Heart failure is a pathophysiological syndrome in which, as a result of a disease of the cardiovascular system, pumping function is reduced, which leads to an imbalance between the hemodynamic need of the body and the capabilities of the heart. Acute heart failure is a consequence of impaired myocardial contractility, a decrease in systolic and cardiac output. The pathology is manifested by extremely severe clinical syndromes: pulmonary edema, cardiogenic shock, acute cor pulmonale.
Chronic heart failure is manifested by a complex of characteristic symptoms (shortness of breath, fatigue and decreased physical activity, edema), which are associated with inadequate perfusion of organs and tissues at rest or during exercise and often with fluid retention in the body. For the treatment of patients suffering from heart failure, the Yusupov Hospital has created all the necessary conditions:
- Chambers with European level of comfort;
- Equipping with life-supporting equipment of expert class;
- Modern methods for identifying the causes of heart failure;
- Treatment with the latest drugs that are highly effective and have a minimal range of side effects.
Severe cases of heart failure with patients experiencing severe shortness of breath and rapid heartbeat are discussed at a meeting of the Expert Council. Doctors and candidates of medical sciences, doctors of the highest category collectively develop the optimal scheme for managing patients. The most severe patients with heart failure are treated in the intensive care unit. It is equipped with modern medical equipment, which allows emergency care to be provided in accordance with current European and domestic standards. If indicated, resuscitators use stationary or portable artificial lung ventilation devices. Relatives of patients may be present in the wards.
Causes of development of chronic heart failure
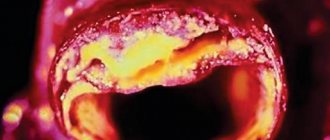
Chronic heart failure can develop in patients suffering from coronary heart disease, arterial hypertension, and heart defects. In coronary heart disease, a common cause of left ventricular systolic dysfunction and chronic heart failure is acute myocardial infarction and ischemic cardiomyopathy. The progression of chronic heart failure is caused by changes in the geometry and local contractility of the heart muscle.
In patients suffering from hypertension, regardless of the cause of arterial hypertension, a structural restructuring of the myocardium occurs, which is called a “hypertensive heart”. Chronic heart failure develops as a result of acquired and uncorrected rheumatic defects. Other causes of chronic heart failure include infective endocarditis, toxic cardiomyopathy due to exposure to drugs, alcohol, radiation therapy, systemic vasculitis, metabolic and endocrine disorders.
Composition and release form
The medicine is flat round white tablets. There is a dividing line on the front side. The corner is a little skewed. This chamfer makes the tablet easy to swallow. The letter D is engraved on the reverse side. The drug is sold in bottles. Each bottle contains 50 tablets.
The main active ingredient of the drug is digoxin. Auxiliary elements have been added to it. 1 tablet contains 0.25 mg of digoxin. It is obtained from raw materials of foxglove (Digitalis lanata). This perennial plant contains many cardiac glycosides that are used in medicine.
Digoxin is also available as a solution for injections. The amount of digoxin in it is 0.25 mg. It is supplemented with injection water, ethyl alcohol, glycerin and citric acid.
This medicine is a cardiac glycoside that normalizes blood pressure, rhythm and heart sounds. Digoxin has a beneficial effect on the heart muscle and belongs to the group of cardiotonic drugs.
Symptoms of chronic heart failure
Shortness of breath is one of the earliest symptoms of heart failure. In the initial stages of the disease, shortness of breath occurs only during intense physical activity. As the disease progresses, the load threshold decreases. Patients with severe heart failure complain of shortness of breath at rest.
Orthopnea is shortness of breath that occurs when lying down, especially with a low headboard. She disappears into a vertical position. Shortness of breath in heart failure appears after a few minutes of the patient being in a horizontal position. It disappears just as quickly in a standing or sitting position. The cause of orthopnea is an increase in venous blood flow to the heart and overflow of blood into the pulmonary circulation.
Patients with heart failure are bothered by a rapid heartbeat. This is a compensatory mechanism that is aimed at maintaining minute blood volume in conditions of decreasing stroke volume. Patients complain of interruptions in the functioning of the heart, which may be a manifestation of rhythm disturbances observed in patients with heart failure.
Strong palpitations and shortness of breath on exertion are accompanied by a dry, unproductive cough. It appears in a horizontal position of the patient. Cough in heart failure occurs due to congestion in the lungs, swelling of the bronchial mucosa and irritation of cough receptors. Early signs of the development of heart failure are weakness, increased fatigue and heaviness in the lower extremities. These complaints appear due to impaired blood supply to skeletal muscles.
