Arterial hypertension (AH) has long been rightly considered one of the significant problems of modern healthcare. It is the main factor contributing to the development of pathologies of the heart and blood vessels. Both most strokes and kidney failure occur due to hypertension.
If hypertension continues for a long time and becomes persistent, renal pathologies begin to progress rapidly and often end in the terminal stage, followed by death. In turn, if kidney function is reduced, this provokes an increase in blood pressure.
Chronic kidney disease is understood as both the main cause of hypertension and one of the complications of arterial hypertension, which cannot be stablely relieved and controlled.
Association between hypertension and CKD
Arterial hypertension and CKD have close and complex relationships with each other. Hypertension is often considered both a cause and a consequence of chronic kidney disease. It is widespread and rarely controlled. The complex interaction of these dangerous pathologies with each other provokes unfavorable outcomes of diseases of the heart, blood vessels and brain.
The pathophysiological mechanisms of increased pressure in renal pathology are complex and are the consequences of many factors such as:
- decrease in kidney cell mass;
- delays in sodium excretion from the body;
- increased activity of the sympathetic nervous system;
- increase in extracellular volume;
- activation of hormonal activity.
Patients with CKD often have high blood pressure with high risks. Hypertension may have:
- hidden form;
- resistant course.
Sometimes it occurs at night.
Hypertension and CKD should be carefully studied to slow the development of cardiac and renal dysfunction.
Hypertension drugs
Blood pressure medications for kidney disease also have a number of contraindications. The most gentle include angiotensin-converting enzyme inhibitors: fonisopril, enalapril, captopril. They increase glomerular filtration, sometimes increasing creatinine and potassium. Possible risks are observed in elderly patients, so treatment should be carried out under medical supervision. Reception is contraindicated:
- with stenosis of the renal arteries (both or only);
- heart failure;
- severe renal failure in combination with diuretic therapy.
The group of calcium channel blockers is no less effective; diuretics are also actively used.
When taking medications for kidney pressure, the amount of potassium in the blood serum should be monitored. Its increase is provoked by a deficiency of renal function. The likelihood of hyperkalemia increases when taking drugs from different groups simultaneously. Therapy is started with small doses, and when increasing, a control test is prescribed.
Problems of chronic kidney disease
Now CKD represents a real epidemiological problem, since the number of patients suffering from it is increasing. Prolonged and recurrent course of the disease leads to the development of end-stage renal failure, resulting in huge costs for the healthcare system.
As kidney function gradually decreases, arterial hypertension also increases, which, as a rule, always accompanies CKD.
Hypertension is an equally serious medical problem, since it is the main cause of the development of:
- all types of strokes;
- pathologies of the heart and blood vessels.
In this case, chronic kidney disease can act both as a cause of arterial hypertension and as its complication if the disease proceeds uncontrolled.
The prevalence of hypertension and CKD among adult patients looks something like this:
- AH - from 25 to 30%;
- CKD - about 15%.
If a person already suffers from chronic kidney disease, he is also diagnosed with arterial hypertension. Conducted epidemiological studies indicate that from 67 to 71% of patients suffer from hypertension, and the percentage of elderly people makes up 82% of the total number of clinical cases. When CKD progresses to the later stages of its course, hypertension is observed in 90% of patients.
When a patient is on dialysis, the frequency of hypertension changes, since the methods of controlling blood pressure are different (pre-, post-dialysis, outpatient, etc.). However, research shows that hypertension affects:
- from 50 to 80% percent of patients undergoing hemodialysis;
- about 30% of those undergoing peritoneal dialysis.
It has been said many times that arterial hypertension can be both a cause and a result of the development of chronic kidney disease.
The prevalence, severity level and ability to control the disease are influenced by:
- causes of renal pathology;
- albumin level in urine;
- hereditary factor;
- socioeconomic reasons.
Ethnic and racial factors should also be taken into account.
TREATMENT OF ARTERIAL HYPERTENSION IN CHRONIC KIDNEY DISEASE
The present paper deals with the present-day problems of nephrogenic arterial hypertension (AH), with the prevalence of AH in chronic renal diseases, with the mechanisms of its development and progression, as well as with its treatment policy. While discussing therapeutical problems in AH, great attention is given to the first-line drugs angiotensin-converting enzyme inhibitors and calcium channel blocking agents. The basic spectrum of these groups of drugs is presented, the mechanisms of their nephroprotective action are described.
