Pathologies of the vascular system of the eye are recognized as one of the main factors of low vision, blindness, and therefore limited vision in people of various age categories. In recent years, there has been an increase in ischemic eye diseases, which is due to the widespread prevalence of atherosclerosis, hypertension, coronary heart disease, and diabetes mellitus.
A classification system for ocular ischemia has not yet been developed. There is a close relationship between lesions of individual parts of the circulatory system and the mechanisms responsible for the development of ischemia. In this regard, ischemic eye diseases are characterized by polyetiology, the absence of a single pathogenesis and the diversity of the clinical picture.
Thus, the clinical picture of ischemic damage to the posterior segment of the eye is largely determined by the characteristics of blood circulation in the area of the optic nerve and retina.
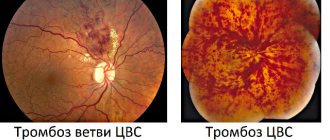
Ischemic processes occurring in the eye are usually divided into acute and chronic. Acute ischemia of the posterior ocular segment is characterized by circulatory disorders of the central retinal artery (CRA) or its central vein (CVS), anterior or posterior ischemic and acute toxic neuropathy.
Acute ischemia becomes a consequence of chronic ocular ischemia (diabetic or hypertensive angioretinopathy, degenerative changes in the retina, stenosis of the carotid or orbital arteries, temporal arteritis). The basis of ischemia is common angiospastic diseases, traumatic lesions of the eye and head. There have been cases of the occurrence of ischemic neuropathies with impaired blood flow in the CAS and CVS, as well as in their branches, with hypotension, taking certain medications and after surgical operations, if the predisposing factors were: microembolization, anemia, disorders of the blood coagulation or anticoagulation systems.
Acute disorders of the blood supply to the retina and optic nerve in the vast majority of cases cause partial loss of vision or blindness. The prognosis of the condition is always serious, but often not hopeless. Often, under the influence of treatment, the process improves or stabilizes. Quite often repeated courses of treatment are necessary.
Often, ischemic optovascular syndrome is a harbinger of ischemic coronary and cerebral attacks. In this regard, not only eye diseases, but also concomitant diseases require long-term careful treatment.
What it is
The disease is a condition accompanied by spasm, blockage (ischemic) or rupture (hemorrhagic) of a blood vessel in the eyeball. An attack can develop acutely or be sluggish. In the first case, we are talking about the appearance of severe pain, loss of certain parts of vision or complete blindness, numbness of the limbs. A sluggish stroke can cause alternations between deterioration and improvement of well-being, and minor visual disturbances. Whatever the symptoms, you should not let the disease take its course; you should consult a doctor as soon as possible.
diagnosing
Sudden vision loss is a medical emergency.
To diagnose an eye stroke, doctors may need to perform tests on the retina. These may include
- Eye dilation with drops for easier vision on the retina.
- Using a dye and camera to take photographs of the retina, known as fluorescein angiography. The dye is injected through the arm and allows the doctor to better see the veins and arteries of the retina.
- Checking the pressure in the eyes using air flow.
- A slit lamp examination, which uses eye drops, a special light, and a microscope to examine the inside of the eyes.
- Vision tests, such as reading eye charts and testing side or peripheral vision.
These tests are painless and are performed by an eye doctor known as an ophthalmologist.
Symptoms depending on the type
For timely diagnosis of any eye diseases, every person must pay close attention to their vision. The concept of ocular stroke includes several conditions, among which are occlusion of an artery and detachment of blood vessels from the retina, blockage of the central artery, and detachment of the central retinal vein. Let's consider the signs characteristic of each pathology.
Artery occlusion and detachment of blood vessels from the retina
The retina is the nervous tissue that is responsible for image perception. Under the influence of various reasons, its detachment may occur. The following symptoms are a signal for immediate medical examination:
- narrowing of the field of view. In a normal state, a person should clearly see the world around him. Even if he looks forward, peripheral vision catches objects that are to the side. A decrease in the field of vision indicates the development of serious disorders;
- the appearance of flies, stars, sparks before the eyes. This symptom is especially pronounced when light enters the eyes;
- pain in the eyeball area;
- the formation of small or larger hemorrhages.
