What will happen in the video:
1. What are monocytes |
00:22 (in video) 2. Normal monocytes in the blood | 02:49 (in video) 3. Reasons for the increase in monocytes in the blood | 03:42 (in video) 4. Symptoms of increased monocytes in the blood | 06:58 (in video) 5. Increased monocytes in children (monocytosis in children) | 10:39 (in video) Online consultation with infectious disease specialist, allergist-immunologist Natalia Nikolaevna Gordienko
Cost of online consultation: 3500 rubles
Online consultation
During the consultation, you will be able to voice your problem, the doctor will clarify the situation, interpret the tests, answer your questions and give the necessary recommendations.
Read more about blood tests in our article
“Hematological tests: norms and interpretation of results.”
What are monocytes?
A monocyte is a representative of white blood cells. If translated from ancient Greek, then μονος is one, and κύτος is a cell. This is a fairly large cell, which has a large nucleus, slightly eccentrically displaced, and in our body it performs very important functions. To perform its tasks, the so-called janitors or orderlies, it is equipped with special devices.
This cell can have amoeboid movement, it can move independently, like an amoeba, in the liquid part of the blood, and it can have transnasal movement. those. leave its stay in the bloodstream through the thin wall of the blood vessel and, accordingly, rush into certain tissues. Performing its function as an orderly, it has such a powerful property as chemotaxis (the motor reaction of microorganisms to a chemical irritant) and can rush precisely to the sites of inflammation. There, where there are many destroyed cells, where there may be dead bacteria, viruses, dead cells of the body.
Let’s say there is a flu-like condition, and during this period there is a lot of destruction of the epithelial cells of the nasopharynx or oropharynx. And monocytes, during the flu period, will rush there and try to utilize dead cells. By enveloping fairly large pieces of destroyed bacterial cells and digesting them, they will prepare the tissue for reparative processes (recovery processes). They must clean out the field, and in this field, after eliminating the source of inflammation, young, healthy cells will then grow.
Causes of increased monocytes
Out of the blue, just like that, the number of monocytes does not increase. There are certain reasons for this. I want to tell you the main diseases and conditions in which the number of monocytes in the blood will increase.
- Of course, tuberculosis, including extrapulmonary forms of tuberculosis, will come first. It is he who will cause this monocytosis. Unfortunately, today the number of tuberculosis of the extrapulmonary form is beginning to increase widely: kidneys, intestines, skin, spine, lymph nodes, cases of tuberculosis of the lymph nodes have especially increased. In all these conditions, in any form of tuberculosis, a person will always have an increase in the number of lymphocytes.
- Syphilitic lesion. Syphilis is also a systemic disease, and it will also cause monocytosis or an increase in the number of lymphocytes.
- Autoimmune diseases. First of all, diseases of an autoimmune nature of connective tissues: systemic lupus erythematosus, rheumatoid conditions, rheumatoid arthritis, periarthritis nodosa. When immune inflammation occurs in connective tissues. In these conditions there will also be monocytosis.
- Problems of the digestive tract, in particular ulcerative colitis, inflammation of the small intestine, Crohn's disease - these are conditions when the number of lymphocytes in the blood will also increase.
- Cancerous tumors. They will also have monocytosis.
- The recovery period after any inflammatory process of infectious origin. What does it mean? Any infectious disease can cause a state of monocytosis. And if monocytosis develops in diseases not related to tuberculosis or syphilis, then an increase in monocytes will indicate that the infectious process has entered its final stage. In other words, monocytes, having activated into phagocytes, indicate that the inflammatory process is entering its final stage.
- Oddly enough - stress. They can cause monocytosis. It is stress, through a violation of psycho-emotional balance, through the pituitary-hypothalamus zone, through the adrenal systems, that can cause an increase in monocytes.
- Oncological diseases such as lymphomas or Kharchenko's disease. They can also provoke an increase in the number of lymphocytes.
Symptoms
How will a person feel, how will he feel? What should motivate a person to go and take a blood test? What symptoms might he have that could lead to an increase in monocytes in the blood?
- This could be causeless weight loss.
- Decreased or complete absence of appetite.
- Increased fatigue. Unreasonable weakness. It seemed like he had gotten enough sleep, he didn’t seem to be overtired, he seemed to be resting, but in the morning he got up and had no strength. This groundless weakness requires mandatory monitoring of blood tests.
- Anxiety, panic attacks, depression, or psycho-emotional agitation. This should also encourage a person to go and do a detailed blood test.
- Irritability, apathy, drowsiness - any disturbance in the psycho-emotional state can cause changes in the peripheral blood.
- Sudden refusal of meat food, even to the point of disgust for meat food. As a rule, monocytosis will be present in a detailed blood test.
- Gastrointestinal disorders: bloating, rapid motility, bowel dysfunction, both constipation and diarrhea, increased secretion of mucus in feces.
- A dry, prolonged cough, sometimes streaked with blood, with scanty sputum.
- Joint and muscle pain in the back and legs. This also requires decoding and examination.
- Specific rashes on the skin and mucous membranes can also be a condition in which there will be monocytosis or an increase in the concentration of monocytes in the blood.
- Presence of rashes on the genitals.
It must be said that all of the above reasons can be disturbing, both individually and collectively, together. Several symptoms unite into entire syndromes. I want to emphasize that an increase in the number of monocytes in the blood in itself is not a diagnosis. This is a state of peripheral blood cells of the immune system, which indicates that not everything is in order in the “state”, and this requires mandatory examination, requires careful attention and further decoding.
How to prepare for the test?