THEM. Kutyrina – Doctor of Medicine. Sciences, Professor of the Department of Nephrology (Head-Corresponding Member of the Russian Academy of Medical Sciences Prof. I.E. Tareev) Faculty of Postgraduate Education MMA named after. THEM. Sechenova Professor IMKutyrina, MD, Department of Nephrology (Head is I.Ye.Tareyeva, Corresponding Member of the Russian Academy of Medical Sciences), Faculty of Postgraduate Training, IMSechenov Moscow Medical Academy
TO
Classification of arterial hypertension (AH) at the present stage is carried out according to three leading signs: blood pressure (BP), degree of target organ damage, etiology.
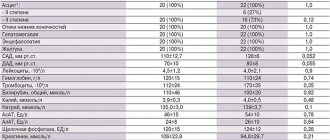
In recent years, there has been a tendency to tighten the diagnostic criteria for hypertension, and currently hypertension is understood as a condition in which the blood pressure level exceeds 140/90 mm Hg. or exceeded it at least 3 times when measuring blood pressure over 3 to 6 months. In table Figure 1 shows the modern classification of hypertension, presented by experts from the National Joint Committee on the Detection, Evaluation and Treatment of High Blood Pressure (USA, 1993). A blood pressure level of up to 120/80 mm Hg is considered optimal. Blood pressure is considered normal if diastolic pressure does not exceed 90 mm Hg when measured twice, and systolic pressure does not exceed 140 mm Hg. There are 4 stages in hypertension, each of which differs from the next in systolic blood pressure by 20 mm Hg, and in diastolic blood pressure by 10 mm Hg. In more than 95% of patients with hypertension, its cause cannot be identified. This type of hypertension is characterized as primary or essential. Among hypertension with a known etiology - secondary hypertension - kidney diseases occupy a leading place. The frequency of detection of hypertension in kidney diseases depends on the nosological form of renal pathology and the state of renal function. In almost 100% of cases, hypertension syndrome accompanies kidney tumors - reninoma (renin-secreting kidney tumor), hypernephroma and damage to the renal great vessels - renovascular hypertension. In diffuse kidney diseases, hypertension syndrome is most often detected in diseases of the renal glomeruli - primary and secondary glomerulopathies: primary glomerulonephritis, nephritis in systemic diseases (periarteritis nodosa, systemic scleroderma, systemic lupus erythematosus), diabetic nephropathy. The incidence of hypertension in these diseases with preserved renal function ranges from 30 to 85%. In chronic nephritis, the frequency of hypertension is largely determined by the morphological variant of nephritis. Thus, with the highest frequency (85%) AH is detected in membranoproliferative nephritis; in focal segmental glomerulosclerosis, the frequency of AH is 65%; AH is significantly less common in membranous (51%), mesangioproliferative (49%), IgA nephritis (43%) and nephritis with minimal changes (34%) [1]. The incidence of hypertension in diabetic nephropathy is high. According to international statistics, in diabetes mellitus, hypertension develops more often in women (50–64% of cases) and somewhat less frequently in men (30–55%). Much less frequently, hypertension is detected in diseases of the renal tubules and interstitium (renal amyloidosis, interstitial nephritis, drug nephritis, tubulopathies), in which the incidence of hypertension rarely exceeds 20%. As renal function declines, the frequency of hypertension increases sharply, reaching a level of 85-70% in the stage of renal failure, regardless of the nosology of the renal process. The relationship between kidney health and hypertension is complex and forms a vicious circle: the kidneys are both the cause of hypertension and the target organ. So, on the one hand, damage to the kidneys and especially the renal vessels through the mechanisms of sodium retention and activation of pressor systems leads to the development of hypertension. On the other hand, hypertension itself can cause kidney damage and the development of nephroangiosclerosis (primarily shriveled kidney), and hypertension, which develops against the background of existing renal pathology, aggravates kidney damage and accelerates the development of renal failure. This occurs due to disturbances in intrarenal hemodynamics - increased pressure inside the renal capillaries (intraglomerular hypertension) and the development of hyperfiltration. The last two factors (intraglomerular hypertension and hyperfiltration) are currently considered as leading factors in non-immune hemodynamic progression of renal failure [2]. Table 1. Classification of hypertension in people aged 18 years and older
| Blood pressure, mmHg Art. | ||
| CATEGORY | systolic | diastolic |
| Optimal blood pressure | <120 | <80 |
| Normal blood pressure | 120–129 | 80–84 |
| Increased normal blood pressure | 130–139 | 85–89 |
| AH, stage: | ||
| I | 140–159 | 90–99 |
| II | 160–179 | 100–109 |
| III | 180–209 | 110–119 |
| IV | >210 | >120 |