As already mentioned, the symptoms of an ocular stroke may vary depending on the characteristics of the disease. Often the development of pathology is indicated by a sharp deterioration in vision and the appearance of white or grayish spots before the eyes. In many cases, increased blood pressure is diagnosed.
The attack is accompanied by eye pain and blurred vision
During a visual examination, the ophthalmologist notes characteristic vascular networks and areas of hemorrhage. The patient reacts painfully to light rays, discomfort appears when moving the eyes.
Blockage of the central artery
The eyes are nourished by numerous vessels. This has important physiological significance, since the blood carries oxygen and other essential substances that are required for the normal functioning of the visual organ. When the central retinal artery is blocked, signs may include the following:
- partial or complete loss of lateral vision;
- distortion of the outlines of objects, blurred visual images;
- the appearance of areas on the eye that are unable to perceive light impulses (blind spots);
- pain, dryness.
If you notice these symptoms, you should immediately consult a doctor. The condition is seriously dangerous and can lead to blindness.
Division of the central retinal vein
The following clinical signs indicate separation of the central retinal vein:
- sharp deterioration of vision or its complete loss;
- the appearance of cross syndrome, characterized by impaired eye mobility and loss of sensitivity of the limbs on the opposite side;
- loss of individual fields of vision;
- severe pain accompanied by constriction of the pupil;
- decreased eye mobility;
- split picture;
- development of strabismus.
Particular attention is paid to the development of the symptom of flickering darkness. In this case, the patient experiences fog before the eyes, glare of light, and white spots. Skin sensitivity is impaired in various places. Often this clinical picture is typical for people suffering from persistent arterial hypertension, migraines, atherosclerosis and other pathologies. The symptom of flickering darkness is paroxysmal in nature, periodically the person experiences relief, after which the symptoms repeat.
Spots before the eyes or loss of visual fields are common signs of the disease
Important! Any type of disorder without the necessary medical treatment leads to partial or complete loss of vision.
Methods for improving vision after a stroke
After a stroke, artificial tears, Korneregel, Taufon, Normax, Taurine are prescribed. Hydration is extremely important for patients who have been in a coma.
During the rehabilitation period, you need to reconsider your diet. After a stroke, it is recommended to eat more carrots, yellow peppers, pumpkin, egg yolks and fish. Cataract prevention is provided by grapes, blueberries and onions.
After a stroke, it is useful to massage with hot or cold compresses. This helps relax the eyes and improve blood circulation. It is enough to wet one towel in cold water and the other in warm water, and alternate them for 5-10 minutes.
The usual tossing of a ball or ball helps in restoring vision. You need to throw the object back and forth from the affected side. Focusing your gaze on an object will help to establish synchronicity between movements and vision.
Computer programs will help to rehabilitate vision after a stroke. One of these programs shows a black square; at certain intervals, a cluster of one hundred dots flashes on the side of the affected eye. Exercises on the computer take 15-20 minutes a day. The course of treatment is several months.
Comparative exercises allow you to check the extent of visual focus impairment. They make it possible to determine the required degree of rehabilitation therapy. The patient should close his eyes and direct his gaze to the injured side of the body. After determining the correct (according to the patient) direction, the eyes are opened, and the doctor determines the proximity of the gaze from the desired direction.
Compensatory vision therapy stimulates the areas of the brain that support vision. It includes scanning, visual field recognition and prism exercises. The visual field can be adapted by moving images from invisible zones.
Prisms in ophthalmology are used to correct various visual impairments. The type and placement of the prism will be determined by the symptoms. In case of double vision, the prism is placed on a glass lens, which allows you to align the direction of view. Spatial neglect requires the use of a prism on the left side of the visual field so that it reflects objects on different sides.
Restorative vision therapy aims to stimulate nerve connections in the brain. There are different techniques for all types of visual impairments.
Usually, surgical treatment of the organs of vision does not help anything after a stroke, because the problem lies in the brain. Only in some cases does surgery correct double vision by affecting the eye muscles.
Main reasons
An ocular stroke can develop regardless of age and gender under the influence of various provoking factors.
