The article was checked by vascular surgeon A.R. Rakhimov. , is for general informational purposes only and does not replace specialist advice. For recommendations on diagnosis and treatment, consultation with a doctor is necessary.
Buerger's disease , or thromboangiitis obliterans , is a systemic immunopathological inflammatory disease of small and medium-sized vessels of the extremities, in which obliteration of the arteries occurs and migratory thrombophlebitis occurs. The disease mainly affects young people under the age of 40.
Causes of Buerger's disease
- Tobacco smoking is one of the main factors that leads to spasm and thrombosis of peripheral arteries
- infectious diseases (caused by streptococci, chlamydia, etc.)
- autoimmune factors - tissue destruction due to the production of antibodies to elastin, collagen, laminin
- trauma, arsenic intoxication, allergy genetic factor
- increased lipoprotein A levels
- increased adrenal function
- organic lesions of nerve fibers
Thromboangiitis obliterans, progressing, goes through three main stages:
- angiospastic
- angiothrombotic
- angiosclerotic or gangrenous
Postthrombophlebitic syndrome - what is it?
Postthrombophlebitic syndrome (PTPS) is a complex of pathological symptoms that develop after deep vein thrombosis, subject to insufficient recanalization of thrombosed venous segments and weak compensatory capabilities of the body. In modern European literature, postthrombophlebitis syndrome is also called venous stress disorder. A disease that occurs as a complication of long-term disruption of venous outflow after deep vein thrombosis (DVT). Postthrombophlebitic disease
Diagnosis of Buerger's disease at the Yauza Clinical Hospital
Specialists at the Yauza Clinical Hospital make a diagnosis after collecting an anamnesis, based on a visual examination and data from instrumental methods. Upon examination, a change in the color of individual areas of the skin, a decrease in their temperature, and trophic disorders are revealed. We perform ultrasound of the arteries, echocardiography, and angiographic examination. It should be noted that due to the objective difficulties in making a diagnosis, it is often made by excluding other diseases with similar clinical manifestations (for example, obliterating endarteritis, Raynaud's disease).
Medical Internet conferences
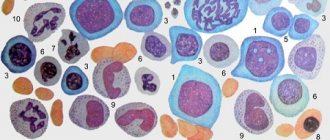
Relevance of the problem. Nowadays, there is an increasing increase in the incidence of systemic vasculitis, especially in people of working age. This is due both to diagnostic difficulties and to a significant increase in the impact of adverse (viral, chemical, toxic) environmental factors on the human body, causing the development of immune inflammation in the walls of blood vessels. Systemic vasculitis (SV) is a group of diseases based on generalized damage to the vascular wall of immune origin with the development of inflammation and necrosis, leading to impaired blood flow in organs and tissues. Systemic vasculitis is one of the most severe forms of human chronic inflammatory diseases.[1]
With various vasculitis, the severity of clinical manifestations, as well as the prognosis, will depend both on the nature of the immune-inflammatory process in the vascular wall, and on the type, caliber and location of the affected vessels, the course and severity of concomitant inflammatory changes in the tissues.[1] Among the most common vasculitis affecting small and medium-sized vessels, our attention was drawn to thromboangiitis obliterans, or in the English literature, “Winiwarter-Buerger disease.” The disease is more common in young men with a long history of smoking, while the progression of the pathological process with an increase in ischemic disorders in the extremities and changes in the vessels of internal organs lead to early disability of patients.[2] Today, there is no doubt about the relationship between immune inflammation and the development of thrombosis due to the fact that these processes are based on many similar pathogenetic mechanisms. Complications of a thrombotic nature remain one of the most severe and life-threatening conditions that occur in patients with systemic vasculitis. [3]
Objective: To demonstrate the diagnostic difficulties in managing a patient with Buerger's disease. Objectives: analysis of a clinical case of a patient suffering from thromboangiitis obliterans with assessment of clinical and laboratory-instrumental data with the establishment of leading syndromes, use of diagnostic criteria “disease development”, “treatment effect” when making a diagnosis.
Materials and methods: a retrospective analysis of the medical history and supervision of a patient with a final diagnosis of Buerger's disease involving the vessels of the upper and lower extremities was carried out.