The presented data on the relationship between the condition of the kidneys and hypertension dictate the need for careful monitoring of blood pressure in all patients with chronic kidney disease. Currently, much attention is paid to the tactics of antihypertensive therapy - the rate of reduction in blood pressure and establishing the level of blood pressure to which the initially elevated blood pressure should be reduced. It is considered proven that: – the decrease in blood pressure should be gradual; a one-time maximum reduction in high blood pressure should not exceed 25% of the initial level; – in patients with kidney pathology and hypertension syndrome, antihypertensive therapy should be aimed at complete normalization of blood pressure, even despite a temporary decrease in renal depuration function. This tactic is designed to eliminate systemic hypertension in order to normalize intrarenal hemodynamics and slow down the rate of progression of renal failure. In the treatment of blood pressure in kidney diseases, the general provisions on which the treatment of hypertension in general is based remain important. This is a regime of work and rest; weight loss; increased physical activity; following a diet with limited salt and cholesterol-containing foods; reducing alcohol consumption; withdrawal of medications that cause hypertension. Of particular importance for nephrology patients is strict limitation of sodium intake. Renal sodium retention and an increase in its content in the body are considered one of the main factors in the pathogenesis of hypertension. In kidney diseases, due to impaired sodium transport in the nephron and a decrease in its excretion, this mechanism becomes decisive. Taking this into account, the total daily salt intake (including salt contained in food products) for nephrogenic hypertension should be limited to 5–6 g. Taking into account the content of table salt in food products (bread, sausage, cheese, etc.), the use of pure table salt salt should be limited to 2-3 g per day. Salt restriction should be less stringent in patients with polycystic kidney disease, “salt-wasting” pyelonephritis, and in some cases of chronic renal failure, when, due to damage to the renal tubules, sodium reabsorption in them is impaired and sodium retention in the body is not observed. In these situations, the criteria for determining the patient’s salt regime are daily electrolyte excretion and the volume of circulating blood. In the presence of hypovolemia and/or increased urinary sodium excretion, salt intake should not be limited. A feature of the treatment of hypertension in chronic kidney diseases is the need to combine antihypertensive therapy and pathogenetic therapy of the underlying disease. Agents of pathogenetic therapy for kidney diseases (glucocorticosteroids, heparin, chimes, non-steroidal anti-inflammatory drugs - NSAIDs, sandimmune) themselves can have different effects on blood pressure, and their combinations with antihypertensive drugs can nullify or enhance the hypotensive effect of the latter. Based on many years of our own experience in the treatment of nephrogenic hypertension, we came to the conclusion that in patients with kidney diseases, glucocorticosteroids can enhance nephrogenic hypertension if their administration does not develop a pronounced diuretic and natriuretic effect. As a rule, such a reaction to steroids is observed in patients with initial severe sodium retention and hypervolemia. Therefore, severe hypertension, especially diastolic hypertension, should be considered as a relative contraindication for the prescription of high doses of glucocorticosteroids. NSAIDs - indomethacin, ibuprofen, etc. - are inhibitors of prostaglandin synthesis. Our studies [3] show that NSAIDs can reduce diuresis, natriuresis and increase blood pressure, which limits their use in the treatment of patients with nephrogenic hypertension. Prescribing NSAIDs simultaneously with antihypertensive drugs can either neutralize the effect of the latter or significantly reduce their effectiveness. In contrast to these drugs, heparin has diuretic, natriuretic and hypotensive effects. The drug enhances the hypotensive effect of other drugs. Our experience suggests that the simultaneous administration of heparin and antihypertensive drugs requires caution, as it can lead to a sharp decrease in blood pressure. In these cases, it is advisable to start heparin therapy with a small dose (15,000 - 17,500 units/day) and increase it gradually under the control of blood pressure. In the presence of severe renal failure (glomerular filtration rate less than 35 ml/min), heparin in combination with antihypertensive drugs should be used with great caution [3]. The following requirements are imposed on antihypertensive drugs used for the treatment of nephrogenic hypertension: – the ability to influence the pathogenetic mechanisms of the development of hypertension; – no deterioration in the blood supply to the kidneys and inhibition of renal function; – ability to correct intraglomerular hypertension; – no metabolic disorders and minimal side effects.
