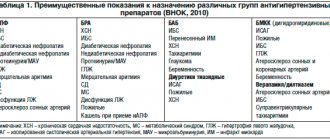
For long-term treatment of hypertension, five main groups of drugs are currently recommended. We have already talked about two of them - ACE inhibitors and angiotensin II receptor antagonists that affect the renin-angiotensin-aldosterone system (RAAS). In this article, we will describe three more groups of antihypertensive drugs and tell you what to pay attention to when servicing prescriptions for these drugs, and what he should warn the buyer about. So today the focus is on diuretics, beta blockers and calcium channel blockers.
Diuretics
Maintaining water-salt balance in the body is the most important condition for maintaining stable blood pressure levels. Renal nephrons regulate fluid volume and electrolyte content in the body through secretion and reabsorption. The water-salt balance can be disturbed in a number of conditions, including hypertension, heart or kidney failure, as well as nephrotic syndrome, cirrhosis, etc.
Diuretics can normalize water-salt balance by increasing the rate of urine flow and excretion of Na+ and the accompanying anion, usually Cl-. The major determinant of extracellular fluid volume in the body is NaCl, and most diuretics reduce extracellular fluid volume by reducing total body NaCl [1].
Today, both thiazide and thiazide-like diuretics and loop diuretics are used to treat arterial hypertension.
Thiazide and thiazide-like diuretics
Mechanism of action
Thiazide and thiazide-like diuretics act mainly in the cortical segment of the nephron loop, at the site of inhibition of the reabsorption of cations (potassium, sodium, magnesium). They block the transport protein that ensures the transfer of sodium and chlorine into tubular epithelial cells, as a result of which the excretion of these electrolytes in the urine increases. The excretion of calcium ions, on the contrary, decreases [2]. This is accompanied by increased diuresis and a decrease in circulating blood volume [3].
In elderly patients, thiazide and thiazide-like drugs are more effective than β-blockers and ACE inhibitors [3].
Even in low doses, they have fairly high antihypertensive activity, which is not inferior to the effect of calcium antagonists and α1-adrenergic blockers [4].
According to research, with regular use of thiazide and thiazide-like diuretics, systolic blood pressure (BP) decreases by an average of 10–20 mmHg. Art., and diastolic - by 5–15 mm Hg. Art. In addition, drugs of this group reduce peripheral vascular tone [2].
Indications and properties
Drugs in this group are used both as monotherapy and in combination with other antihypertensive drugs for arterial hypertension. In addition, they are prescribed for chronic heart failure, renal dysfunction, premenstrual syndrome (to reduce swelling associated with PMS).
Thiazides and thiazide-like diuretics, like most other classes of modern antihypertensive drugs, exhibit a complex cardiovascular effect [3]:
- reduce blood pressure;
- prevent the development of cardiovascular complications;
- reduce cardiovascular mortality.
The effect on cardiovascular risks is due to the ability of drugs in this group to reverse the development of left ventricular hypertrophy. Another positive property is that they increase the effectiveness of antihypertensive drugs of the other four pharmacological groups.
When taking some drugs of this group, the level of uric acid increases, and slightly - glucose and atherogenic lipids [2].
Individual representatives
- Hydrochlorothiazide is one of the most studied and popular diuretics used to treat hypertension. Efficacy and a high safety profile have been proven in long-term randomized studies, so this diuretic is one of the drugs of choice for long-term treatment of hypertension [4].
- Indapamide, unlike other thiazide (and thiazide-like) diuretics, blocks calcium channels in the muscular wall of the arteries, reducing peripheral vascular resistance and exerting a direct vasodilator effect [2, 5]. Indapamide has proven significant organoprotective effects - regression of left ventricular hypertrophy, kidney protection. Hypothiazide is significantly superior in its effect on systolic blood pressure [5]. In addition, the drug does not affect glucose levels and is suitable for use in diabetes mellitus [2].
Portability
Thiazides and thiazide-like diuretics in low doses are well tolerated and do not cause significant changes in carbohydrate and lipid metabolism. Rarely, usually in men, gout may develop while taking medications [4]. In addition, thiazide diuretics have an adverse effect on erectile function.
What should I warn the client about?
- During treatment, electrolyte balance may be disturbed, therefore, if you experience dry mouth, thirst, heart rhythm disturbances, or unusual fatigue during treatment, you should contact your doctor as soon as possible [6].
- When taken together with alcohol, orthostatic hypotension may occur (a sharp decrease in pressure when changing body position from horizontal to vertical) [6].
- At the beginning of treatment with drugs of this group, it is not recommended to drive a car or perform work that requires increased attention. The duration of this period is individual [6].
- Thiazide and thiazide-like diuretics may contribute to the development of erectile dysfunction. If a client purchases drugs from this group (including as part of combination drugs) and PDE-5 inhibitors, it is appropriate to warn him about the possible negative impact of the former on sexual function.
