Retinal hemorrhage is a visual disorder that occurs due to damage to the eye vessels. As a result of the development of pathology, bleeding occurs into the retina tissue.
Often the causes of hemorrhage are mechanical damage to the organ of vision (contusions that can occur due to a blow to the head, face, etc.); some serious diseases can also provoke the pathological process.
Root causes of hemorrhage:
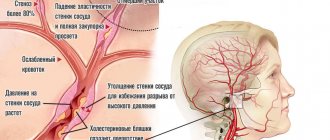
- Arterial hypertension.
- Leukemia, anemia and other blood diseases.
- Intraocular tumors.
- Diabetes.
- Inflammatory pathologies of the choroid.
- Myopia in later stages of development.
- Systemic connective tissue diseases: vasculitis, scleroderma.
- Atherosclerosis and other diseases.
Strong screaming or coughing can also cause damage to the eye vessels. Retinal hemorrhage is sometimes diagnosed in women during labor during childbirth.
Cardio training and excessively intense sports can also cause bleeding in the retina.
Signs of retinal hemorrhages
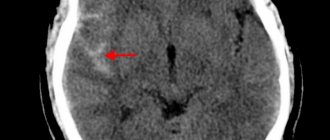
Hemorrhages can occur in any layers of the retina. The localization of pathology, as a rule, can be determined by a number of external signs. Thus, the outpouring of blood into the layer of nerve fibers looks like streaks, and into the area of the optic nerve head and macula - radial stripes. Blood in the middle layers of the retina appears as small, clearly defined circles of bright purple or red color. Preretinal hemorrhage, localized between the posterior hyaloid membrane of the vitreous body and the layer of nerve fibers, has the appearance of a large puddle (up to 4-5 diameters of the optic disc) with a horizontal level of separation of plasma and other blood elements. Subretinal hemorrhage, localized between the layers of the retinal neuroepithelium and pigment epithelium, is characterized by a darker color than retinal hemorrhage and the absence of clear contours. Choroidal hemorrhage appears as a dark red and even bluish tint. The most dangerous pathology is retrochoroidal hemorrhage, which is essentially arterial bleeding, otherwise expulsive hemorrhage.
Retinal hemorrhages usually occur in one eye, and the patient feels it by a sharp decrease in visual acuity.
Diagnostics
If retinal bleeding is suspected, our ophthalmologists conduct a comprehensive examination of the patient.
- Visual acuity test, which shows the condition of the central zone of the retina;
- Perimetry (study of lateral vision), which allows assessing the condition of the peripheral areas of the retina;
- Tonometry – measurement of intraocular pressure.
With the help of a special examination - ophthalmoscopy (with a wide pupil) we will determine the location of hemorrhages, their number, and also identify thinned areas that pose a danger in terms of the emergence of new pathological foci (changed vessels).
An ultrasound examination gives an idea of the size of the detached retina (if this occurs against the background of hemorrhage) and the condition of the vitreous body. It is especially important for opacities of the lens, cornea or vitreous body, when it is impossible to see the retina.
Optical coherence tomography (OCT) allows differentiation of ocular structures measuring a few thousandths of a millimeter (micrometers) in size. It combines the capabilities of a scanner and a microscope. With this diagnostic test, the ophthalmologist can examine in detail the condition of all layers of the retina.
Our center has a unique opportunity to perform OCT angiography (OCTA) – i.e. examine the blood flow through the vessels of the retina and identify the place of blood exit for further laser treatment.
In terms of forecasts for vision restoration, electrophysiological studies (EPS) are used: an ophthalmologist determines the viability of the optic nerve and retinal nerve cells, which determines the appropriateness of treatment (including expensive ones).
Fig.2 Retinal optical coherence tomography (OCT) procedure
Treatment
Treatment of retinal hemorrhages is carried out only in an ophthalmological hospital, where patients are required to be hospitalized.
As a conservative therapy, in the treatment of retinal hemorrhages, corticosteroids (subconjunctival injections), angioprotectors, antioxidants, non-steroidal anti-inflammatory drugs, diuretics, vasodilators and antihistamines are prescribed. Osmotherapy and laser coagulation are carried out (for large volumes).
