Reasons for the development of pathology. Symptoms Possible complications of lymphangioma Diagnosis of pathology and treatment methods
Lymphangioma
or lymphatic malformation - the scientific definition of pathology, is a benign tumor formed in the plexus of lymphatic vessels of connective tissue.
At present, the true causes of the tumor have not been established. There is an opinion among doctors that lymphangioma
is a real benign tumor that develops in the body due to the existing conditions. On the other hand, there is an opinion that the pathology is a congenital malformation of the lymphatic system. The neoplasm consists of cysts of various sizes. The most common manifestation of tumor development are nodes with a diameter of 0.2-0.3 cm. However, in medical practice there are cases of the presence of large formations as a result of malformation of the lymphatic system, which are detected upon visual examination. A benign tumor most often develops in childhood. In some cases, the pathology is a congenital form of the disease.
According to the Ministry of Health, lymphangioma
occurs quite often. Every tenth case from the general picture of the development of tumors in children is associated with a benign neoplasm in the lymphatic system. There is a clear division into primary tumors and secondary neoplasms. The secondary form of tumor growth is observed as a result of infectious diseases suffered by the child and complications arising in connection with this.
Reasons for the development of pathology. Symptoms
It was said earlier that at present there is no clear idea about the reasons for the development of benign neoplasms of the lymphatic system. As a result of examination of patients, it was found that lymphangioma
most often becomes the result of the development of a congenital malformation of the lymphatic system. In some cases, the pathology forms during the prenatal period and begins to develop intensively immediately after the birth of the child. Often, a benign tumor of the lymphatic system develops against the background of other abnormalities of the body. The congenital nature of the pathology, in accordance with the latest scientific developments and guesses of medical scientists, can be influenced by a poor environmental situation for the expectant mother, including exposure to gamma radiation. Other indirect factors influencing the formation of pathology may be poor heredity and complications resulting from severe systemic and infectious diseases suffered by the expectant mother.
The symptoms of the pathology are pronounced. With the development of a tumor at an early age, the child experiences the appearance of compactions in the neck, in the oral cavity, and somewhat less often in the internal organs and in the peritoneum. There are cases of nodules developing in other parts of the patient’s body. The tumor is localized in the subcutaneous fatty tissue. Depending on the symptoms, the following types of pathology are distinguished:
- capillary lymphangioma
; - cavernous lymphangioma
; - cystic lymphangioma
.
Capillary or simple pathologies include neoplasms, the location of which most often is the oral cavity, tongue, and the inner surface of the child’s cheeks. From a clinical point of view, the neoplasms in this case look like swellings measuring 203 cm, soft to the touch and with an unchanged color. There is no pain when palpating the tumors. A detailed analysis can reveal the structure of the seals, consisting of a network of capillaries, a large number of lymphoid cells and connective tissue.
The second type of pathology, cavernous lymphangioma
manifests itself in the form of bubbles on the surface of the skin, the size of which is 2-5 cm. Bubbles, as a rule, appear in the soft subcutaneous tissues in the areas of the largest plexus of the lymphatic system, neck, chest area, on the side of the body, on the arms and legs.
The third type of pathology, cystic lymphangiomas, is much more common in medical practice. Neoplasms develop at the site of the plexus of lymph nodes. Large, spherical formations can occur in the submandibular region, armpits, or in the area of the ears. Unlike the previous two types of pathology, cystic lymphangioma
is characterized by rapid growth, which is caused by the rapid filling of the cyst cavities with fluid. As a result of cyst rupture, abscesses and infection of the body often occur.
A distinctive feature of the first two types of the disease is the ability to stop tumor growth on its own. Regression in tumor development, ending with scarring, is often observed. Detected lymphangioma
in childhood it develops rather slowly, the process of which accelerates during puberty. The reasons explaining such dynamics are not fully understood. There is an opinion among doctors that the activation of tumor growth with the onset of puberty is associated with the impact of the developing secretory system of the body on the state of the lymphatic system.
