinical signs. It should be recognized that today there is not a single clinical symptom, laboratory or instrumental sign that would indicate with absolute certainty the presence of PE and DVT. Clinical manifestations of thrombosis and ultrasound results can be the basis for the correct diagnosis of venous thrombosis. The clinical picture of deep vein thrombosis consists of a complex of symptoms that characterize a sudden disturbance of venous outflow with preserved arterial blood flow to the limb. Swelling, cyanosis of the limb, bursting pain, local increase in skin temperature, overflow of the saphenous veins, pain along the vascular bundle are characteristic to one degree or another for thrombosis of any localization. Movements in the joints of the limb and sensitivity remain virtually unchanged. General signs, such as low-grade fever, weakness, adynamia, and slight leukocytosis, occur in most patients. The diagnosis of thrombosis largely depends on the location of the lesion, i.e. on the level of distribution of thrombotic masses.
Treatment methods
Arterial thrombosis and embolism require hospital treatment , which is selected depending on the severity of the pathology.
Conservative therapy with the use of anticoagulants, angioprotectors, intra-arterial drug block and other drugs is prescribed for the first degree of the disease. Non-surgical treatment may be possible for the second degree A, but more often doctors still advise resorting to surgical removal of blood clots.
In our department, highly qualified specialists perform surgical removal of blood clots (direct and indirect thrombectomy) and perform shunt operations. If a patient experiences muscle contraction due to swelling under the fascia, a fasciotomy is indicated in addition to vascular surgery.
If we are talking about arterial thrombosis of the limb of the third degree, then it will no longer be possible to avoid the formation of a gangrenous focus. In some cases, surgery on the affected vessels can be performed to improve blood flow, which makes it possible to avoid amputation. In case of third degree B, high limb amputation is prescribed.
Treatment of deep vein thrombosis
Treatment of venous thromboembolism can be conservative or surgical. If deep vein thrombosis is suspected, if conditions permit, the patient should be admitted to a specialized angiosurgical hospital. Before instrumental examination, one must proceed from the assumption that the patient has a floating thrombus. In this regard, the patient must be transported to the hospital in a lying position and bed rest is required before the examination. Patients with thrombosis without the threat of thromboembolism can be activated using elastic compression of the limb to improve venous outflow, activate muscle collaterals, and prevent varicose transformation of the saphenous veins. The appointment of long-term elastic compression of the extremities is an immutable rule of conservative treatment of thrombosis of both deep and superficial veins (subcutaneous thrombophlebitis).
Aspirex Straub technology . A unique Swiss method for removing blood clots from deep veins. Today, our clinic is the only one where indications for this method have been developed. A special probe is passed through the blood clot and completely sucks it out. During the procedure, a special trap is installed in the inferior vena cava to prevent thromboembolism. Performing this procedure for deep vein thrombosis leads to complete elimination of the blood clot and prevents the development of complications of thrombophlebitis and post-thrombotic disease.
Thrombolytic drugs and anticoagulants are used for conservative treatment. Surgical methods include embolectomy or fragmentation and removal of the thrombus using a probe.
The most realistic prevention of threatening pulmonary embolism is the effective treatment of acute venous thrombosis. Treatment of acute venous thrombosis includes the immediate administration of heparins with parallel administration of antivitamins K. With progressive growth of the thrombus and the threat of embolization, the possibility of installing a removable vena cava filter should be considered, followed by surgical removal of the thrombus.
It is very important to timely and adequately assess the risk of thrombosis in each individual case. The consequences of lack of thrombosis prevention lead to death from pulmonary embolism, an increased risk of repeated episodes of venous thromboembolism, and the development of post-thrombotic disease. Currently, there are all possibilities for carrying out effective preventive measures to prevent thromboembolism. Prevention and treatment of deep vein thrombosis should be considered as prevention of pulmonary embolism.
Prevention measures
Thromboembolism prevention is based on timely detection and treatment of heart and vascular diseases, so we recommend undergoing a comprehensive examination at least once a year.
It is also necessary to lead a healthy and active lifestyle, exercising moderately and adhering to the principles of a healthy diet. The diet should be dominated by foods of plant origin, but it is advisable to exclude foods containing cholesterol.
In the summer, you should avoid dehydration by following a drinking regime. Bad habits, such as smoking, increase the risk of blood clots - give them up.