Table 2. Daily doses of ACE inhibitors
| A drug | Dose, mg/day | Number of appointments per day |
| Captopril (capoten) | 25–75 (150) | 3–4 |
| Enalapril (Renitec) | 5–20 (40) | 1–2 |
| Ramipril (tritace) | 2,5–10 (10) | 1–2 |
| Peridopril (Prestarium) | 2–4 (8) | 1–2 |
| Lisinopril (sinopril) | 10–40 (80) | 1–2 |
| Cilazapril (inhibase) | 2,5–10 (10) | 1–2 |
| Trandolapril (Hopten) | 2–4 | 1–2 |
Antihypertensive (hypotensive) drugs
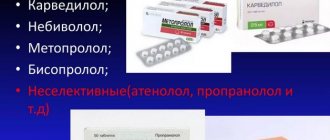
Currently, 5 classes of antihypertensive drugs are used to treat patients with nephrogenic hypertension: – angiotensin-converting enzyme inhibitors (ACEIs); – calcium antagonists; – beta blockers; – diuretics; - alpha blockers. Drugs with a central mechanism of action (rauwolfia drugs, clonidine) have an auxiliary value and are currently used only for narrow indications. First choice drugs include ACEIs and calcium channel blockers (calcium antagonists). These two groups of drugs meet all the requirements for antihypertensive drugs intended for the treatment of nephrogenic hypertension, and, most importantly, simultaneously have nephroprotective properties. In this regard, this article will focus on these two groups of drugs.
IACF
The basis of the pharmacological action of all ACE inhibitors is the inhibition of ACE (aka kininase II). The physiological effect of ACP is twofold. On the one hand, it converts angiotensin I into angiotensin II, which is one of the most powerful vasoconstrictors. On the other hand, being kininase II, it destroys kinins - tissue vasodilator hormones. Accordingly, pharmacological inhibition of this enzyme blocks the systemic and organ synthesis of angiotensin II and leads to the accumulation of kinins in the circulation and tissues. Clinically, this is manifested by a pronounced hypotensive effect, which is based on a decrease in total and locally renal peripheral resistance, and correction of intraglomerular hemodynamics, which is based on the expansion of the efferent renal arteriole, the main site of application of local renal angiotensin II [4]. In recent years, the renoprotective role of ACE inhibitors has been actively discussed, which is associated with the elimination of the effect of angiotensin, which determines the rapid sclerosis of the kidneys, i.e. with blockade of proliferation of mesangial cells, their production of collagen and epidermal growth factor of the renal tubules. Depending on the time of elimination from the body, the first generation ACE inhibitors are distinguished (captopril with a half-life of less than 2 hours and the duration of the hemodynamic effect of 4–5 hours) and the second generation ACEI with a half-life of the drug of 11–14 hours and the duration of the hemodynamic effect of more than 24 hours. To maintain The optimal concentration of drugs in the blood during the day requires 3-4 doses of captopril and a single or double dose of other ACE inhibitors. In table Table 2 shows the most common ACE inhibitors with their dosages. Elimination of captopril and enalapril is carried out only by the kidneys, ramipril - 60% by the kidneys and 40% by the extrarenal route. In this regard, with the development of chronic renal failure, the dose of drugs should be reduced, and if the glomerular filtration rate (GFR) is less than 30 ml/min, it should be halved. The hypotensive effect of IACF develops quickly (within 24 hours), however, several weeks of continuous use of the drugs are required for the development of the full therapeutic effect.
Effect of ACEI on the kidney
In nephrological patients with hypertension with initially preserved renal function, ACE inhibitors with long-term use (months, years) increase renal blood flow, do not change or slightly reduce the level of blood creatinine, increasing GFR. In the first week of treatment, there may be a slight increase in the level of creatinine and K in the blood, which returns to normal on its own over the next few days without stopping the medication. A risk factor for a stable decline in renal function and an increase in K concentration in the blood is the elderly and senile age of patients. The dose of ACE inhibitors in this age group should be reduced. ACEI therapy in patients with renal failure requires special attention. In the vast majority of patients, long-term ACEI therapy, corrected for the degree of renal failure, had a beneficial effect on renal function: creatininemia decreased, GFR increased, serum K levels remained stable, and the development of end-stage renal failure slowed down. However, an increase in the level of creatinine and K in the blood that persists for 10-14 days from the start of IACI therapy is an indication for discontinuation of the drug. ACE inhibitors have the ability to correct intrarenal hemodynamics, reducing intrarenal hypertension and hyperfiltration. In our observations, correction of intrarenal hemodynamics under the influence of ACE inhibitors (Capoten, Renitek, Tritace) was achieved in 77% of patients. The vast majority of ACEIs have pronounced antiproteinuric properties. The maximum antiproteinuric effect develops against the background of a low-salt diet. Increased consumption of table salt inhibits the proteinuric effect of IACF.