Limited lymphangioma in a cancer patient
Limited (capillary) lymphangioma (lymphangioma circumscriptum) is a congenital or acquired anomaly of the superficial lymphatic vessels, representing grouped papules, on the top of which there are vesicles that contain clear lymphatic fluid, but can become hemorrhagic, resembling “frog spawn” in appearance [1] .
Wegener in 1877 first divided lymphangiomas into simple, cavernous and cystic [2]. Capillary lymphangioma belongs to the category of simple ones; the term “cutaneous lymphangioma circumscriptum” (CLC) was proposed by M. Morris in 1889 [3]. Almost a century later, Peachey and Lever in 1970 described the classical and localized forms of dermatosis based on histopathological features and clinical presentation [4].
CLC accounts for 4.0% of all skin tumors and up to 25.0% of all benign vascular neoplasms in children. The onset of the disease is usually observed in childhood, with up to 90.0% of cases occurring before 2 years of age [5]. However, the manifestation of CLC has also been described in adults. A retrospective study conducted at the Aga Khan University Hospital (Aga Khan University, Karachi, Pakistan) showed that from 2002 to 2012, the average age of patients with CLC was 27 years [6]. Gender differences have not been described, but girls are more often affected among young children [7]. The incidence in the United States is 1.2–2.8 per 1000 births [8]. Data on morbidity in Russia are not found in the literature. The role of heredity has not been established [9].
Pathogenetically, CLC is a typical hamartoma. The pathogenesis of dermatosis was described by Whimster in 1976. The author noted that during ontogenesis, abnormal lymphatic cisterns grow separately from normally functioning ones in the thickness of the hypodermis and are associated only with the superficial lymphatic bed. Contractions of smooth muscles discharge lymph from the cisterns into the superficial lymphatic vessels, which, due to high pressure, expand and protrude into the epidermis [10]. It is noteworthy that the visible clinical skin process does not correspond to the number of abnormal cisterns, creating an “iceberg” effect [11]. It is important to note that the absence of cutaneous lymphedema indicates the presence of lymphatic drainage through normally functioning vessels [5].
Histologically, accumulations of cystic lymphatic spaces are determined, occupying the entire thickness of the dermis. Acanthosis and papillomatosis, morphological differences in superficial and deep lymphatic vessels are characteristic. Thus, endothelial cells of the upper channel have a high electron density, are flattened (up to 0.1–0.3 μm), their nuclei contain densely packed chromatin, and the basement membrane has a different number of layers in different areas. In turn, endotheliocytes of the deep channel are less flat (up to 0.6–2.5 μm), the basement membrane is continuous throughout, pinocytotic vacuoles are defined, formed by invagination of the cell membrane. Comparison of morphology suggests that the vessels of the superficial lymphatic bed have undergone pathological changes as a result of loss of transport function, while the vessels of the deep bed are morphologically unchanged [12].
Cutaneous manifestations of CLC are represented by grouped translucent vesicles with serous-hemorrhagic contents, resembling “frog spawn” [13]. However, along with vesicles, bullous elements can be observed. Trauma to the elements leads to bleeding and lymphorrhea. Sometimes the rash may undergo changes such as hyperkeratosis or verrucous growths. Thus, LC Horn in 2005 described a case of giant CLC in a 22-year-old woman, externally resembling a giant Buschke-Levenstein condyloma [14, 15]. Most often, the rashes are localized on the proximal parts of the limbs, trunk, axillary region, as well as on the oral mucosa, especially on the tongue. Rashes on the penis, vulva, and scrotum have also been described [16, 17]. The dermoscopic picture is represented by hypopyon-like lacunae from light brown to purple, surrounded by light septa. Some authors compare such finds to “bunches of grapes.” Hypopyon-like lacunae reflect sedimentation of blood in tissue fluid [18].
