Clinical characteristics of hemorrhagic syndrome
| I. Hematoma type (disturbance of the internal coagulation pathway of coagulation hemostasis) | II. Petechial-spotted (microcirculatory) type (disturbance of the platelet link of hemostasis, external coagulation pathway of coagulation hemostasis) | III. Mixed (bruise-hematoma) type (combined disorder of both platelet and coagulation components of hemostasis) | IV.Vasculitic purpuric type (pathology of the microvascular bed) | V.Angiomatous type (local vascular pathology) |
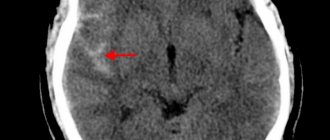
Diagnosis of ICH
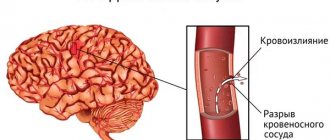
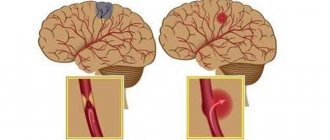
The appearance in a patient receiving NAC of a sharp headache predominantly in the occipital region, nausea, vomiting that does not bring relief, non-systemic dizziness, as well as stunned consciousness is the basis for immediately excluding the diagnosis of ICH. Symptoms of hemorrhage usually develop suddenly [3, 7, 17–19], and meningeal syndrome and low-grade fever may develop first. Already in the first hours, signs of ICH can be determined using computer or magnetic resonance imaging (MRI). A highly sensitive technique is MRI using gradient echo [1, 20, 21].
Symptoms of hemorrhagic syndrome
The nature and localization of skin rashes during hemorrhagic syndrome determine the symptoms of this pathology.
The main symptom is prolonged bleeding that occurs as a result of injury or exhausting physical activity, severe overexertion, hypothermia or overheating, which can also occur spontaneously.
In every fifth case of the pathology, a rash of a different nature is observed, both small petechiae and large necrotic hematomas may appear, and angiectasias may occur.
Hemorrhagic syndrome can result from taking medications that affect the natural processes of platelets and reduce blood clotting. In addition, patients suffering from Werlhof's disease, hemophilia and prothrombin deficiency may also experience this pathology.
What kind of disease is this
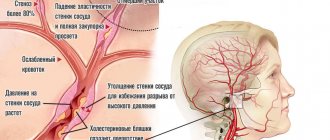
This disease is of an infectious-allergic nature: the main cause of hemorrhagic vasculitis is the presence in the blood of patients of immune complexes and active components of the protective system of proteolytic enzymes. Immune complexes accumulate in the bloodstream, and with an excessive amount of antigens or a lack of antibodies, protein formations are deposited on the endothelium of the microvascular wall. Factors contributing to the development of the disease are:
- bacterial and viral respiratory infections suffered 2-4 weeks before the onset of the disease, which account for up to 60-80% of all cases of the disease;
- foci of chronic infection (sinusitis, tonsillitis, caries, etc.);
- some medications, mainly of antibiotic action;
- potentially allergenic foods (strawberries, citrus fruits, chocolate, eggs, etc.);
- administration of a vaccine or serum;
- hypothermia and dampness or prolonged exposure to the sun.
There is evidence of a hereditary predisposition to the disease. In some cases, it is impossible to find out which factor served as the “trigger” for the patient’s body.
Types of hemorrhagic syndrome
Violation of the internal coagulation pathway of coagulation hemostasis (hematoma type of bleeding)
Congenital and acquired afibrinogenemia
Deficiencies of different types of clotting factors cause different types of diseases called hemophilia, as well as other disorders that are not specific to a specific type.
More details
Disturbance of the platelet component of hemostasis, the external coagulation pathway of coagulation hemostasis (petechial-spotted type of bleeding)
Disturbance of the platelet component of hemostasis:
Disturbance of the plasma component of hemostasis
Thrombocytopenia
A condition characterized by a decrease in platelet count below 150•109/l, which is accompanied by increased bleeding and problems with stopping bleeding.
More details
Thrombocytopathy
A disease characterized by increased bleeding due to dysfunction of platelets (blood platelets that provide the initial stage of blood clotting) when their number is normal.
More details
Deficiency of factors II,V,VII,XI
Diseases associated with impaired coagulation; in these diseases, hemorrhages occur in the joints, muscles and internal organs, both spontaneously and as a result of injury or surgery.
More details
Combined violation of the platelet and coagulation components of hemostasis (mixed (bruise-hematoma) type of bleeding)
Etiology:
- Von Willebrand's disease (coagulopathy - impaired function of factor VIII, thrombocytopathy - impaired platelet aggregation)
- DIC syndrome (consumptive coagulopathy - decrease in all coagulation factors, hypofibrinogenemia, activation and depletion of fibrinolysis, thrombocytopenia, consumption thrombocytopathy)
Hemorrhagic syndrome:
- Petechial rash, ecchymosis, bleeding from the mucous membranes (nasal, gingival), postoperative, postpartum bleeding.