Complications and side effects observed when taking IACF
ACEIs are a relatively safe group of drugs that cause a small number of adverse reactions. The most common complications are cough and hypotension. Cough can occur at different stages of drug treatment - both at the earliest and after 20-24 months from the start of therapy. The mechanism of cough is associated with the activation of kinins and prostaglandins. The basis for discontinuing medications when a cough appears is a significant deterioration in the patient’s quality of life. After stopping the medications, the cough goes away within a few days. A more severe complication of IACF therapy is the development of hypotension. The risk of hypotension is high in patients with congestive heart failure, especially in old age, with malignant high-renin hypertension, and with renovascular hypertension. It is important for the clinician to be able to predict the development of hypotension during the use of IACF. For this purpose, the hypotensive effect of the first small dose of the drug is assessed (12.5 - 25 mg Capoten, 2.5 mg Renitec, 1.25 mg Tritace). A pronounced hypotensive reaction to this dose may be a precursor to the development of hypotension during long-term drug treatment. In the absence of a pronounced hypotensive reaction, the risk of developing hypotension with further treatment is significantly reduced. Quite common complications of IACF treatment are headache and dizziness. These complications, as a rule, do not require discontinuation of medications. Allergic reactions - angioedema, urticaria - are not observed so often. Neutropenia and agranulocytosis can develop when using high doses of captopril in patients with systemic diseases (systemic lupus erythematosus, systemic scleroderma, etc.) and require discontinuation of the drug. Typically, the white blood cell count recovers within a month after discontinuation of the drug. In nephrological practice, the use of IACF is contraindicated in the following cases: – the presence of renal artery stenosis of both kidneys; – the presence of renal artery stenosis of a single kidney (including a transplanted one); – combination of renal pathology with severe heart failure; – chronic renal failure (CRF), long-term treatment with diuretics. The appointment of an ACE inhibitor in these cases may be complicated by an increase in the level of creatinine in the blood, a decrease in glomerular filtration, and even the development of acute renal failure. ACE inhibitors are not indicated during pregnancy, since their use in the second and third trimesters can lead to fetal hypotension and malnutrition. In elderly and senile patients, ACE inhibitors should be used with caution due to the risk of hypotension and decreased renal function. Impaired liver function creates complications during drug treatment due to deterioration in the metabolism of inhibitors in the liver.
Calcium antagonists
The mechanism of the hypotensive action of calcium antagonists (CA) is associated with the dilation of arterioles and a decrease in increased total peripheral vascular resistance (TPR) due to inhibition of the entry of Ca2+ ions into the cell. The ability of drugs to block the vasoconstrictor hormone, endothelin, has also been proven. According to the modern classification of AKs, there are three groups of drugs: papaverine derivatives - verapamil, tiapamil; dihydropyridine derivatives – nifedipine, nitrendipine, nisoldipine, nimodipine; benzothiazepine derivatives - diltiazem. They are called prototype drugs, or first generation AKs. In terms of hypotensive activity, all three groups of prototype drugs are equivalent, i.e. the effect of nifedipine at a dose of 30-60 mg/day is comparable to that of verapamil at a dose of 240-480 mg/day and diltiazem at a dose of 240-360 mg/day. In the 80s, AK II generation appeared. Their main advantages are a long duration of action (12 hours or more), good tolerability and tissue specificity. Among the second generation AKs, the most widely used are slow-release verapamil and nifedipine, known as verapamil SR (isoptin SR) and nifedipine GITS); nifedipine derivatives - isradipine (Lomir), amlodipine (Norvasc), nitrendipine (bayotensin); diltiazem derivatives - klentiazem. In clinical practice and in nephrology in particular, short-acting drugs are less preferable because they have unfavorable pharmacodynamic properties. Nifedipine (Corinfar) has a short period of action (4 - 6 hours), the half-life ranges from 1.5 to 5 hours. For a short time, the concentration of nifedipine in the blood varies over a wide range - from 65 - 100 to 5 - 10 ng/ml . A poor pharmacokinetic profile with a peak increase in drug concentration in the blood, entailing a short-term decrease in blood pressure and a number of neurohumoral reactions, such as the release of catecholamines, activation of the RAS and other stress hormones, determines the presence of the main adverse reactions when taking drugs - tachycardia, arrhythmias exacerbation of angina, facial flushing and other symptoms of hypercatecholaminemia, which are unfavorable for the function of both the heart and kidneys. Long-acting and continuous-release nifedipines (GITS form) provide a constant concentration of the drug in the blood for a long time, due to which they are devoid of the above undesirable properties and can be recommended for the treatment of nephrogenic hypertension. Drugs of the verapamil and diltiazem group do not have the disadvantages of short-acting dihydropyridines. In terms of hypotensive activity, AKs represent a group of highly effective drugs. The advantages over other antihypertensive drugs are their pronounced antilipidemic (the drugs do not affect the lipoprotein spectrum of the blood) and antiaggregation properties. These qualities make them the drugs of choice for treating older people.