With systolic heart failure, patients experience swelling in the lower extremities. Initially, they are located in the ankles and feet, appear in the evening and disappear in the morning after rest. As heart failure progresses, swelling spreads to the lower legs and thighs. They become more persistent, intensify in the evening and do not disappear after rest.
In the early stages of heart failure, patients develop nocturia, an increase in urine output at night. It is associated with differences in blood flow in the renal arteries in patients with heart failure at rest and during exercise. a significant decrease in daily diuresis (oliguria) - indicates a significant decrease in renal blood flow and cardiac output even at rest. It is characteristic of late stages of heart failure.
Dosage and instructions for use
Digoxin is prescribed only in the hospital for inpatient treatment, so that doctors have the opportunity to monitor the patient’s condition. The dose is selected individually for each patient, taking into account his muscle mass.
Types of therapy:
- rapid digitalization - the patient receives about 0.75–1.5 mg;
- gradual digitalization - the patient is prescribed 1-3 tablets per day (0.25-0.75 mg per day) for 5-7 days;
- therapeutic support - 0.5–1 tablet per day (0.125–0.25 mg of substance).
For older people, reduced doses are chosen. Patients should not change the dosage themselves.
For atrial fibrillation, a higher dose is prescribed than for CHF. It decreases slightly if the patient has serious kidney disease, hypothyroidism, low calcium levels, or if the muscles are underweight.
Examination of patients with chronic heart failure
When examining a patient with shortness of breath, the doctor sees rapid breathing. The patient with shortness of breath takes a vertical position. In order to reduce shortness of breath in severe heart failure, patients take a forced sitting position with their legs down. They have pale skin that is cold to the touch. Excessive sweating develops as a result of increased activity of the sympathetic nervous system, slower peripheral blood flow and decreased blood supply to the tissue. Due to an increase in the content of reduced hemoglobin due to an increase in the release of oxygen from venous blood in patients suffering from heart failure, the skin of the torso, limbs, tip of the nose, and earlobes acquires a bluish tint. A manifestation of increased venous pressure is swelling of the neck veins.
Patients with shortness of breath experience increased breathing. When percussing the lungs in the presence of congestion, pulmonologists determine dullness of the percussion sound. Against the background of harsh or weakened breathing, moist, fine, silent rales or crepitus are heard in the lower parts of the lungs. Hydrothorax may occur in patients with biventricular heart failure. The fluid is located in the lower parts of the pleural cavity on the right or on both sides.
When examining the cardiovascular system, physical data reflect signs of the underlying disease, which is the cause of the development of heart failure. The boundaries of relative cardiac dullness may not change, shift to the right, left, or in both directions. In patients with coronary heart disease, the development of decompensation is accompanied by a weakening of the first tone, an accent of the second tone on the pulmonary artery can be heard, and with the development of relative atrioventricular insufficiency - systolic murmur.
Yusupovskaya’s doctors use the following laboratory diagnostic methods for heart failure:
- Clinical blood and urine tests;
- Determination of serum electrolytes;
- Estimation of glomerular filtration rate;
- Blood glucose level;
- Liver tests.
Considering that drugs that are used for shortness of breath due to heart failure affect the level of potassium in the blood, this indicator must be determined. To confirm the diagnosis of heart failure, a study of the level of natriuretic peptides - brain natriuretic peptide and its N-terminal fragment - is carried out.
The electrocardiogram reveals nonspecific changes that are characteristic of the underlying disease, rhythm and conduction disturbances, or coronary circulatory failure. Transient myocardial ischemia, rhythm and conduction disturbances are detected using 24-hour Holter ECG monitoring.
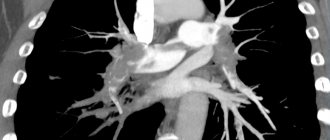
X-ray examination of the chest organs reveals an increase in the size of the heart and congestion in the pulmonary circulation. Echocardiography is an extremely important and basic method for assessing central hemodynamics and blood movement within the cavities of the heart. Using ultrasound, doctors clarify the origin of chronic heart failure, determine the nature and severity of dysfunction of the left ventricle, and objectively assess the dynamics of the process and the effectiveness of the therapy.