The classic form of CLC primarily affects the upper extremities, upper back, axilla, and chest. This form is not characterized by verrucous and hyperkeratotic transformation; its dimensions exceed 1 cm2, and manifestation is typical at an early age. The localized form, in turn, is usually less than 1 cm2, occurs at any age and on any part of the body. Two forms have been described in one patient in the form of an overlap syndrome [4]. There are possible associations of CLC with Cobb, Proteus, and Maffucci syndromes [19–21]. D. V. Elkini et al. describe secondary lymphangiomas developing in the area of postmastectomy lymphedema resulting from surgical and/or radiation intervention, which was observed in our case [22].
Differential diagnosis is carried out with molluscum contagiosum, hemangioma, angiokeratoma. In addition, it is important to exclude cutaneous metastases of malignant neoplasms (carcinoma teleangiectoides), the visual manifestations of which are almost identical to CLC. However, in the case of neoplasia, the main morphological elements are nodules - often painless, round or oval, dense, mobile, elastic to the touch, from physiological color to brown, black-blue and even red, located, as a rule, next to the primary tumor [23 ].
The goals of treatment for CLC are pain relief, drainage of dilated lymphatic and blood vessels, and treatment of secondary infection if it occurs [24]. It is important to explain to the patient that existing methods of treating CLC do not exclude the development of relapse of dermatosis. Surgical treatment is the most effective, the effectiveness of which, according to the literature, reaches 75.0%; in the case of repeated excision, it increases by 12.0% [9]. The incision for CLC is deep, sometimes reaching the muscular fascia, due to the need to excise deep-lying abnormal lymphatic cisterns. To determine the most accurate cut boundaries, visualization methods, in particular magnetic resonance imaging (MRI), are highly effective. The authors note that, by determining the adequate extent of surgical intervention, the use of MRI reduces the chance of relapse of dermatosis [10]. Positive results have been described using a 5 W carbon laser in continuous mode. Electrocautery, like cryotherapy, is used in cases of superficial CLC. Sclerotherapy with sodium tetradecyl sulfate 0.25–0.5% and polidocanol 0.5% is used, but the drugs are not approved by the US Food and Drug Administration (FDA) for the treatment of CLC. Radiation therapy is not used because there is a risk of malignancy. Thus, the literature describes cases of transformation of lymphangioma into Dabsky tumor (endovascular papillary angioendothelioma) and lymphangiosarcoma [25, 26].
When a tumor is infected, cephalexin 500 mg 2–4 times a day for 10 days or doxycycline 100 mg 2 times a day for 10 days is used as antibacterial therapy if methicillin-resistant Staphylococcus aureus (MRSA) is detected. in the separated elements [27].
We present an observation of a clinical case.
Clinical case
A 54-year-old woman came to the dermatovenerological clinic with complaints of blistering rashes on the skin of the anterior surface of the chest, right shoulder, without subjective sensations. From the anamnesis it is known that she considered herself ill for two years, when blisters first began to appear in the area of the armpit on the right. I periodically noted the appearance of similar elements on the skin of the chest and shoulder. When the vesicles were injured, a yellowish fluid was released. I lubricated it myself with a solution of boric acid, alcohol, chlorhexidine - without effect. The patient has a history of radical left mastectomy for cancer of the left breast T1cN0M0 in 1999, lymphostasis on the right. Right mastectomy in 2015 for right breast cancer T1N0M0.
Status specialis: the rash is asymmetrical, located on the anterior surface of the chest in the mammary areas, the medial surface of the left shoulder. They are represented by miliary and lenticular papules of brown and purple colors, on top of which there are small (up to 0.2 cm in diameter) vesicles with serous contents, rising above the surrounding skin like “frog eggs”. Dermoscopically, lacunae are identified, filled with orange and purple contents, separated by white partitions.
Based on a clinical examination and dermoscopic picture, a diagnosis of limited lymphangioma of the skin of the chest and right shoulder was made. It is recommended to prevent trauma to elements, use solutions of antiseptics, aniline dyes, and antibacterial patches.
The described case is presented due to the rarity of this dermatosis.
Literature
- William J., Timothy B., Dirk E. Andrews' Diseases of the Skin // Clinical Dermatology. 2005, p. 585.
- Bauer BS, Kernahan DA, Hugo NE Lymphangioma circumscriptum – a clinicopathological review // Annals of Plastic Surgery. 1981. Vol. 7. P. 318–326.