Action of AK on the kidneys
AA have a beneficial effect on renal function: they increase renal blood flow and cause natriuresis. The effect of drugs on GFR and intrarenal hypertension is less clear. There is evidence that verapamil and diltiazem reduce intraglomerular hypertension, while nifedipine either has no effect on it or increases intraglomerular pressure. In this regard, for the treatment of nephrogenic hypertension, among drugs from the AK group, preference is given to verapamil and diltiazem and their derivatives [5]. All AKs have nephroprotective properties, which are determined by the ability of the drugs to reduce renal hypertrophy, inhibit metabolism and mesangial proliferation, and thereby slow the rate of progression of renal failure.
Complications and adverse reactions observed when taking AK
Side effects are usually associated with taking short-acting dihydropyridine group AKs and include tachycardia, headache, facial flushing, swelling of the ankle and feet. Swelling of the legs and feet decreases with a decrease in the dose of drugs, by limiting the patient’s physical activity and by prescribing diuretics. Due to its cardiodepressive effect, verapamil can cause bradycardia, atrioventricular block and, in rare cases (when using large doses), atrioventricular dissociation. Constipation often occurs when taking verapamil. Although AA do not cause negative metabolic effects, the safety of their use in early pregnancy has not yet been established. Taking AK is contraindicated in case of initial hypotension, sick sinus syndrome. Verapamil is contraindicated in cases of atrioventricular conduction disorders, sick sinus syndrome, and severe heart failure.
Treatment of hypertension in the stage of chronic renal failure
The development of severe chronic renal failure (GFR 30 ml/min or lower) requires adjustments in the treatment of hypertension. With chronic renal failure, as a rule, complex therapy for hypertension is necessary, including limiting salt in the diet without limiting fluids, removing excess sodium with the help of saluretics and the use of effective antihypertensive drugs and their combinations. Of the diuretics, the most effective are loop diuretics - furosemide and ethacrynic acid, the dose of which can be increased to 300 and 150 mg per day, respectively. Both drugs slightly increase GFR and significantly increase K excretion. They are usually prescribed in tablets, and in urgent conditions (pulmonary edema) they are administered intravenously. When using large doses, be aware of the possibility of ototoxicity. Due to the fact that hyperkalemia often develops simultaneously with sodium retention in chronic renal failure, potassium-sparing diuretics are rarely used and with great caution. Thiazide diuretics (hypothiazide, cyclometazide, oxodoline, etc.) are contraindicated in chronic renal failure. AK is one of the main groups of antihypertensive drugs used for chronic renal failure. The drugs have a beneficial effect on renal blood flow, do not cause sodium retention, do not activate the RAS, and do not affect lipid metabolism. A combination of drugs with beta blockers, centrally acting sympatholytics (for example: Corinfar + anaprilin + dopegit, etc.) is often used. In case of severe, treatment-refractory and malignant hypertension in patients with chronic renal failure, an inhibitory agent (Capoten, Renitek, Tritace, etc.) is prescribed in combination with saluretics and beta-blockers, but the dose of the drug should be reduced taking into account the decrease in its secretion as chronic renal failure progresses. Constant monitoring of GFR, the level of azotemia and K in the blood serum is necessary, since with the predominance of the renovascular mechanism of hypertension, glomerular filtration pressure and GFR can sharply decrease. If drug therapy is ineffective, extracorporeal removal of excess sodium is indicated: isolated ultrafiltration, hemodialysis (HD), hemofiltration. In the terminal stage of chronic renal failure after transfer to program HD, treatment of volume-dependent hypertension consists of maintaining an adequate HD and ultrafiltration regimen and an appropriate water-salt regimen in the interdialytic period to maintain the so-called “dry mass”. If additional antihypertensive treatment is necessary, antihypertensive agents or sympatholytics are used. In cases of severe hyperkinetic syndrome, in addition to the treatment of anemia and surgical correction of arteriovenous fistula, the use of beta blockers in small doses is useful. At the same time, since the pharmacokinetics of beta-blockers in chronic renal failure is not affected, and large doses suppress renin secretion, these same drugs are also used in the treatment of renin-dependent hypertension in combination with vasodilators and sympatholytics [6]. In case of hypertension not controlled by HD, combinations of several antihypertensive drugs are often more effective, for example: beta blocker + alpha blocker + AC and especially ACEI, and it must be taken into account that captopril is actively eliminated during the HD procedure (up to 40% in 4 - hourly GD). In the absence of the effect of antihypertensive therapy, when preparing a patient for a kidney transplant, they resort to bilateral nephrectomy to convert renin-dependent uncontrolled hypertension into a renoprivative volume-sodium-dependent controlled form. In the treatment of hypertension that develops again in patients on HD and after kidney transplantation (KT), it is important to identify and eliminate the causes: dose adjustment of medications that contribute to hypertension (erythropoietin, corticosteroids, sandimmune), surgical treatment of graft artery stenosis, resection of the parathyroid glands, tumors and etc. In the pharmacotherapy of hypertension after LT, AA and ACE inhibitors are primarily used, and diuretics are prescribed with caution, since they enhance lipid metabolism disorders and can contribute to the formation of atherosclerosis, which is responsible for a number of complications after LT [7]. In conclusion, it can be stated that at the present stage there are great opportunities for the treatment of nephrogenic hypertension at all its stages: with preserved renal function, at the stage of chronic and end-stage renal failure, during treatment with programmatic HD and after LT. The choice of antihypertensive drugs should be based on a clear understanding of the mechanisms of hypertension development and clarification of the leading mechanism in each specific case.