Thiazide diuretics in the treatment of arterial hypertension
Chlorothiazide, the first thiazide diuretic effective when taken orally, was created in 1956. In 1957, hydrochlorothiazide (HCT) was synthesized, which replaced chlorothiazide from clinical practice due to its higher effectiveness. In 1959, the thiazide-like diuretic chlorthalidone appeared, and indapamide in 1974. The most frequently used and, therefore, the most studied diuretics in clinical trials are chlorthalidone, HCTZ and indapamide (including indapamide retard form). In our country, the most popular diuretics are HCTZ and indapamide (indapamide retard). However, despite the recognition of the clinical value of this class of drugs, in recent years their leading position has been questioned, and this was primarily due to the discussion of their metabolic effects, with the results of the ACCOMPLISH study [7] and a new meta-analysis of the antihypertensive effects of HCTZ [8]. Metabolic effects of diuretics: myths and reality Negative metabolic effects on carbohydrate, lipid and purine metabolism, and electrolyte disturbances are used as arguments against the priority use of TDs as first-choice drugs. The most significant debate has developed in recent years around the “diabetogenic” effects of TD. A drug is considered a significant factor in the manifestation of diabetes mellitus (DM) if, firstly, the number of patients who developed diabetes mellitus while using this drug is greater than with the natural course of hypertension, and, secondly, the development of diabetes mellitus during therapy is accompanied by a worsening of clinical symptoms. outcomes. Available data allow discussion of differences between the main classes of drugs in relation to the development of new cases of diabetes. However, the significance of the existing evidence to date should be considered limited, primarily due to the fact that in none of the completed large controlled studies, the development of new diabetes was not the primary endpoint. An analysis of 27 randomized controlled trials involving 158,709 patients (of which 33,395 with diabetes), comparing the effect of the “old” and “new” antihypertensive therapy regimens on cardiovascular events and mortality in patients with hypertension depending on the presence of diabetes, did not reveal differences in reducing the risk of major cardiovascular events in patients with or without diabetes during therapy based on ACE inhibitors, AK, ARB II and TD/BB. Tighter BP control was accompanied by a significant reduction in major cardiovascular events in patients with diabetes compared with patients without diabetes [9]. Consequently, all modern classes of antihypertensive drugs, including TDs, can be used in the treatment of hypertension. In the ARIC cohort study (Atherosclerotic Risk in Community cohort, n=13877) - one of the most methodologically high-quality observations - when analyzing the subgroup with hypertension (3804 people), TD therapy compared with untreated patients was not accompanied by an increase in the incidence of diabetes (RR 0.91 , 95% CI 0.73–1.13), which was not significantly different from data for ACE inhibitors (RR 0.98, 95% CI 0.72–1.34) or OCs (RR 1.17, 95% CI 0.83–1.66) [10]. Only BB therapy led to a significant increase in new cases of diabetes (RR 1.28, 95% CI 1.04–1.57; p<0.05). In the EWPHE, STOP-Hypertension-2, INSIGHT, ALLHAT, LIFE, ASCOT-BPLA studies, a higher incidence of diabetes was indeed observed in the groups where TD was prescribed [11–16]. However, EWPHE, STOP-Hypertension-2, INSIGHT and ALLHAT did not reveal any advantages of other drugs over TD in terms of outcomes [12,13,14,16]. The LIFE study [15] found differences in the primary endpoint, and the ASCOT-BPLA study [11] found differences in secondary cardiovascular outcomes, but it should be remembered that in the latter two studies, TDs were not the main drugs. It seems important to note significant methodological differences when identifying new cases of diabetes. For example, in the EWPHE study, the assessment of new cases of diabetes was based on physician reports [12]. In summary, none of the completed studies considered new cases of diabetes as a primary endpoint. Inconsistent results regarding new cases of diabetes may be due to differences in study design and duration, sample sizes, comparison groups, patient populations, laboratory techniques, drugs, and dosages used. Data obtained from comparing two treatment regimens may equally reflect both the positive effect of one drug and the negative effect of the other. Despite the potentially negative effects of TD on glucose metabolism, therapy with this class of drugs leads to a decrease in cardiovascular morbidity and mortality in patients with hypertension. Any possible negative metabolic effects of TD therapy are offset by positive effects on other cardiovascular endpoints and overall mortality. Treatment with relatively high doses of TD during the first year may be accompanied by an increase in the level of total cholesterol and LDL cholesterol by 5–7% without a significant effect on HDL cholesterol; none of the long-term studies revealed an increase in the level of serum cholesterol during TD therapy compared with placebo [17]. The effectiveness of TD in relation to the incidence of strokes, coronary artery disease, and cardiovascular diseases did not depend on the initial cholesterol level in the SHEP study [18]. The adverse effects of TD on lipid metabolism are dose-dependent. At the present stage, HCTZ is used in low doses that are safe from the point of view of its effect on lipid metabolism, and indapamide retard has minimal effect on glucose and lipid metabolism. The effect of long-term TD therapy on cholesterol levels is minimal and may have limited clinical significance. Patients can receive TD regardless of baseline lipid levels, especially given the option of statin therapy. The risk of developing electrolyte disturbances (primarily