- Morris M. Lymphangioma circumscriptum // International Atlas of Rare Skin Diseases. London: Lewis. 1889. P. 1–4.
- Peachey RD, Lim CC, Whimster IW Lymphangioma of the skin. A review of 65 cases // British Journal of Dermatology. 1970. Vol. 83. P. 519–527.
- Fernandez G. Lymphangioma // eMedicine Dermatology. 2007. URL https:// www.emedicine.com/DERM/topic866.htm (Accessed 26 Nov 2019).
- Fatima S., Uddin N., Idrees R. Lymphangioma Circumscriptum: Clinicopathological Spectrum of 29 Cases // Journal of College of Physicians and Surgeons Pakistan. 2015. Vol. 25. No. 9. P. 658–61.
- Schwartz RA Arterial vascular malformations including hemangomias and lymphangiomas // eMedicine Pediatrics. 2009. URL https://emedicine.com/ped/topic2926.html (Accessed 26 Nov 2019).
- Filston HC Hemangiomas, cystic hygromas, and teratomas of the head and neck // Seminars in Pediatric Surgery. 1994. Vol. 3. P. 147–159.
- Flanagan BP, Helwig EB Cutaneous lymphangioma // Archives of Dermatology. 1977. Vol. 113. P. 24–30.
- Whimster IW The pathology of lymphangioma circumscriptum // British Journal of Dermatology. 1976. Vol. 94. P. 473–486.
- Martínez-Menchón T., Mahiques-Santos L., Febrer-Bosch I. Lymphangioma Circumscriptum: An Example of Whimster's Hypothesis // Pediatric Dermatology. 2004. Vol. 21. No. 6. P. 652–654.
- Asano S., Endo H., Sagami S. An ultrastructural study of localized lymphangioma circumscriptum // Archives of Dermatological Research. 1978. Vol. 262. P. 301–309.
- Mordehai J., Kurzbart E., Shinhar D. Lymphangioma circumscriptum // Pediatric Surgery International. 1998. Vol. 13. P. 208–210.
- Erkilic S., Kocer NE, Mutaf M. Giant lymphangioma circumscriptum mimicking wart in a 13-year-old girl // The Journal of Dermatology. 2006. Vol. 33. P. 501–503.
- Horn LC, Kuhndel K., Pawlowitsch T. Acquired lymphangioma circumscriptum of the vulva mimicking genital warts // European Journal of Obstetrics & Gynecology and Reproductive Biolog. 2005. Vol. 123. P. 118–120.
- Yagmurlu A. et al. A children’s disease of rarity: “scrotal lymphangioma circumscriptum” // International Urology and Nephrology. 2004. Vol. 36. P. 229–233.
- Yildiz F., Atahan IL, Ozyar E. Radiotherapy in congenital vulvar lymphangioma circumscriptum // The International Journal of Gynecological Cancer. 2008. Vol. 18. P. 556–559.
- Mabel DA Gomides, Lais D. Costa. Cutaneous lymphangioma circumscriptum: The relevance of clinical, dermoscopic, radiological, and histological assessments // Clinical Case Reports. 2021. Vol. 7. No. 4. P. 612–615.
- Child FJ, Werring DJ, Vivier AW Proteus syndrome: diagnosis in adulthood // British Journal of Dermatology. 1998. Vol. 139. P. 132–136.
- Shim JH, Lee DW, Cho BK A case of Cobb syndrome associated with lymphangioma circumscriptum // Dermatology. 1996. Vol. 193. P. 45–47.
- Elkin V.D., Mitryukovsky L.S., Sedova T.G. Selected dermatology. Rare dermatoses and dermatological syndromes. Il. reference on the diagnosis and treatment of dermatoses. Ed. second, rev. and additional Perm: IPK Zvezda, 2004. 943 p.
- Van Vonno N. A case of carcinoma telangiectaticum // The British Journal of Dermatology and Syphilis. 1933. Vol. 45. P. 423–424.