The level of monocytes is determined in the blood, so it is important to avoid the influence of various factors on the results.
Blood must be donated on an empty stomach after an overnight fast. For infants - half an hour before the next feeding. In children under 3 years old - 3-4 hours after eating.
The patient needs physical and emotional rest. Stress and physical activity may affect the results of the study.
Calm the child down and explain what will happen in the blood collection room. A child should not be afraid of doctors and nurses. You can reward his good behavior with some sweets or a trip to the park.
If the patient is taking any medications, it is necessary to inform the doctor about this to exclude their influence on the result.
Before giving a referral for any test, a competent specialist should advise the patient on how to properly prepare for the test.
Monocytosis in children
Separately, I want to talk about monocytosis in children. This has recently become a fairly common condition, and parents and, unfortunately, not even medical workers always know what to think about with monocytosis and what pathological causes can cause an increase in the number of monocytes in children.
- Firstly, these are diseases caused by bacteria, fungi and viruses. In principle, any of these “friends” can cause an increase in monocytes in the child’s blood.
- Infection with worms. This reason can even be put in first place in children's practice.
- Inflammatory processes in the gastrointestinal tract. And that condition of the gastrointestinal tract, which we call: intestinal dysbiosis, which is also not a diagnosis, but it is the microbiota that can determine the concentration of monocytes and cause monocytosis.
- Food poisoning. And any other poisoning can cause monocytosis in a child’s body.
- Allergic reactions in a child. If we talk about young children, then this is predominantly a genetically determined food allergy. If we talk about older children, then these may be allergic reactions associated with the same parasitosis, helminthic infestations, protozoan infections, or the consumption of food products containing a lot of preservatives, allergens, all kinds of stabilizers, etc., that is, not Completely suitable food for a child.
- Oncological diseases of the blood. Of course, they can also cause monocytosis, and, first of all, these are leukemia and lymphoma.
- Autoimmune pathology of children.
- Rheumatoid arthritis or juvenile rheumatoid arthritis.
- Systemic lupus erythematosus.
- Crohn's disease.
- Infectious processes after surgical interventions can also cause monocytosis, and this will be one of the body’s protective reactions.
If we talk about monocytosis in pediatric practice, then, of course, first of all it will be associated with acute respiratory viral infections, diseases of an infectious nature, and bacterial diseases of the gastrointestinal tract. Therefore, on the one hand, there is no need to be afraid of monocytosis, but on the other hand, this is a blood indicator that can indicate some serious, still hidden problems that are not clearly manifested clinically. And this is a reason to conduct more in-depth research on a specific person.
That’s basically all I wanted to tell you about monocytes. If you have any questions, you can write to us or ask them in the comments. And if everything is clear to you, I was glad to give you this information. Come see us if the need arises and stay healthy.
And who is to blame for the infection?
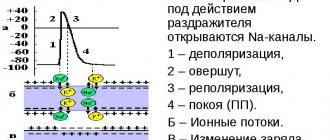
When you know which blood cells are responsible for what, using a blood test to figure out what kind of infection has attacked the child this time is not easy, but simply simple. A high ESR and high leukocytes mean that the infection is in full swing and it must be treated immediately (in addition to these indicators, there is most often a temperature above 38C). High neutrophils mean that we have met another bacteria, and high lymphocytes mean a viral infection.
Everything is simple, as you can see. Now let's look at examples. And in order not to get confused in the numbers, we will simply say “a lot” or “a little”. Shall we try?
Acute viral infection
Signs . Leukocytes and ESR are higher than normal, in the leukocyte formula there is an excess of lymphocytes, a decrease in the number of neutrophils. Monocytes and eosinophils may increase slightly.
What to do ? Most often, doctors prescribe drugs containing interferon - viferon, kipferon or genferon.
Important! The so-called intracellular parasites - chlamydia and mycoplasma - behave exactly like viruses. They can be distinguished by the clinical manifestations of the disease. The “calling card” of both is a prolonged dry cough with an extremely unclear external picture - the child looks active, there is no wheezing in the lungs. However, the cough may last for weeks.
Chronic viral infection
Signs . The child is often sick, the blood has a normal ESR and normal (or even low) leukocytes. In the leukocyte formula, lymphocytes and monocytes float at the upper limit of normal. Neutrophils are at the lower limit of normal or even lower.
What to do? Examine the child for antibodies to Epstein-Bar viruses and cytomegalovirus. Most likely, these two are to blame.
Important! If the child has just had a viral infection, the blood test will be exactly the same. So, if a child gets sick twice a year and has just suffered a viral runny nose, it is somewhat premature to run to get tested for chronic viral infections.
Advertising
Acute bacterial infection
Signs. Leukocytes and ESR are higher than normal, in the leukocyte formula there is an excess of neutrophils (or even monocytes along with them) against the background of a decrease in the number of lymphocytes. Externally, signs of inflammation are visible, such as fever, purulent nasal discharge, wheezing in the lungs or a wet cough.
What to do? The most common medical prescriptions with such a blood test are antibiotics of the penicillin group (Augmentin, Flemoklav, Solutab, Suprax), less often - antibiotics of the azalide group (Vilprofen, Sumamed).
Chronic or local bacterial infection
Signs. All the same - increased neutrophils (not higher than the upper limit of normal) and decreased lymphocytes (also within normal limits, only closer to the lower limit). If there are such changes in blood tests, you will have to look for a local, not very active source of infection (Examination by an ENT doctor or an image of the paranasal sinuses; if a urinary tract infection is suspected, a general urine test).
Important! A blood test after a recent bacterial infection looks exactly the same.