Results: Patient N., 40 years old, was admitted to the cardiology department of the S.R. Clinical Hospital. Mirotvortseva SSMU on March 28, 2021 with complaints of mixed shortness of breath at rest and in a position with a low head, tachycardia, weakness accompanied by cold sweat, pain in the left leg, in the right half of the chest. From the anamnesis it is known that the symptoms manifested acutely: on March 26, for no apparent reason, constant pain appeared in the left lower leg, inspiratory shortness of breath with slight physical exertion, and severe weakness. However, the symptoms did not increase and he continued to lead his usual lifestyle (went to work). On March 28, he noted a sharp deterioration in his general condition: severe weakness appeared, severe shortness of breath, and he broke out in a cold sweat. He was taken to the cardiology department by ambulance with a preliminary diagnosis of pulmonary embolism (PE). From his life history it is known that over the past 6 years he suffered three times severe pneumonia, complicated by hemoptysis. I suffered from arterial hypertension for about 5 years.
Upon admission, the condition was assessed as severe, the skin was pale, acrocyanosis, and pastiness of the left leg. Prefers a position with an elevated headboard. The respiratory rate is 22 per minute, shallow breathing, with an open mouth. Auscultation of the lungs reveals harsh breathing, weakened on the right in the lower parts, no wheezing. The borders of the heart are expanded to the left to the left midclavicular line. The heart sounds are weakened, the emphasis of the 2nd tone is on the pulmonary artery. Blood pressure 100 and 60 mmHg. Heart rate 100 per minute. Plesh's symptom is negative. The abdomen is slightly painful on palpation in the right hypochondrium. The liver cannot be detected by palpation. In other organs there are no features. Additional examination revealed: moderate leukocytosis (up to 16*109/l), increased level of C-reactive protein (CRP) to 28 mg/l, ALT, AST more than 2 upper limits of normal; the level of markers of myocardial necrosis (troponins, CPK-MB), coagulogram parameters are normal. An electrocardiographic study (ECG) revealed a deviation of the electrical axis of the heart to the right, right bundle branch block, QIII, SI. On March 29, a duplex scan of the veins of the lower extremities was performed, which revealed thrombosis of the popliteal and superficial femoral veins on the left with the apex of the thrombus localized in the superficial femoral vein at the level of the c/3 thigh; passable lumen of veins from 10% to 60%. Doppler echocardiography (DEchoCG) revealed signs of significant dilatation of the right ventricle (RV) and moderate dilatation of the right atrium (RA). In the cavity of the RA, two ribbon-like floating thrombi were identified, about 5.0 and 7.0 cm long, about 1.0 cm thick, which from the mouth of the vena cava reached the tricuspid valve (TV) leaflets. There were no echo signs of TC obstruction. Tricuspid regurgitation is significant (grade III). Paradoxical movement of the interventricular septum, caused by volume overload of the RV, and hyperkinesis of the posterior wall were determined. Myocardial thickness, chamber size and global contractility of the left ventricle were normal (ejection fraction about 63% according to the Teichgolz formula). Signs of cardiac decompensation in the systemic and pulmonary circulation were established (dilation of the inferior vena cava (IVC) up to 2.7 cm without signs of collapse, high-grade pulmonary hypertension - systolic pressure in the pulmonary artery (SPAP) 80 mmHg). An ultrasound examination of the abdominal cavity revealed signs of hepatomegaly and congestion in the IVC system. When X-raying the chest organs, there was an increase in the pulmonary pattern in the basal sections due to full-blooded vessels; in the area of the apexes of the lungs and the marginal border of the pulmonary fields, the pulmonary pattern was not traced. The mediastinal organs are unremarkable.
Based on the development of the disease (male gender, onset of the disease before 40 years of age, recurrent venous thrombosis complicated by embolism, increased levels of CRP), it was suggested that the patient has Buerger's disease, which has an atypical course (absence of clinical and instrumental signs of arterial damage).[ 4]
Treatment with anticoagulants, calcium channel blockers, β-blockers, glucocorticoids, antibacterial therapy, and gastroprotection was prescribed. Considering that the patient has a very high risk of developing pulmonary embolism (13 points on the GENEVA scale) and echocardiography data (blood clots in the RA cavity), a decision was made to conduct thrombolytic therapy with streptokinase. During treatment, the patient's condition improved significantly: chest pain, shortness of breath at rest were relieved, and exercise tolerance increased. On April 11, a repeat echocardiogram was performed, which showed positive dynamics in the form of lysis of one of the thrombi and a reduction in the size of the second (in the RA, one ribbon-like floating thrombus is visualized, about 5.0 cm long and about 0.6 cm thick, reaching the TC). Tricuspid regurgitation (I degree) and pulmonary hypertension (I degree, MPAP 36 mm Hg) decreased, signs of circulatory failure in the systemic circle stopped (IVC 1.8 cm, collapses on inspiration). On April 12, 2021, a repeat duplex scan of the veins of the lower extremities was performed, where an improvement was also noted in the form of a decrease in the length of the blood clot.