Literature:
1. Ritz E., Rambausek M., Hasslacher C., Mann J. Pathogenesis of hypertension in glomerular disease. Amer J Nephrol 1989;9(suppl.A):85-90. 2. Brenner BM. Hemodynamically mediated glomerular injury and progressive nature of kidney disease. Kidney Int 1983;23:647-55. 3. Tareeva I.E., Kutyrina I.M. Treatment of nephrogenic hypertension Clinical medicine, 1985;N 6:20-7. 4. Ichikawa J., Brenner BM Glomerular actions of angiotensin II. Amer J Med 1984;76:43-9. 5. Sunderrajan S., Reams G., Bauer J. Long-term renal effects of diltiazem in essential hypertension. Amer Heart J 1987;114:383-8. 6. Ermolenko V.M. Chronic hemodialysis. M: Medicine, 1982. p. 53-88. 7. Curtis JJ Management of hypertension after transplantation. Kidney Int 1993;44: (suppl. 43): S45-S49.
Pathophysiological mechanisms of high blood pressure in CKD
The relationship between arterial hypertension and renal pathology always develops in two directions. It is known that patients with CKD are most often people with high-risk hypertension phenotypes (we are talking about resistant forms, “nocturnal” hypertension and its latent course). If hypertension occurs latently, target organs are affected. Thanks to recent research, a number of patterns have been identified. For example, if hypertension has a latent course, this is usually associated with:
- with a high risk of left ventricular hypertrophy;
- with the appearance of proteinuria;
- with a decrease in GFR.
In addition, latent forms of arterial hypertension are always associated with:
- with diseases of the heart and blood vessels;
- with chronic kidney failure in the terminal stage;
- with any cause of death.
In any case, latent hypertension must continue to be carefully studied, with the constant introduction of rational diagnostic and therapeutic methods.
It is customary to talk about resistant arterial hypertension in cases where, when prescribing at least three antihypertensive drugs (subject to optimal dosage), the pressure remains at the same high level and the target level cannot be achieved during therapy.
As for the pathophysiological mechanisms of the development of arterial hypertension in CKD, it is complex and has many predisposing factors, in particular:
- sodium retention in the body;
- increased intracellular volume;
- intensive work of the parasympathetic nervous system;
- intensive operation of the RAA system;
- endothelial dysfunction.
Recently, researchers have been providing a lot of information about the homeostasis and regulation processes of water and sodium in the body. No less relevant is the discussion of multi-organ effects that cause:
- limiting water consumption;
- prescribing a diet with a high salt content;
- drug vasopressin;
- level of sodium accumulation;
- excretion of sodium by the kidneys.
It has been proven that the kidneys and cardiovascular system are negatively affected by impaired sodium and water metabolism. If the body reacts poorly to a high-salt diet, it is most often associated with an increase in the incidence of both hypertension and chronic kidney disease. Prescription of drugs containing erythropoietin is also associated with both hypertension and CKD. Research shows the multifactorial mechanisms of this connection. For example, there are patients with CKD who cannot quickly adapt to the fact that the red blood cell volume becomes higher due to:
- decreased glomerular filtration rate;
- strong vascular resistance;
- hypertrophy of the left ventricle of the heart.
When using EPA, physicians should be extremely careful, regularly monitoring the rate at which hemoglobin levels in the blood increase (in this case, it can be difficult to control blood pressure).