- Bond J., Basheer MH, Gordon D. Lymphangioma circumscriptum: pitfalls and problems in definitive management // Dermatologic Surgery. 2008. Vol. 34. P. 271–275.
- Emanuel PO, Lin R., Silver L. Dabska tumor arising in lymphangioma circumscriptum // Journal of Cutaneous Pathology. 2008. Vol. 35. P. 65–69.
- King DT, Duffy DM, Hirose FM Lymphangiosarcoma arising from lymphangioma circumscriptum // Archives of Dermatology. 1979. Vol. 115. P. 969–972.
- Bryan A., Galen F. Lymphangioma Circumscriptum (Lymphangiectasia, Dermal Lymphangioma) // Dermatology Advisor. 2017. URL https://www.dermatologyadvisor.com/home/decision-support-in-medicine/dermatology/lymphangioma-circumscriptum-lymphangiectasia-dermal-lymphangioma/ (Accessed 27 Nov 2019).
M. A. Ufimtseva1, Doctor of Medical Sciences Yu. M. Bochkarev, Candidate of Medical Sciences A. A. Komarov A. S. Shubina
Federal State Budgetary Educational Institution of Higher Education USMU of the Ministry of Health of Russia, Ekaterinburg
1 Contact information
DOI: 10.26295/OS.2020.35.92.006
Limited lymphangioma in an oncology patient/ M. A. Ufimtseva, Yu. M. Bochkarev, A. A. Komarov, A. S. Shubina For citation: Attending physician No. 5/2020; Page numbers in the issue: 33-35 Tags: skin, lymphatic vessels, malignant neoplasms
Possible complications with lymphangioma
Despite its benign nature, lymphangioma
poses a serious danger to the body. The main danger is due to the threat to the body during childbirth, both for the mother and for the unborn child. The pathology poses a danger not only to newborns, but also to adolescent children, causing serious harm to their health. Neoplasms that arise in the fetus create difficulties for the woman in labor during the passage of the fetus through the birth canal. Often there is compression of neighboring organs, displacement of tissues, causing congenital hypoxia and coronary heart disease and other organs in the newborn.
Lymphangioma that appeared after birth in a newborn
, gives every reason to suspect that the child has serious impairments in the functionality of vital organs. Over time, complete loss of functionality of individual organs may occur. Based on the fact that the defect during birth affects organs in the head and neck area, the newborn may have problems with the respiratory process and make it difficult to swallow.
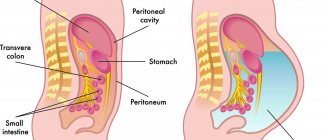
The most common complication resulting from developing pathology is lymphatic malformation, formed as a result of any inflammatory process. Complications can arise as a result of otitis media, acute respiratory viral infections, respiratory diseases, and lymphadenitis. One of the severe complications, the likelihood of which increases as a result of the development of a benign tumor in the lymphatic system, is the leakage of lymph into the chest and peritoneum, which poses a threat to the patient’s life.
Treatment methods for lymphangioma in Israel
The choice of therapeutic tactics depends on the specific case. At Top Ichilov, the treatment protocol is compiled by a team of specialists. This approach allows you to get the most complete picture of the patient’s health status and outline the best direction for further action. Treatment of lymphangioma in Israel may include the following methods:
- Sclerotherapy. This is an innovative type of treatment for macrocystic lymphangiomas, which has already proven its effectiveness. The tumor-destroying drug Picibanil is injected directly into the tumor under ultrasound guidance. Since the injections are quite painful, children are given them under anesthesia. Treatment of lymphangioma without surgery in Israel using this method is carried out by qualified specialists who have experience not only in performing the procedure, but also in the further management of the patient.
- Radiofrequency ablation. Performed percutaneously. The doctor inserts a thin needle into the tumor area, through which a high-frequency current is applied, which destroys the tumor tissue. The Top Ichilov Clinic has modern systems for radiofrequency ablation, which allow highly precise and effective treatment of the tumor.