Conclusion. This clinical case clearly demonstrated the atypical course of Buerger's disease. As a rule, thromboangiitis obliterans is a chronic disease of small and medium-sized arteries and veins. The clinical picture of the disease is dominated by signs of damage to the veins of the lower extremities, which is quite rare.[5] Quick diagnosis, choice of rational patient management tactics and the use of high-tech medical care significantly improve the prognosis of the disease.
Treatment of thromboangiitis obliterans at the Yauza Clinical Hospital
Vascular surgeons at the Yauza Clinical Hospital provide conservative treatment in the initial stages of Buerger's disease. It involves the use of vasodilator drugs throughout life, which minimize the risk of complications and further progression of the disease. We also prescribe training walking, photohemotherapy, plasmapheresis, and hemosorption to patients. A very important point is to quit smoking. In some cases, surgical intervention is required - sympathectomy. In the final stages of the disease, limb amputation may be performed.
You can see prices for services
X-ray angiography
To clarify the diagnosis, the attending physician refers the patient to X-ray angiography, as well as duplex scanning via ultrasound. Both methods allow one to analyze the condition of blood vessels with a high degree of accuracy. In addition, there is rheovasography, which allows you to evaluate blood circulation in the legs and arms, and Doppler flowmetry, which checks microcirculation in small vessels. In addition, blood tests for circulating immune complexes are often performed.
Recommendations
A person suffering from Buerger's disease must immediately stop smoking - otherwise the disease will only progress. In addition, the patient should avoid skin damage due to exposure to high or low temperatures, chemicals, lesions associated with wearing uncomfortable shoes, minor operations (for example, callus removal), fungal infections.
All patients (except patients with ulcers and gangrene on the affected limbs) are recommended to walk briefly (20-30 minutes) several times a day.
Video from YouTube on the topic of the article:
Postthrombophlebitic syndrome, stages and forms
Postthrombophlebitis syndrome is part of the structure of diseases manifested by symptoms of chronic venous insufficiency (CVI). The most modern and relevant gradation of postthrombophlebitis syndrome today is the CEAP classification. This tool most accurately describes the trophic and morphological changes that occur in the lower limb during the development of pathology. Also, doctors in many public medical institutions use the GHPratt classification, as modified by M.I. Cousin. According to it, postthrombophlebitis syndrome is divided into the following forms:
- Edema and pain
- Varicose
- Ulcerative
- Mixed
Classification
Buerger's syndrome is associated with inflammation, it is strictly limited to certain parts of the arteries and causes the formation of clots that completely block the vessel. The cause is an immune reaction due to hereditary preload, which is caused by foreign substances (antigens) contained in tobacco.
Depending on which part of the artery the blood flow is obstructed, there are 3 types of disease:
- Distal type (60-65% of the total), characterized by narrowing of small-diameter arteries.
- Proximal type (15-20%), damage to arteries of medium and large diameter.
- Mixed type (15-20%), a combination of the first two types of lesions.
In severe cases of the disease
The severe course of the disease is characterized by frequent exacerbations with a progressive deterioration of the blood supply to the blood vessels of the legs.
- The pain syndrome is more intense.
- The pain bothers me without connection with exercise, day and night.
- Easier when lowered.
- The patient’s posture is typical: sitting on the bed at night, supporting the sore leg, trying to massage it to relieve numbness.
- The appearance of a brown spot on a finger is regarded as the beginning of dry gangrene (death of tissue).
- The spot enlarges and the color changes to black.
- Due to additional infection of tissues, the stage of wet gangrene occurs.
Postthrombophlebitic syndrome - symptoms
Signs and symptoms of postthrombophlebitis lower extremity syndrome may include:
- pain
- night muscle cramps
- heaviness
- itching and/or tingling
- edema
- phlebeurysm
- skin hyperpigmentation
- lipodermatosclerosis
- trophic ulcer.
These signs and symptoms can vary significantly between patients and over time, the clinical picture changes in the direction of increasing severity. In postthrombophlebitis syndrome, symptoms usually worsen after prolonged walking or standing and improve with rest or a horizontal position of the lower limb.