hypokalemia) is determined by the initial potassium content in the body, the level of salt consumption during treatment, and the doses of diuretics. For a modern dose of HCTZ 12.5–25 mg/day. effects on serum potassium levels are minimal. To prevent hypokalemia induced by diuretics, it is recommended to use minimal doses of diuretics (HCTZ 12.5–25 mg/day, indapamide retard 1.5 mg/day), reducing sodium intake to 2.5 mg/day, increasing intake potassium, the use of diuretics as part of combination therapy. The development of hypokalemia when low doses of diuretics are prescribed is a factor requiring the exclusion of primary hyperaldosteronism [17]. An increase in the level of uric acid in the blood serum, associated with increased reabsorption in the proximal tubules, is also a dose-dependent effect of TD therapy [17]. One of the beneficial metabolic effects of TD that is largely undiscussed is its ability to increase bone density. Treatment with HCTZ is accompanied by an increase in calcium resorption by the renal tubules, a decrease in the activity of total and bone-specific alkaline phosphatase, and a beneficial effect on markers of bone formation (N-telopeptide and osteocalcin). Several RCTs have assessed whether HCTZ improves bone density and have explored possible mechanisms that might explain these effects [19–22]. For example, a randomized, double-blind, two-year study compared HCTZ 50 mg/day. versus placebo in 138 healthy postmenopausal women [19]. Significant effects were found in the active therapy group on the total bone density of the lower leg and forearm, with no effect on the spine or femoral neck. TDs were able to prevent fractures, which is especially important in elderly patients with osteoporosis (not a separate indication, but is considered as an additional positive metabolic effect). According to a cohort study of 7891 patients over 55 years of age (mean age 68.9 years), TD therapy for one year was associated with a statistically significant reduction in the risk of hip fractures (RR 0.46, 95% CI 0.21–0.96) according to compared with persons not receiving diuretic treatment. However, 4 months after cessation of TD therapy, the risk of fractures was similar to that before treatment [21]. Thus, adverse metabolic effects are minimal when diuretics are used in low doses and do not lead to undesirable clinical consequences, and the ability of TD to influence bone density and reduce the risk of osteoporosis deserves attention in a number of clinical situations. Have the results of the ACCOMPLISH trial changed the place of diuretics in the treatment of hypertension? The main result of the ACCOMPLISH study (Avoiding Cardiovascular Events in Combination therapy in Patients Living with Systolic Hypertension) [7] was a significant 20% reduction in the relative risk of cardiovascular morbidity and mortality (primary combined endpoint) in the group of patients with high-risk hypertension (n= 11506) receiving benazepril/amlodipine compared with those receiving benazepril/hydrochlorothiazide at 36 months. observations. To date, this is the only study to compare outcomes between two fixed combinations of antihypertensive drugs. Anticipating the main question in connection with the ACCOMPLISH results, whether the combination of an ACEI with a calcium antagonist should replace the combination of an ACEI with a thiazide diuretic, the authors emphasized that “the results of the study should not cast doubt on the ability of diuretics to reduce the risk of cardiovascular events in patients with hypertension” [7]. . To explain the results obtained, the characteristics of the observation group, the characteristics of the end point, the choice of diuretic, and the dose of amlodipine and hydrochlorothiazide were discussed. The observation group turned out to be a population with indications for the prescription of a calcium antagonist and relative contraindications for the prescription of a thiazide diuretic [3–5]: the average age of the patients was 68 years, 60% of them had a history of diabetes mellitus, 50% had obesity, 36% had coronary revascularization , 23% – myocardial infarction, 11% – history of unstable angina (patients with asymptomatic systolic dysfunction were not included). Thus, the ACCOMPLISH population was not representative and, therefore, its results cannot be extrapolated to all patients with hypertension. In addition, the tolerability of therapy with a combination that included HCTZ was better than that with a combination using amlodipine. The primary composite endpoint did not include hospitalization for heart failure (an event for which calcium antagonists are known to be inferior to other drugs, including thiazide diuretics)23,24, but did include coronary revascularization (usually a component of the secondary endpoint). . Moreover, revascularization accounted for more than 40% of events recorded as the primary endpoint. Thus, a number of features of the observation population and primary endpoint largely explain the differences observed. Another reason discussed was the choice of diuretic, with the assumption that HCTZ is less effective than chlorthalidone in reducing the risk of cardiovascular events. Hydrochlorothiazide and chlorthalidone differ in their pharmacokinetic characteristics. HCTZ begins to act 2 hours after administration, the peak of its effect occurs after 4–6 hours. With a single dose, the duration of action is about 12 hours. With long-term use, the duration of the antihypertensive effect increases and reaches 24 hours. Knowledge of the pharmacokinetics of HCTZ can protect you from a common mistake – premature change of treatment tactics. Unlike HCTZ, the peak effect of chlorthalidone occurs after 6 hours. Moreover, the drug has a very long half-life - about 42 hours. This is due to the fact that chlorthalidone accumulates in red blood cells and is slowly released from them into the plasma, providing a long-lasting therapeutic effect. The fact that the