Common reasons:
- hypertonic disease. Patients suffering from a persistent increase in blood pressure are at risk for the disease, since their vessels are constantly exposed to high stress;
- stressful situations and chronic fatigue. It has been proven that excessive production of the hormone adrenaline does not have the best effect on veins and capillaries. Overfatigue is also considered a cause of deterioration in the condition of vascular walls;
- low blood clotting. This condition promotes hemorrhages;
- hereditary predisposition and congenital vascular weakness;
- prolonged eye strain. The risk group includes people who are forced to spend a long time behind a computer screen or work with papers;
- diseases accompanied by impaired blood flow;
- diabetes mellitus type II;
- bad habits (drug use, alcohol use, smoking);
- lack of vitamins and minerals.
A common cause of ocular stroke is the use of certain groups of medications. This includes hormonal medications, oral contraceptives, and some other medications.
All these factors contribute to the formation of blood clots (thrombi, emboli). They are formed on the walls of blood vessels from cholesterol, bacteria, and particles of calcium crystals. When a blood clot breaks away from the wall, it enters the bloodstream and can cause a blockage in any part of the body, including the eyes. In turn, this provokes acute circulatory disorders and decreased visual function. If the blood clot resolves on its own or with timely treatment with drug therapy, vision is partially or completely restored. In severe cases, blindness occurs.
Hypertension and other vascular diseases are a common cause of stroke
For the organs of vision, the greatest threat is posed by emboli formed in the area of the coronary or carotid artery. In diseases of the cardiovascular system, infectious pathologies, allergies, poor coagulation and other conditions, the blood clot breaks away from the vessel wall and closes the lumen of the central vessel of the organ of vision.
In addition, the causes of stroke include the following provoking factors:
- blockage with subsequent rupture of the vertebral artery. This often happens with diseases such as osteochondrosis, back injuries, intervertebral hernias;
- severe increase in intracranial pressure. This is another reason that leads to impaired nutrition of the eye.
Important! Patients at risk should be attentive to their health and undergo annual preventive examinations with an ophthalmologist.
Treatment
In case of acute obstruction of the central nervous system or its branches, it is necessary to immediately administer general and local vasodilators: a nitroglycerin tablet under the tongue, inhalation of amyl nitrite (a few drops on a cotton swab), 0.5 ml of atropine solution 0.1% retrobulbar, intravenous 0.3-0, 5 ml of xanthinol nicotinate solution 15%, intravenously 10 ml of aminophylline solution, intramuscularly or intravenously 1-2 ml of papaverine solution or xanthinol nicotinate solution 15%.
For thrombosis of the central nervous system, anticoagulant therapy, control of blood clotting and prothrombin time are recommended: fibrinolysin with retrobulbar heparin (5-10 thousand units), heparin up to 10 thousand. ED subcutaneously 6 times a day, then use indirect anticoagulants - finilin up to 4 times a day, 0.03 mg for the first few days, then once a day.
Additionally, anti-sclerotic and vitamin therapy is used (miscleron, methionine, vitamins A and C, B6, B12).
By contacting the Moscow Eye Clinic, each patient can be sure that highly qualified refractive surgeons - one of the best Russian specialists in this field - will be responsible for the results of surgical intervention. The high reputation of the clinic and thousands of grateful patients will certainly add to your confidence in the right choice. The most modern equipment for the diagnosis and treatment of eye diseases, some of the best specialists and an individual approach to the problems of each patient are a guarantee of high treatment results at the Moscow Eye Clinic.
You can find out the cost of a particular procedure or make an appointment at the Moscow Eye Clinic by calling 8 (800) 777-38-81 (daily from 9:00 to 21:00, free for mobile phones and regions of the Russian Federation) or using the form online entries.
Diagnostics
Diagnosis of pathology is carried out in a hospital setting. If a patient is suspected of developing a stroke, he urgently needs to undergo examination by a neurologist. The doctor evaluates a person’s reflexes, his speech, orientation in space, and vision. If a stroke is confirmed, consultation with an ophthalmologist is also required.
Among the instrumental diagnostic techniques used:
- computed tomography;
- CT angiography (vascular visualization);
- Magnetic resonance imaging.