Arterial hypertension in patients on dialysis occurs due to a number of reasons:
- high volume of fluid in the body;
- increase in sympathetic hyperactivity;
- intensity of operation of the RAA system;
- atherosclerotic changes, etc.
In chronic kidney disease, uremic toxins constantly accumulate in the intestine, negatively affecting its microflora, as well as metabolic processes. Once in the blood, endotoxins aggravate the inflammatory process and damage the kidney structure, which, unfortunately, worsens the prognosis of the disease.
What happens to the body when there is excess uric acid
21.09.2021
You've probably heard many times about hyperuricemia - excess uric acid in the blood . But do you know what exactly we are talking about ? Why does this condition occur? And how does this threaten health?
Elevated uric acid levels: causes, symptoms and treatment
Uric acid is a substance that our body produces through its own metabolism. Although a small part of it is formed during the breakdown of purine, a type of protein present in the food we eat. The more protein we eat, the more uric acid the body produces. Uric acid usually does not cause any health problems if it is functionally eliminated by the kidneys . The problem occurs when its level increases. That is, when the body produces too much uric acid or does not remove it properly.
In this case, hard crystals form and settle on the joints , causing severe pain.
The main reasons for the increased MC content:
- Excessive production of uric acid by the body itself
- Problems with excretion through the kidneys
- Inadequate diet with excess protein-rich foods
- Consumption of alcohol and other substances harmful to health
In addition, there are several risk factors that increase the likelihood of the disease:
- Regular consumption of large amounts of caffeine
- Chronic alcohol consumption
- Family history of gout
- Stressful situations
- Male
- Hypertension , diabetes , obesity and high cholesterol
High UA levels may not cause symptoms. Although one of the main consequences of this problem is the appearance of gout, due to the accumulation of acid crystals, they are deposited in the joints .
Other symptoms:
- Pain, swelling and redness of the joints
- Difficulty in joint movement, especially in the fingers, knees , ankles, heels and toes
- Deformities appear in severely affected joints
- kidney stones - causes lower back and difficulty urinating
Treatment is aimed at bringing uric acid to normal levels. It is based on diet : minimizing or eliminating foods high in purine and consuming plenty of water that is low in minerals. To relieve pain caused by joint , you can take ibuprofen or non-steroidal anti-inflammatory medications. Doctors often prescribe medications that block the absorption of urate.
As for the prevention of gout, xanthine oxidase inhibitors are used. joint pain occurs , as the condition may worsen. It is very important to follow a diet to reduce sUA levels.
Here are some of the products to look out for:
• Artichoke • Onion • Celery • Pumpkin • Carrots • Cereals • Apples • Strawberries • Citrus fruits • Blueberries • Chicken • Eggs • Low mineralization water
And these are the products that are prohibited:
• Red meat • Shellfish • Red fish • Spinach • Mushrooms • Cauliflower • Asparagus • Ice cream • Butter • Industrial baked goods • Alcoholic drinks • Carbonated drinks
To avoid increasing the level of MK, you need to follow some tips:
- If you have risk factors, see your doctor once a year to monitor your condition.
- Drink anti-inflammatory and diuretic infusions twice a week. Chamomile and horsetail are recommended.
- Drink at least two liters of water per day.
- Don't eat a lot or too often of seafood or red meat.
This article is for informational purposes only. Do not self-medicate and discuss any advice with your doctor .
Published in Laboratory research Premium Clinic
Blood pressure control and its targets
Despite the high level of awareness of patients with CKD about hypertension, it is not always possible to control blood pressure. For diagnostic purposes, blood pressure is most often measured either randomly or in an outpatient setting. Thanks to ambulatory blood pressure measurement, it is possible to further evaluate its variability during the day. Unfortunately, not all patients with CKD regularly monitor their blood pressure; therefore, from 30 to 60% of patients cannot achieve its target values. It is their target organs that may be damaged in the future.
Thus, regular blood pressure monitoring ensures:
- reducing the risk of complications from the heart and blood vessels;
- reduced risk of cerebral complications;
- reduction in mortality rate;
- prevention of irreversible processes associated with kidney failure.
The optimal blood pressure values for people suffering from chronic kidney disease still remain controversial among specialists, despite the fact that clinical studies have already made it possible to give specific and clear recommendations:
- upper “digits” of blood pressure - 140/90 (albuminuria - less than 30 g daily);
- 130/80 (albuminuria - more than 30 mg daily).
For patients with CKD and a high level of cardiovascular risk, the optimal target blood pressure for them is 130/80.