pharmacokinetic characteristics of HCTZ did not affect blood pressure control in the ACCOMPLISH study is evidenced by the results of a substudy using ABPM, which confirmed the comparability of blood pressure control [25]. A meta-analysis specifically comparing the results of studies using chlorthaladione or other TDs, including HCTZ (5 studies, 2 of which used chlorthalidone), did not reveal significant differences in the effect of chlorthaladione and other TDs on clinical outcomes [26]. . Therefore, there is currently no strong evidence to support the use of chlorthalidone instead of HCTZ. Available evidence suggests that one of these two drugs should be used to treat hypertension. The question of the advantages of one drug over another can only be resolved in a study with a direct comparison of them. The effectiveness of HCTZ was also criticized by a meta-analysis of studies that compared the antihypertensive effects of HCTZ with other drugs, with the conclusion that HCTZ is a “weak drug”, which is effective in modern doses of 12.5–25 mg/day. “has not been proven in any randomized controlled trial” and that it “should be excluded from first-line antihypertensive treatment” [8]. It should be noted that this meta-analysis included studies in which HCTZ in daily doses of 12.5 and 25 mg was used as monotherapy. Meta-analysis, as a methodological approach, has a number of known limitations, and in terms of its evidentiary power it is significantly inferior to double-blind randomized studies. A double-blind, randomized trial of indapamide retard, amlodipine, or hydrochlorothiazide (Hypothiazide) in elderly patients showed similar efficacy of the treatment regimens [27] (Fig. 1). From the point of view of modern recommendations on hypertension, it is obvious that it is not relevant to consider diuretic monotherapy as a strategy of preferential choice. The common position of all modern recommendations on hypertension is the emphasis on combination antihypertensive therapy, and from this point of view, the fact that HCTZ increases the effectiveness of all classes of antihypertensive drugs without exception when used in a combination regimen is very important. In addition, almost all representatives of the classes of ACE inhibitors, ARA II and some b-blockers are in the form of fixed combinations containing HCTZ at a dose of 12.5–25 mg. Moreover, it is HCTZ that is part of the first registered fixed three-component combination of APAII, AK and TD. All this puts HCT in the position of the most widely used TD throughout the world. The effectiveness of HCTZ as initial or adjunctive therapy on outcome has been well established in randomized controlled trials (Table 1). Use of the drug in low doses was associated with improved outcomes in a number of early and modern studies in the field of hypertension. Thus, in the placebo-controlled study EWPHE (European Working Party on High blood pressure in the Elderly trial) in patients over 60 years of age (average age 72 years) in the HCTZ therapy group 25 mg/day. and triamterene 50 mg/day. There was a significant decrease in cardiovascular mortality, mortality from myocardial infarction, and the number of non-fatal cerebrovascular complications [12]. According to the comparative study MRC Substudy (Medical Research Council trial of treatment hypertension in older adults), in the group of patients receiving diuretics (amiloride 2.5 mg/day + HCTZ 25 mg/day), the risk of developing strokes, cardiac events and all cardiovascular complications compared with the placebo group. In the atenolol group 50 mg/day. no significant reduction in the frequency of the above events was detected [28]. In the ANBP-2 study (Second Australian National Blood Pressure Study) in 6083 elderly patients with equally significant reductions in blood pressure, mixed results were obtained regarding the benefits of ACEIs over HCTZ. ACE inhibitors were more effective in preventing a combination of cardiovascular events (RR 0.89, 95% CI 0.79–1.00; p=0.05). Moreover, in the ACEI group, the risk of fatal stroke was almost twice as high as in the diuretic group (OR 1.91, 95% CI 1.04–3.5, p=0.01) [29]. Analysis of the results of the LIFE study, during which, of 9193 hypertensive patients with ECG-LVH, 70% received HCTZ in addition to the main therapy with losartan or atenolol during 4.8 years of follow-up [30], specifically addressed the question of how HCTZ administration affected outcomes. The results of the analysis showed that additional administration of HCTZ 12.5–25 mg/day. was associated with lower cardiovascular morbidity, cardiovascular and overall mortality, regardless of blood pressure reduction, regression of LVH and randomized therapy. In patients who received a diuretic, compared with those who did not receive it, the RR for the combined endpoint was 0.70 (0.62–0.80), cardiovascular death 0.58 (0.47–0.71), myocardial infarction 0 .64 (0.51–0.79), stroke 0.82 (0.68–0.99), death from any cause 0.55 (0.47–0.64). Thus, data from randomized controlled trials convincingly demonstrate the ability of HCTZ at a dosage of 12.5–25 mg/day. improve clinical outcomes in hypertension and the value of this drug in its treatment. The conclusion of thiazide diuretics still remain the cornerstone of modern antihypertension therapy and are an affordable effective class of antihypertensive drugs. This is one of the classes of antihypertensive drugs, which fully retained its value in the treatment of hypertension from the moment of its creation. Adverse metabolic effects are minimally expressed when using thiazide diuretics in low doses and do not lead to undesirable clinical consequences. Hydrochlorotiazide is one of the most studied diuretics, included in most fixed combinations of antihypertensive drugs and currently remains one of the most important drugs to reduce blood pressure, reliably reducing the risk of developing cardiovascular complications and reducing mortality from cardiovascular diseases.