- Cryodestruction. This method is used mainly for the treatment of simple lymphangiomas of the oral mucosa. The tumor is destroyed by application or spraying of liquid nitrogen. Several treatment sessions are sometimes required to achieve optimal results.
- Laser destruction. Neoplasm tissues are destroyed by thermal exposure to a laser. The advantages of this technique are: immediate coagulation of blood and lymphatic vessels, reduced postoperative pain, minimal risk of infection and absence of scars. This is a relatively new treatment for lymphangioma in Israel, the reviews of which are mostly positive.
- Surgical removal. Lymphangiomas often grow into muscle tissue, affecting nerves and blood vessels, which complicates their surgical removal. At the Top Ichilov Clinic, experienced surgeons perform surgical treatment of lymphangiomas. They strive not only to completely remove the tumor to avoid recurrence of the disease, but also to do it as carefully as possible so as not to leave extensive scars. In case of significant damage, plastic surgery of the resulting defect is performed.
Diagnostics
Lymphangioma in 90% of cases manifests itself in the first year of a child’s life. Increasing thickenings in the lymph nodes can grow with the child, but they can also change their size dramatically. Simple lymphangiomas are hilly thickenings of the skin that do not stand out sharply. The surface of the skin may be moist - this is called lymphorrhea.
Cystic lymphangioma looks like an elastic formation that is covered by stretched skin. In some cases, the formation of a blue tint is noticeable through the skin. This tumor most often occurs in children on the neck. Cystic lymphangiomas increase in size slowly, but during their growth they can compress internal organs, tracheas, and nerves that are located nearby.
Cavernous type lymphangioma is determined by the presence of swelling; its outlines are fuzzy and blurry. When pressed, such a lymphangioma decreases in volume, and then gradually restores the volume. Most often found on the lips, tongue, neck, parotid areas, cheeks.
Why choose Top Ichilov clinic
- The most modern methods of treating lymphangioma in Israel
- Possibility of non-surgical treatment
- Fast and high-quality diagnostics with a second opinion
- Comfortable conditions for staying in the hospital: comfortable and clean rooms, equipped with everything necessary, polite medical staff
- Loyal prices, flexible payment system
- Personal case manager, organizing the process of diagnosis and treatment, as well as taking upon himself the solution of all everyday problems
- 5
- 4
- 3
- 2
- 1
(3 votes, average: 3.7 out of 5)
Diagnosis of lymphangioma in Israel
For patients coming to Israel for treatment, the duration of treatment is very important, because every day of stay in a foreign country costs money. Top Ichilov specialists know about this, so the diagnostic process here is clearly coordinated and does not take more than three days.
- Day 1
- Day 2
- Day 3
Day 1: consultation with a leading surgeon
Your personal assistant will schedule a doctor's consultation for you in advance, so you won't have to waste time searching for the right specialist or waiting in lines. At your first visit to your doctor, you will undergo a physical examination. In addition, the doctor will ask you the necessary questions and review your medical documents. He will then draw up a plan for subsequent diagnostic activities.
Day 2: diagnostic procedures
Diagnosis of lymphangioma in Israel may include the following tests:
- Ultrasound examination. This is an informative and inexpensive method for diagnosing lymphangioma.
- Angiographic examination. Allows you to accurately determine which blood vessels are involved in the pathological process.
- Biopsy. Taking a small area of the tumor for histological analysis. Helps to distinguish lymphangioma from other neoplasms with similar clinical manifestations.
- Computed and magnetic resonance imaging. These studies are usually performed as part of preoperative planning. The high discriminative power of MRI helps to clearly distinguish between pathological and healthy tissues and avoid incomplete or unnecessary resection.
- General and genetic blood tests.
Day 3: medical consultation
After the results of diagnostic tests are ready, your attending physician will convene a consultation of specialists. Doctors from various fields will take part in it. This approach allows you to comprehensively evaluate each specific case of the disease and choose the optimal treatment tactics. Another advantage of collegial diagnosis is the minimal risk of medical error. The patient immediately receives a second opinion and can be confident in the correctness of the chosen line of therapy.