These methods help to determine the location and degree of occlusion and select the necessary treatment measures. X-rays of the person are often performed to identify the presence of malformations, vascular aneurysms, and other abnormalities. Ultrasound and electrocardiography are used to identify pathologies that caused the development of an ocular stroke. Blood and urine tests show glucose concentrations, electrolytes and kidney metabolites.
To diagnose an attack, a comprehensive examination is used
In addition to confirming an ocular stroke, these techniques make it possible to identify at an early stage such dangerous conditions as renal failure, hypertensive crises, heart attacks and others.
At-risk groups
Most patients who suffered an ocular stroke suffered from atherosclerosis and its manifestations (cardiac ischemia, angina, hypertension), and diabetes. The next position as a direct etiological factor is occupied by rheumatic pathologies, then temporal arteritis, vascular diseases.
Additional risk groups:
- people whose work activity involves working at a computer (eye strain);
- people exposed to frequent and prolonged stressful situations (doctors, lawyers, military personnel and emergency responders);
- age over 40 years;
- smokers;
- persons who abuse alcohol;
- frequently ill people (decreased immunity);
- family history of atherosclerosis, hypertension, diabetes, heart and vascular diseases.
Treatment tactics
Treatment for stroke always depends on several aspects. This includes the type of pathology, features of its course, causes, symptoms in the patient and some other factors. Laser coagulation is considered the most effective and safe method. The use of a laser allows you to effectively get rid of a blood clot, which helps restore blood flow in the affected area and prevent dangerous complications. The same technique is used for retinal detachment.
Another type of therapy is hyperbaric oxygen therapy. Its essence is the use of oxygen under pressure. In this case, the patient is in a hermetic pressure chamber.
Drug therapy includes groups of drugs designed to eliminate a blood clot, normalize blood circulation, relieve spasms, and normalize blood pressure. Treatment includes:
- antihypertensive drugs. To normalize blood pressure, the patient is prescribed diuretics, beta blockers, calcium antagonists, and ACE inhibitors. The decision on the type of drug in a particular case is made by the attending physician, depending on the characteristics of the course of the disease;
- anticoagulants. The main goal of therapy for ocular stroke is to restore normal blood flow. Since the cause of circulatory disorders is most often a blockage with a blood clot, to eliminate it, agents are prescribed that help dissolve blood clots;
- antispasmodics. These medications relieve spasm and pain that develop during an attack.
Treatment tactics depend on the characteristics of the pathology
Depending on the patient’s concomitant pathologies, other medications may be prescribed, for example, non-steroidal anti-inflammatory drugs, corticosteroids, narcotic analgesics, etc.
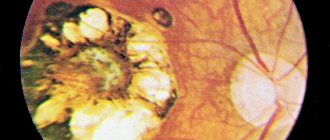
Complications and consequences
Visual impairment can become irreversible after a stroke, even leading to blindness, if timely assistance is not provided to the patient. This is the main and most dangerous complication of the disease. An equally serious consequence is retinal detachment and macular defects, which also leads to vision loss. The transition of the pathological process to the second eye and optic nerve atrophy occur less frequently.
When the retina lacks nutrition, the body begins to come up with workarounds. This is how new blood vessels form – neovascularization. This is not a healing process - the new vessels are too brittle and tortuous, and the risk of rupture is high. There are known cases of neovascularization of the optic nerve head and neovascular glaucoma.
Prevention
Like many other diseases, ocular stroke can be prevented by following simple preventive measures. First of all, it is worthwhile to promptly treat various diseases of the cardiovascular system and respiratory organs. This is explained by the fact that it is pathologies of the heart, arteries and veins that often cause ruptures or spasms of blood vessels. Under no circumstances should you self-medicate. Medications should be selected by a doctor.
In addition, it is recommended to maintain a balanced diet and proper drinking regimen. Saturating the body with beneficial vitamins and minerals will ensure the health of blood vessels and all internal organs. To do this, you should give up a large amount of animal fats, limit the consumption of salt, sugar, fatty, smoked, and sour foods. It is better to give preference to plant products, vegetables, fruits, preferably raw or baked.
Another important aspect is giving up bad habits and sufficient physical activity. These and other activities will help maintain not only the health of your eyes, but also your entire body for many years.