Disseminated intravascular coagulation
Impaired blood clotting due to massive release of thromboplastic substances from tissues.
More details
von Willebrand disease
A hereditary blood disease characterized by the occurrence of episodic spontaneous bleeding, which is similar to bleeding in hemophilia.
More details
Pathology of the microvascular bed (vasculitis-purple type of bleeding)
Petechial bleeding with exudative-inflammatory phenomena, foci of necrosis, hematuria, arthralgia, bleeding of mucous membranes.
Vasculitis:
- infectious, immune;
- systemic;
- hemorrhagic vasculitis (Schonlein-Henoch disease).
Hemorrhagic vasculitis
Systemic aseptic inflammation of the microvasculature with predominant damage to the skin, joints, gastrointestinal tract and renal glomeruli.
More details
Angiomatous bleeding
Angiomatous bleeding
One of the forms of hereditary vascular disease, characterized by a tendency to bleeding of the mucous membranes.
More details
results
Patients were treated at the Center for Anesthesiology, Resuscitation, Intensive Care and ECMO of the Federal State Budgetary Institution State Scientific Center of the Russian Federation - Federal Medical Biophysical Center named after. A.I. Burnazyan" FMBA of Russia.
In accordance with the study inclusion and exclusion criteria, 21 patients participated in the study: VV-ECMO was performed in 16 patients, VA-ECMO in 5. The causes of respiratory dysfunction that required VV-ECMO were community-acquired pneumonia in 15 (71.4 %) patients and neurogenic pulmonary edema in 1 (3.7%) patient after aneurysmal subarachnoid hemorrhage. The cause of cardiac dysfunction that required VA-ECMO was acute myocardial infarction in 5 (23.8%) cases. The duration of ECMO ranged from 1 to 33 days (average 7.23±7.6 days). The age of the patients ranged from 23 to 84 years (mean age: 48.5±15.7 years). Length of stay in the intensive care unit (ICU) - from 1 to 47 (19±8.5) days (
table 1).
Table 1. Demographic and clinical characteristics of the examined patients
Among all recorded complications, the most common were acute renal failure - 13 (61.9%), hemorrhagic complications - 12 (57.1%) and sepsis - 10 (47.6%) cases ( Table 2).
Table 2. Complications that developed in the examined patients
The planned design of the study involved dividing the first 7 days of ECMO into 24-hour intervals, during which the development of hemorrhagic complications was recorded and each of which began with an appropriate cut of traditional clotting and viscoelastic hemostasiological parameters. 116 laboratory sections and 24-hour intervals were obtained and analyzed. For technical reasons, it was not possible to perform the full range of planned traditional clotting and viscoelastic hemostasiological parameters in all sections of laboratory data. In table 3 given
Table 3. Number of 24-hour clinical and laboratory sections analyzed, indicating the number of laboratory parameters analyzed; number of hemostasiological parameters collected.
A total of 92 cases of hemorrhagic complications were recorded. Pulmonary hemorrhage developed statistically significantly more often in 59 (64.1%) cases ( p
<0,05)
(Table 4)
.
Table 4. Localization of hemorrhagic complications during extracorporeal membrane oxygenation
Bleeding associated with ECMO more often developed in the first 5 days of this procedure (Fig. 1).
Rice. 1. Distribution of bleeding by time of occurrence. The maximum number of cases of bleeding associated with ECMO was recorded on the 2nd and 3rd days of the procedure. Clinically insignificant bleeding developed more often than clinically significant bleeding - 70 (76.1%) and 22 (23.9%) cases, respectively (Fig. 2).
Rice. 2. Distribution of bleeding according to severity.
The studied patients were divided into two groups depending on the development of bleeding: group 1 - presence of bleeding, group 2 - absence of bleeding. A comparative analysis of the studied hemostasiological parameters in patients was carried out (Table 5)
. It was found that the presence of bleeding is statistically significantly associated with a reduced level of the Quick prothrombin index and platelets, with a decrease in the MCEex-MCEfib difference. A paradoxical tendency to increase fibrinogen levels with the development of bleeding was obtained, which did not reach a statistically significant level. During bleeding, MCFex was statistically significantly lower, but the absolute values of this indicator remained within the reference values in patients of both groups.
To determine the clinical significance of the studied hemostasiological parameters in predicting the likelihood of developing hemorrhagic complications during ECMO, the sensitivity and specificity of each indicator from the number of analyzed traditional clotting tests and ROTEM indicators was calculated.
Among all analyzed traditional clotting tests (APTT, INR, prothrombin index according to Quick, AT-III, fibrinogen level and platelet content), only INR statistically significantly predicted the likelihood of bleeding. Only this parameter demonstrated an area under the curve above 0.5 during ROC analysis (Fig. 3).