When performing echocardiography in M-mode, functional diagnostic doctors measure the size of the heart cavities, evaluate the structure and functional viability of the heart valves, and clarify the homogeneity and contractility of the myocardium. In order to objectify the condition of patients suffering from chronic heart failure, a six-minute walk test is performed:
- Measure a distance of 20 meters;
- Install 2 chairs at the ends of the distance;
- The patient is asked to walk from chair to chair for 6 minutes at his usual pace;
- After 6 minutes, the distance traveled is determined.
When assessing symptoms, the presence of dizziness, anginal pain in the heart, shortness of breath, and fatigue are taken into account. Before starting the test and immediately after its completion, heart rate and respiratory movements, and blood pressure are recorded. To determine the cause of chronic heart failure, invasive diagnostic methods are used: coronary angiography in combination with ventriculography.
Contraindications
There are many contraindications for which Digoxin cannot be taken.
- congenital heart defects - stenosis, Wolff-Parkinson-White syndrome (WPW);
- ventricular fibrillation;
- poisoning with cardiac glycosides;
- II degree of AV heart block;
- ventricular tachycardia;
- tamponade;
- intermittent complete block of the bundle branches;
- allergy to medication components;
- transient complete AV block;
- lactation period;
- age under 3 years;
- obstructive hypertrophic cardiomyopathy (without CHF and atrial fibrillation);
- disturbances in the absorption of lactase, glucose and galactose.
Digoxin should be taken with great caution for a number of diseases and conditions:
- mitral valve stenosis;
- I degree of AV block;
- unstable forms of angina;
- sick sinus syndrome;
- acute stage of myocardial infarction;
- renal or liver failure;
- manifestations in the past of MAS syndrome (Morgagni-Adams-Stokes);
- obesity;
- risk of unstable impulse conduction through the AV node;
- oxygen starvation;
- cardiac asthma (especially in combination with mitral valve stenosis);
- pericarditis;
- arteriovenous fistula (shunt);
- hypothyroidism;
- amyloid cardiac dystrophy;
- any type of restrictive cardiomyopathy;
- dilatation of the heart chambers;
- inflammatory myocardial disease;
- excess alkaline substances in the body (alkalosis;
- extrasystole;
- electrolyte imbalance (increased calcium and sodium, decreased magnesium and potassium);
- elderly age of the patient;
- slow heart rate (bradycardia);
- severe or chronic lung diseases;
- carotid sinus syndrome;
- "pulmonary" heart.
The doctor carefully examines the patient’s health condition and prescribes the appropriate medicine and its exact dosage.
Overdose
An excessive dose of Digoxin is extremely dangerous and can lead to the death of the patient. Overdose happens quite often. If the level of digoxin in the blood plasma reaches 2 ng/ml, this concentration is toxic and life-threatening. The lethal dose is 10 mg.
Main symptoms:
- any heart rhythm disturbances;
- sweating;
- the ECG shows trough-shaped depression of the ST segment (a sign of the presence of digitalis in the body, and not just an overdose);
- hallucinations;
- dizziness and pain;
- distorted color perception;
- digestive disorders;
- drooling, poor appetite;
- weakness;
- sensitivity disorders;
- depressed mental state;
- disorientation;
- AV block;
- various cardiac conduction disorders;
- on the ECG the PQ interval lengthens.
In children, signs of gastrointestinal disorders are more common. Cardiac conduction disturbances and some types of arrhythmias are also observed.
The doctor immediately prescribes an antidote and other therapy that will eliminate the symptoms and improve the patient’s condition. An electrical pacemaker will be needed if the patient has Morgagni-Adams-Stokes attacks and complete transverse heart block. A pacemaker is installed temporarily until the serious condition disappears.
Can I take it during pregnancy?
Pregnant women can take Digoxin only as prescribed by a doctor. This medicine does not harm the baby, but can penetrate the placenta into the fetus. A pregnant woman may need an increased dosage of the drug. Digoxin can lead to the birth of a low birth weight baby. Excess of substances contained in digitalis greatly harms the unborn child. During breastfeeding, you should also avoid taking Digoxin, because it enters the baby’s body through breast milk.
2. Drug treatment of the disease
To treat COPD, medications are also used that can perform different functions. Yes, bronchodilators
help open the bronchi, which in turn makes breathing easier. These medications may be short-acting (to quickly relieve symptoms of the disease) or long-acting to help prevent them.
Anti-inflammatory drugs
to treat COPD symptoms (such as corticosteroids) may come in the form of tablets or inhalers that help the medicine go directly to the lungs.
Visit our Pulmonology page