References 1. Chobanian AV, Bakris GL, Black HR et al. Seventh report of the Joint National Committee on prevention, detection, evaluation and treatment of high blood pressure. Hypertension. 2003;42:1206–1252. 2. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens 2003;21:1983–1992. 3. 2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC); Journal of Hypertension. 25(6):1105–1187, June 2007. 4. Diagnosis and treatment of arterial hypertension, Recommendations of the Russian Medical Society on Arterial Hypertension and the All-Russian Scientific Society of Cardiologists, Appendix 2 to the journal “Cardiovascular Therapy and Prevention” 2008; 7(6) 5. Mancia G, Laurent S, Agabiti–Rosei E et al. Reappraisal of European guidelines on hypertension management: a European Society of Hypertension Task Force document. J Hypertens 2009, 27:2121–2158 6. Williams B, Poulter NR, Brown MJ et al. British Hypertension Society guidelines for hypertension management 2004 (BHS–IV): summary. BMJ 2004;328:634–64 7. Jamerson K, Weber MA, Bakris GL, et al. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med 2008;359:2417–28 8. Messerli FH et al. Hydrochlorothiazide is inappropriate for first–line antihypertensive therapy. ESH Meeting; June 12–16, 2009; Milan, Italy. Abstract LB1.3. 9. Blood Pressure Lowering Treatment Trialists' Collaboration. Effects of different blood pressure–lowering regimens on major cardiovascular events in individuals with and without diabetes mellitus designed: results of prospectively overviews of randomized trials. Arch Intern Med. 2005;165:1410–9. 10. Gress TW, Nieto FJ, Shahar E. et al. Hypertension and antihypertensive therapy as risk factors for type 2 diabetes mellitus. N Engl J Med 2000;342:905–912 11. Dahlof B, Sever PS, Poulter NR, et al. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo–Scandinavian Cardiac Outcomes Trial–Blood Pressure Lowering Arm (ASCOT–BPLA): a multicentre randomized controlled trial. Lancet 2005;366:895–906. 12. Fletcher A., Amery A., Birkenhager W. et al. Risks and benefits in the trial of the European Working Party on High Blood Pressure in the Elderly. J Hipertens 1991;9:225–2230 13. Hansson L, Lindholm LH, Ekbom T et al. Randomized trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity the Swedish Trial in Old Patients with Hypertension–2 study. Lancet 1999;354:1751–1756. 14. Mancia G., Broun M., Castaigne A. et al. Outcomes with nifedipine GITS or co-amilozide in hypertensive diabetics and nondiabetics in Intervention as a Goal in Hypertension (INSIGHT). Hypertension 2003;41:431–436. 15. Dahlof B, Devereux RB, Kjeidsen SE et al. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomized trial against atenolol. Lancet. 2002;359:995–1003. 16. ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high–risk hypertensive patients randomized to angiotensin–converting enzyme inhibitor or calcium channel blockers diuretic: The Antihypertensive and Lipid–Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 2002;288:2981–2997. 17. Michael E. Ernst, Pharm.D., and Marvin Moser, MD Use of Diuretics in Patients with Hypertension N Engl J Med 2009;361:2153–64. 18. Savage PH, Pressel SL, Curb D. et al. Influence of long–term, low–dose, diuretic–based anyhypertensive therapy on glucose, lipid, uric acid, and potassium levels in older men and women with isolated systolic hypertension. Arch Intern Med 1998;158:741–751. 19. Raid IR, Ames RW, Orr–Walker BJ et al. Hydrochlorothiazide reduces loss of cortical bone in normal postmenopausal women: a randomized controlled trial. Am J Med. 2000;109:362–370. 20. LaCroix AZ, Ott SM, Ichikawa L. et al. Low–Dose Hydrochlorothiazide and Preservation of Bone Mineral Density in Older Adults: A Randomized, Double–Blind, Placebo–Controlled Trial. Ann Intern Med. 2000;133:516 – 526. 21. Schoofs M, Klift M, Hofman A et al. Thiazide diuretics and the risk for hip fracture. Ann Intern Med. 2003;139:476–482. 22. Raid IR, Ames RW, Orr–Walker BJ et al. Hydrochlorothiazide reduces loss of cortical bone in normal postmenopausal women: a randomized controlled trial. Am J Med. 2000;109:362–370. 23. Psaty BM, Lumley T, Furberg CD, et al. Health outcomes associated with various antihypertensive therapies used as first–line agents: a network meta–analysis. JAMA 2003;289:2534–44. 24. Costanzo P, Perrone–Filardi P, Petretta M et al. Calcium channel blockers and cardiovascular outcomes: a meta-analysis of 175,634 patients. J Hypertens 2009; 27:1136–1151 25. https://www.medscape.com/viewarticle/702679 26. Barry L. Carter, Michael E. Ernst and Jerome D. Cohen Hydrochlorothiazide Versus Chlorthalidone: Evidence Supporting Their Interchangeability Hypertension 2004; 43;4–9 27. Emeriau JP, Knauf H, Pujadas JO et al. A comparison of indapamide SR 1.5 mg with both amlodipine 5 mg and hydrochlorothiazide 25 mg in elderly hypertensive patients: a randomized double–blind controlled study. J Hypertens 2001; 19;343–350 28. Medical research council working party. Medical research council trial to treatment of hypertension in older adults: principal results. BMJ 1992;304:405–12. 29. Wing LM, Reid CM, Ryan P. et al. Second Australian National Blood Pressure Study Group. A comparison of outcomes with angiotensin–converting–enzyme inhibitors and diuretics for hypertension in the elderly. N Engl J Med 2003;348:583–592. 30. Okin PM, Devereux RB; Hille DA et al. Concomitant Hydrochlorothiazide Therapy in Hypertensive Patients is Associated with Reduced Cardiovascular Morbidity and Mortality.
Loop diuretics
Mechanism of action
Diuretics acting at the level of the loop of Henle are the most potent representatives of this class of drugs, since 20-30% of all filtered sodium is reabsorbed through this segment of the nephron. By reducing the volume of circulating blood, loop diuretics reduce the load on the myocardium, reduce congestion in the lungs and relax the vascular wall. They are characterized by a rapid onset of action and a powerful short-term effect [7].
Indications and properties
The scope of use of loop diuretics is usually limited to emergency situations. They are prescribed for edema syndrome of various origins. In arterial hypertension, drugs of this series are used for hypertensive crises, resistance to thiazide diuretics, as well as for concomitant severe renal failure [7]. An exception may be the modern loop diuretic torasemide.
Individual representatives
- Furosemide is a powerful loop diuretic. Dilates blood vessels, increases renal blood flow, has antiaggregation activity. It is used for acute conditions, rarely for the treatment of hypertension [6]. The drug is “reserved” for patients resistant to traditional antihypertensive therapy.
- Torsemide is a loop diuretic, which is characterized by a less pronounced peak effect and a longer duration of action compared to furosemide. The antihypertensive effect has been proven in a number of clinical studies. They are used both for long-term treatment of hypertension and as part of combination therapy for chronic heart failure [7]. However, current guidelines for the treatment of hypertension do not mention the drug as a first-line treatment [3].