Rice. 3. Sensitivity and specificity of clotting methods.
The INR, with a sensitivity of 89.6% and a specificity of 55.6%, predicted the likelihood of bleeding in a patient on ECMO over the next 24 hours (see Table 1).
rice. 3).
Other traditional clotting parameters did not show a statistically significant association with the development of ECMO-associated hemorrhagic complications (area under the curve less than 0.5), so their sensitivity and specificity are not shown in the ROC analysis plot.
Among all analyzed ROTEM parameters, statistical significance in predicting the probability of developing ECMO-associated bleeding over the next 24 hours (area under the ROC analysis curve above 0.5) was demonstrated by MCFin, CFTex (Fig. 4).
Rice. 4. Sensitivity and specificity of rotational thromboelastometry parameters. The sensitivity and specificity of MCFin are 87.6 and 53.4%, respectively, and the sensitivity and specificity of CFTex are 84.9 and 65.6%, respectively.
The sensitivity and specificity of the MCFex-MCFfib and MCEex-MCEfib indicators in predicting the likelihood of developing hemorrhagic complications associated with ECMO were calculated: for MCFex-MCFfib - 0.37 and 0.8%, respectively, for MCEex-MCFib - 0.35 and 0.79% accordingly (Fig. 5).
Rice. 5. Sensitivity and specificity of parameters MCFex—MCFfib and MCEex—MCEfib.
Diagnosis of hemorrhagic syndrome
A timely diagnosis will help a specialist prescribe effective treatment, and you will be able to make your blood vessels healthy once and for all. The diagnosis can be confirmed or refuted by passing a series of laboratory tests aimed at obtaining detailed information about the state of the blood. You will also need to conduct coagulation tests; during controversial situations, the diagnostician may perform a sternal puncture for in-depth diagnostics.
After obtaining a complete picture of the disease, determining its stage, causes and severity of hemorrhagic syndrome, treatment will be prescribed.
Treatment of hemorrhagic syndrome
The basis for choosing a treatment method for hemorrhagic syndrome is determining the cause of the disease, but there are the following key principles:
- Regardless of the cause, the patient is provided with emergency medical care to stop the bleeding. For this, vikasol, calcium chloride, vitamin C, and thromboplastin solution are used.
- If pathology occurs while taking potent medications, their discontinuation is mandatory.
- Local therapy for hemorrhages is carried out using dry thrombin, homeostatic sponges, aminomethylbenzoic acid (Amben).
- In case of heavy blood loss, transfusion of blood or its fractions may be necessary, preferably directly from the donor.
- Also, for hemorrhagic syndrome of various etiologies, serotonin preparations, for example, Dynaton, are used.
Prevention of hemorrhagic syndrome
The most important and fundamental part of the prevention of hemorrhagic syndrome is a complete medical examination for the timely identification and elimination of its possible causes.
Newborn premature babies need subcutaneous vitamin K and breastfeeding as soon as possible after birth.
The dietary nutrition of patients prone to this pathology should be based on increased consumption of vitamin K, as well as proteins, vegetables and fruits. In addition, such people need to avoid physical activity that leads to injury and injury.
You may also be interested in
Acute intestinal obstruction
A pathological condition that is characterized by a violation of the passage of the contents of the gastrointestinal tract in the direction from the stomach to the anus
More details
Intestinal paresis
Intestinal paresis is a condition that accompanies many serious diseases and is characterized by a gradual decrease in the tone of the intestinal wall and paralysis of the intestinal muscles
More details
Medical care in hospital
All patients receive intensive therapeutic care at an early stage in a neuro intensive care hospital. Initial treatment measures are aimed at:
- normalization of microcirculation, hemorheological disorders;
- relief of cerebral edema, treatment of obstructive hydrocephalus;
- correction of blood pressure, body temperature;
- functional regulation of the cardiovascular system;
- maintaining water and electrolyte balance;
- prevention of possible seizures;
- prevention of extracranial consequences of inflammatory and trophic nature (pneumonia, embolism, pulmonary edema, pyelonephritis, cachexia, DIC syndrome, endocarditis, bedsores, muscle atrophy, etc.);
- providing respiratory support (if the patient needs it);
- elimination of intracranial hypertension in HI with dislocation.
Prognosis for ICH
The higher the INR level at the time of hospitalization, the greater the likelihood of increased hematoma size, residual neurological deficit and death [3, 17, 46, 65, 66]. Death occurs in 2/3 of patients with ICH if the INR at the time of hospitalization exceeds 3 [65]. A large volume of hematoma (> 50 ml), intraventricular extension of hemorrhage, and displacement of the midline structures of the brain are also associated with a poor prognosis [3, 6, 7]. According to AY Zubkov et al. [67], prognostically unfavorable factors are a low score on the Glasgow scale (Table 4) at the time of admission and a large initial volume of the hematoma. The development of neurological deficit does not depend in any way on the INR level at admission.