Classification of apoplexy
There are two forms of stroke:
- Ischemic;
- Hemorrhagic.
Ischemic stroke is caused by an acute decrease in blood flow (ischemia), usually due to a blood clot that blocks a blood vessel in the brain. This form of apoplexy is the most common type of stroke, accounting for 80 to 85% of all strokes.
An ischemic stroke in the brain stem has especially serious consequences, because vital centers that are responsible for breathing control and consciousness are located there. An example of a brainstem infarction is thrombosis of the basilar artery: in severe cases, this causes complete paralysis of all limbs (tetraparesis) and coma or immediate death.
Ischemia
Hemorrhagic stroke
Hemorrhagic stroke occurs when abnormalities in the coagulation system, high blood pressure, or pathological changes in the vessel wall lead to bleeding in the brain. Between 15 and 20 percent of all apoplexies fall into this category.
Almost a million people in Russia suffer from apoplexy every year. 900,000 of them have their first stroke. Apoplexy occurs mainly in older people. As their proportion of the population steadily increases, the number of stroke patients is likely to increase as well.
Brain strokes mainly affect older people, but can also occur at a young age. Even newborn children in the mother's body can already have apoplexy. Possible causes include coagulation disorders and cardiovascular pathologies. Sometimes an infectious disease causes bleeding in the brain tissue in children.
In Russia, apoplexy is diagnosed every year in about 1,000 children and adolescents. However, experts believe the actual number is much higher because diagnosing stroke in children is more difficult. The reason is that brain maturation has not yet been completed, so apoplexy in children is often detected only after several months or years. For example, partial paralysis does not appear in infants until six months later.
Prevention
Testing for cardiovascular disease is key to preventing ocular strokes. This may include regular cholesterol and blood pressure checks, as well as discussion of other risk factors for heart disease, such as family history, diet and lifestyle.
Heart disease risk factors play a role in the risk of ocular strokes. An article in the journal Eyes found that 64% of people had at least one new, undiagnosed risk factor for heart disease that was discovered after a stroke. The biggest factor for these people was high cholesterol.
In general, to maintain healthy blood vessels and prevent eye stroke, people should do the following:
- exercise regularly; The Physical Activity Guidelines for Americans recommend 2.5 hours per week.
- Eat a healthy diet including plenty of fruits, vegetables, whole grains and unsaturated fats.
- work with a nutritionist, as recommended for some people.
- avoid smoking or quit smoking
- work with your doctor to treat other conditions, such as diabetes.
Perspective
The long-term outlook for people with eye stroke can vary greatly. This depends on the severity of the stroke, the success of treatment, and the arteries or veins affected.
An article in the journal Eye, as mentioned above, found that 80% of people who have a stroke have significant vision loss by 20400 or worse.
In some cases, a person's vision may be restored over time. A study in the American Journal of Ophthalmology found that vision loss may improve for many people, depending on the type of ocular stroke.
https://www.youtube.com/watch?v=p_BQonMqWcQ
The authors state that identifying the type of ocular stroke is an important factor in how well a person can see after it.
Conclusion
Living a healthy lifestyle isn't just good for your heart. It can improve overall health and reduce the risk of problems such as eye stroke and vision loss.
Symptoms
Paralytic strabismus manifests itself with a complex of classic symptoms for a group of diseases:
- increased visual fatigue;
- difficult motor activity of the affected eye due to the inability to direct gaze in the direction opposite to that on which the paralyzed muscle is located;
- deviation of the healthy eye to the side when trying to focus on an object with the affected eye.
In acquired forms of paretic strabismus
patients complain of double vision, dizziness, and inability to focus on an object. To remove these inconveniences, patients are forced to exclude the affected organ from the visual process by covering it or turning their head towards the pathological eye.
Typical signs of the paralytic form of strabismus are associated deviations from the norm:
- inability to determine the location of an object when examining it with the affected eye;
- drooping upper eyelid on the affected side;
- deviation of the eyeball towards the temple and downwards;
- lack of pupil reaction to light;
- complete immobility of the eye (characteristic of multiple paralysis of the oculomotor muscles).
In the vast majority of cases, patients have unilateral eye damage. Bilateral is considered a rare occurrence.