Portability
Loop diuretics can contribute to a sharp decrease in blood pressure and the development of orthostatic hypotension.
What should I warn the client about?
- Excessive loss of fluid and/or electrolytes may occur while taking loop diuretics. It is important to tell the buyer that if you experience dry mouth, increased thirst, or dizziness, you should contact your doctor as soon as possible.
- Loop diuretics are not recommended for use by vehicle drivers and people whose work requires increased concentration.
- Drugs in this group should not be taken at night due to their powerful diuretic effect.
Beta blockers
Beta-blockers (BABs) have been used for many years as first-line treatment for hypertension.
Mechanism of action
The action of drugs in this group is based on the blockade of β1- and β2-adrenergic receptors located in various organs. Depending on the selectivity of the blockade, which is determined by the β1/β2 ratio, beta blockers are divided into selective and non-selective. The latter (propranolol, pindolol, sotalol) are practically not used in cardiology today [8].
Modern cardioselective beta blockers (metoprolol, bisoprolol, betaxolol and others) exhibit a complex of cardiovascular effects [8]. They lower heart rate and reduce the activity of the renin-angiotensin-aldosterone system by blocking renin synthesis in the kidneys. Thus, they exhibit antianginal and antiarrhythmic effects, and also reduce blood pressure.
Indications and properties
Drugs in this group are indicated for long-term treatment of hypertension with concomitant angina, as well as for treatment after myocardial infarction and for certain types of arrhythmia.
However, beta blockers also have a significant drawback: they do not affect the incidence of cardiovascular events and arterial stiffness, and also do not have a beneficial effect on the condition of target organs [8].
Individual representatives
- Bisoprolol is one of the most popular selective β1-blockers. Provides controlled dose-dependent blood pressure reduction. Due to its high selectivity, it can be used in special groups of patients - patients with diabetes and patients with lipid metabolism disorders [9].
- Carvedilol is a drug that stands out from a number of selective biologically active agents. Shows an additional vasodilating effect. It blocks β1- and β2-receptors, as well as (slightly) α1-receptors of peripheral arteries, helping to reduce peripheral vascular resistance and a more pronounced decrease in blood pressure compared to other representatives of this group.
- Nebivolol is a new generation beta blocker with high selectivity for β1-adrenergic receptors. It has a direct vasoconstrictive effect by stimulating the production of nitric oxide by the vascular endothelium. It is tolerated significantly better than other beta blockers [9].
Portability
BBs can have a number of side effects that negatively affect the quality of life. Among them:
- heart rhythm disturbance;
- neurological reactions - depression, insomnia;
- dyspeptic symptoms - nausea, vomiting, constipation or diarrhea.
1 male patient out of 199 develops erectile dysfunction while taking drugs of this group [8].
What should I warn the client about?
Visitors, having studied the instructions for use and familiarized themselves with the impressive list of side effects, may doubt whether it is worth taking such a “harmful” drug. The primary goal is to explain that if there are indications (arterial hypertension due to coronary heart disease, cardiac arrhythmias, heart failure, migraine, pregnancy, glaucoma), the benefits of taking beta blockers are much higher than the potential risk of side effects. In addition, according to research, only 3–5% of patients cannot take drugs from this group due to developing adverse reactions [8].
Currently generally accepted recommendations for the treatment of arterial hypertension (AH) [1] imply the use of representatives of 5 classes of antihypertensive drugs as the main drugs, among which thiazide diuretics (TDs) still retain their position. Like other antihypertensive drugs, they are not completely free from certain undesirable effects, which, however, are not a reason to refuse them. The prescription of TDs in the treatment of hypertension is justified from a pathogenetic point of view, supported by long-term experience of their use in clinical practice and the results of controlled clinical studies, indicating a significant positive effect of this class of drugs on the long-term prognosis of patients.
Why did TD begin to be used for the treatment of hypertension?
Back in the first half of the twentieth century. sodium and water retention was recognized as one of the central components of the pathogenesis of most clinical variants of hypertension; moreover, it was often given a decisive role in the formation of a persistent increase in blood pressure (BP) [2]. Before the advent of truly effective antihypertensive drugs in patients with hypertension, including severe hypertension, it was possible to achieve a noticeable reduction in blood pressure by sharply limiting the consumption of table salt. A series of studies by Wallace Kempner in the 1940s is considered classic. demonstrated the possibility of significantly reducing blood pressure in patients with high hypertension, including kidney disease, by changing the diet, which meant eliminating foods containing salt. Patients received only rice and fruit; at the beginning of the observation period, they tolerated the complete cessation of access to table salt very poorly (even to the point of suicide attempts). Subsequently, many people began to feel disgusted by salty food, which often coincided with a decrease in systolic blood pressure (SBP) and diastolic blood pressure (DBP) [3].
TD is the product of a targeted search for approaches to controlling the function of tubular transport systems (interestingly, this search was initially aimed at developing agents that slow down the excretion of expensive penicillin and, therefore, prolong its action). The ability of TDs to reduce blood pressure and, in certain doses, to significantly increase diuresis is determined by their effect on the Na+/Cl- transporter of the distal nephron tubules [4]. By interacting with the Cl-binding center of the transporter, these drugs cause an increase in the excretion of sodium and chloride ions, and, consequently, an increase in the clearance of osmotically bound water, while the pre- and afterload on the left ventricular myocardium decreases, and blood pressure decreases.
The significance of the described mechanisms in the development of the antihypertensive effect of TD was established back in the late 1950s – early 1960s. Wilson IM et al. (1959) [5] demonstrated that in patients with hypertension, taking chlorothiazide is accompanied by a decrease in blood plasma volume, body weight, and an increase in urinary excretion of sodium, chloridione and potassium; in parallel, most patients experienced a decrease in blood pressure. In most patients, these effects of chlorothiazide persisted even with long-term (12 months) use of this drug, but disappeared relatively quickly after its discontinuation. Thus, it can be argued that the antihypertensive effect of TDs is determined primarily by their ability to stimulate natriuresis and the excretion of osmotically bound water.
Have the benefits of TD been confirmed in controlled clinical trials?
TD is a class of antihypertensive drugs, the use of which has been able to justify the need for continuous treatment of hypertension with the achievement and maintenance of target blood pressure values. It is well known that until the second half of the 1970s. The practice of treating hypertension primarily meant stopping hypertensive crises and lowering blood pressure in a situation where its increase was accompanied by a deterioration in well-being, for example, a headache. The benefit of chronic use of antihypertensive drugs was considered not obvious, and in some categories of patients (for example, the elderly) even dangerous. However, in the early 1970s. Freis ED, comparing outcomes in groups of patients who received constant antihypertensive therapy (its main component was hydralazine) or placebo, showed a significant difference in the incidence of cerebral strokes, which indicated the need for a constant reduction in blood pressure [6]. These data were obtained as part of a large study, the Veterans Administration Cooperative Study, the results of which also showed a significant reduction in the incidence of ECG abnormalities, achieved through the constant use of antihypertensive drugs, including hydrochlorothiazide (HCTZ) [7]. Thus, the incidence of left ventricular hypertrophy, registered on the basis of an increase in the Sokolov-Lyon index > 35 mm, was 28% in those taking placebo and 6% in the group of patients receiving antihypertensive drugs (p < 0.005). Moreover, the Veterans Administration Cooperative Study demonstrated that long-term use of antihypertensive treatment regimens including HCTZ can reduce the Sokolov-Lyon index, indicating regression of left ventricular hypertrophy: the incidence of this effect was 32% in those treated and 6% in those taking placebo (p < 0.005).
The Hypertension Detection and Follow-up Program study, conducted at 14 US clinical centers, included 10,940 patients with previously untreated hypertension aged 30 to 69 years. Patients were randomized to the then generally accepted antihypertensive therapy regimen (taking an antihypertensive drug if clinically indicated) or to continuous use of antihypertensive drugs that ensured maintenance of DBP < 90 mmHg. Art. A five-year follow-up of patients continuously receiving antihypertensive drugs was designed to confirm or refute the benefit of continuous drug normalization of blood pressure in terms of its effect on mortality. The majority of patients enrolled in the Hypertension Detection and Follow-up Program study were receiving HCTZ; If necessary, other antihypertensive drugs were added.
Contrary to the initial belief that continuous use of antihypertensive drugs, especially those with a diuretic effect, would be poorly tolerated by patients, more than 80% of patients randomized to continuous antihypertensive therapy were adherent to it and more than 75% of them achieved target DBP [8 ]. Moreover, chronic antihypertensive therapy using HCTZ was found to achieve a significant reduction in overall mortality compared with those receiving episodic antihypertensive therapy; this difference remained statistically significant regardless of the degree of blood pressure increase, age, sex, and race [9]. The prognostic advantages of continuous antihypertensive therapy were explained primarily by a significant decrease in blood pressure compared with the group where antihypertensive drugs were taken occasionally [10].
TD is a class of antihypertensive drugs, thanks to which it was possible to radically change the fate of patients with isolated systolic hypertension, demonstrating that they require constant antihypertensive therapy (until the early 1990s, they were practically not given due to the fact that it was considered dangerous, and An increase in blood pressure with age was considered as a variant of the norm). In the SHEP study, patients with isolated systolic hypertension over the age of 60 years were randomized to receive TD chlorthalidone (12.5–25 mg) or placebo. The follow-up period was 5 years. The primary endpoint was any new cardiovascular complication. Treatment with chlorthalidone was accompanied by a reduction in the incidence of non-fatal cerebral stroke by 37%, non-fatal acute myocardial infarction by 33%, and chronic heart failure (left ventricular) by 54%. In addition, a 25% reduction in the number of transient ischemic attacks, as well as overall (13%), cardiovascular (20%), cerebrovascular (29%) and coronary (15%) mortality was recorded [11]. The achieved improvement in cardiovascular prognosis persisted 14 years after the end of the study [12].
The well-known large controlled trial ALLHAT, the results of which remain one of the main events in cardiology of the 2000s, was planned with the aim of possibly demonstrating the benefits of newer classes of antihypertensive drugs compared with TD (ACE inhibitor, long-acting dihydropyridine calcium antagonist, α- adrenergic blocker) from the point of view of the effect on cardiovascular prognosis in patients with hypertension who had other risk factors. However, neither the ACE inhibitor nor the long-acting dihydropyridine calcium antagonist reduced the likelihood of the primary endpoint of nonfatal acute myocardial infarction and cardiovascular death more than TD, and the α-blocker did not. In comparison, it even worsened the cardiovascular prognosis: in particular, with its use, a significant increase in the number of new cases of chronic heart failure was noted [13]. The prognostic effectiveness of TD in the ALLHAT study did not depend on the race of the patient (the large number of included African Americans initially caused some criticism due to the fact that in this category of hypertensive patients TD is obviously superior in effectiveness to other classes of antihypertensive drugs) [14].
Thus, the rationale for the need for continuous treatment of hypertension is largely related to clinical studies in which TDs were used. Both when compared with true placebo and when compared with other classes of antihypertensive drugs, TDs have demonstrated the ability to significantly reduce the risk of disabling and potentially fatal cardiovascular events.
What are the possible limitations for prescribing TD for hypertension?
The use of TD, like other classes of antihypertensive drugs, may be associated with the development of certain adverse events. Thus, it is well known that taking TD can provoke the development of gouty arthritis [15]. A 52-year follow-up of women enrolled in the Framingham Heart Study [16] showed that TD use was associated with a 2.39-fold increase in the risk of gouty arthritis, but was not the most significant determinant of articular gout (its risk increased by 2.74). times with increasing age for every 5 years and 3.1 times with consumption of more than 200 ml of ethanol per week). However, this does not mean that TDs themselves cause uric acid metabolic disorders: it is obvious that they aggravate the already existing urate dysmetabolism, which is widespread in the general population and makes a certain contribution to the formation of essential hypertension [17, 18]. Obviously, in patients with hyperuricemia, TD can be prescribed only after the dose of allopurinol has been adjusted, and only in a situation where the patient is on a low-purine diet.
Most of the adverse events associated with the use of TD (erectile dysfunction, worsening metabolic disorders) are caused by a decrease in serum potassium concentration that occurs in some cases. According to large controlled studies, the incidence of TD-induced hypokalemia is generally low and does not exceed 8% [19]. It must be emphasized that increasing potassium intake with food and taking medications containing potassium can reduce the incidence of TD-induced (or more often aggravated in the presence of more significant predisposing factors: type 2 diabetes mellitus (T2DM) and smoking) erectile dysfunction [20]. In addition, the vast majority of patients receiving TDs today take them in combination with ACE inhibitors or angiotensin II receptor blockers, which are known to significantly reduce the likelihood of hypokalemia.
A decrease in serum potassium concentration and metabolic disorders are observed in the vast majority of cases when TD is used in doses significantly higher than currently recommended for mono and combination therapy. For example, in a systematic review by Zillich AJ et al. (2006) [21], which summarized 59 clinical studies, the maximum dose of chlorthalidone was 100 mg/day, and HCTZ was 400 mg/day (i.e., 16 times more than the maximum dose that is currently usually used for the treatment of hypertension ).
T2DM associated with the use of TD - a danger that can be controlled?
Noted in some controlled clinical trials, for example in ASCOT-BPLA [22], an increase in the number of new cases of T2DM in groups of patients taking TD has become the basis for attempts to reconsider the role of this class of antihypertensive drugs in the treatment of hypertension and is considered as an argument in favor of their exclusion number of first line funds. This point of view is obviously not justified, if only because the greatest risk of T2DM was found when TD was combined with α-blockers, which themselves significantly increase the likelihood of clinically obvious disorders of carbohydrate metabolism.
It is known that the formation of T2DM associated with the intake of TD is determined by a decrease in serum potassium concentration, causing an increase in insulin resistance and a disruption of the phasicity of insulin secretion by pancreatic α-cells [23]. An analysis of the SHEP study population published in 2008 [24] showed that a 0.5 mEq/L decrease in serum potassium concentration was associated with a 45% increase in the risk of T2DM (p < 0.001). Moreover, the likelihood of T2DM increased maximally during the first year of chlorthalidone use, thus being associated with initial changes in potassium concentrations. If hypokalemia is not observed at the beginning of TD treatment, the factors leading to it are eliminated (for example, concomitantly used loop diuretics in large doses), and the patient receives potassium-containing drugs, the likelihood of TD-induced diabetes is most likely low.
In addition, T2DM associated with the use of TD apparently does not lead to a significant deterioration in the prognosis of patients. In the previously mentioned SHEP study, the presence of T2DM at baseline or its development during follow-up was associated with a significant increase in mortality. However, in the group of patients in whom the development of T2DM was associated with taking the TD chlorthalidone, there was no increase in overall and cardiovascular mortality [25]. It should be noted that patients who had T2DM and received TD demonstrated the lowest cardiovascular and overall mortality rates.
Thus, TD should not be considered as drugs with a clear “diabetogenic” effect. They obviously should not be used primarily as monotherapy in patients with metabolic syndrome and/or with established insulin resistance, as well as in combination with β-blockers, especially those without cardioselectivity. The increased likelihood of T2DM observed in some categories of patients receiving TD generally reflects the scale of the epidemic of this disease and the conditions that predispose to its development.
What are the indications for the use of TD in hypertension?
Currently, the vast majority of patients with hypertension require combination antihypertensive therapy at the first stage of treatment[26]. TD, in particular HCTZ, is almost always included in combinations as the second or third drug. It must be borne in mind that their combination with ACE inhibitors and especially with angiotensin II receptor blockers makes it possible to achieve almost complete neutralization of negative metabolic effects [27]. In addition, the use of HCTZ, which makes it possible to control natriuresis, disorders of which still remain one of the central mechanisms of the development of hypertension, allows for a greater reduction in SBP, which is especially important for patients with high/very high risk hypertension. HCTZ also demonstrates significant advantages in hypertension associated with chronic heart failure. In this regard, despite the emergence of new classes of antihypertensive drugs, the history of the use of TD in hypertension will undoubtedly continue.