The duration of treatment is usually 14 days, after which the hemorrhage will resolve and vision will improve.
Major retinal diseases
- Retinal angiopathy;
- retinal detachment;
- retinal dystrophy;
- diabetic retinopathy;
- retinal tear;
- retinal degeneration;
- macular degeneration and macular degeneration;
- retinitis;
- hypertensive retinopathy;
- retinal tumor;
- retinal hemorrhage.
Retinal pathologies can occur with various general and systemic diseases - hypertension, diabetes mellitus, kidney and adrenal gland diseases, as well as with eye injuries and traumatic brain injuries. Some infectious diseases (flu, etc.) can be complicated by retinal diseases.
Prevention
Retinal hemorrhages may recur. To prevent such complications, mandatory medical examination and limitation of physical activity are recommended for 2-3 months after discharge from the hospital. For diabetic patients, therapy of the underlying disease, correction of the diet, as well as working and rest conditions are necessary.
In the medical department, everyone can undergo examination using the most modern diagnostic equipment, and based on the results, receive advice from a highly qualified specialist. The clinic provides consultations to children from 4 years old. We are open seven days a week and work daily from 9 a.m. to 9 p.m. Our specialists will help identify the cause of vision loss and provide competent treatment for identified pathologies.
You can find out the cost of a particular procedure or make an appointment at the Moscow Eye Clinic by calling 8 and 8 (499) 322-36-36 (daily from 9:00 to 21:00) or using the online registration form .
Forecast
In most patients, retinal hemorrhages resolve well. Sometimes, in their place, delicate connective tissue moorings develop or mottling of the macular zone remains, as a result of which visual acuity sharply decreases. Therefore, to preserve vision, it is important to promptly contact a specialized eye clinic with doctors who know and can treat such diagnoses. We will be happy to help you - call to ask your questions and make an appointment.
You can find out the cost of basic diagnostic procedures and surgical procedures performed in our clinic in the PRICES section.
Foreign body of the conjunctiva
A foreign body of the conjunctiva (usually small particles of earth, coal, stone or metal, grains of sand, hairs of cereal plants) can remain on the surface or penetrate into it, violating the integrity of the epithelial cover, in the latter case an inflammatory infiltrate is formed.
In the clinic, symptoms of eye irritation predominate: photophobia, pain, blepharospasm and, naturally, the sensation of the presence of a foreign body. During examination or biomicroscopy, you can see a foreign body on or inside the conjunctiva.
A foreign body can move due to blinking reflex movements of the eye. Often it lingers in the groove of the eyelid, on its inner surface. Then, when the eyelid is everted, an inflammatory infiltrate with papillae in the center of which is a foreign body (hair of cereal plants, etc.) is discovered.
Often, damage to the conjunctiva leads to subconjunctival hemorrhage. This can happen due to trivial rubbing of the eye. A blood-red spot appears on the sclera. Despite the “terrible appearance,” such hemorrhage is not dangerous: it resolves on its own in two to three weeks and does not lead to visual impairment. But sometimes a perforation of the eyeball can be missed behind a bloody spot. Therefore, at the slightest suspicion, the victim should be sent for examination to an ophthalmologist.
Treatment
If it is located superficially, the foreign particle can be easily removed with a cotton swab soaked in a disinfectant solution. If penetration occurs deep into the tissues of the eye, you need to drip a solution of tetracaine (0.5%) into the eye and then remove it with a special needle or tweezers. If it is impossible to remove in this way, a section of the conjunctiva is excised along with the foreign particle.
Large fragments of coal, stone, glass, metal that cause severe irritation should be removed. And small particles of sand and stone that do not cause irritation do not need to be removed; they will “come out” on their own thanks to the blinking movements of the eye.
Injuries to the cornea of the eye
Most often, corneal injuries are caused by scratching with a fingernail or other foreign body, but more serious injuries, such as chemical burns, can also occur.
All corneal wounds are divided into linear and patchwork. They can be of various sizes and shapes. Clinical manifestations: lacrimation, photophobia, eye pain, blepharospasm. If an infection occurs, inflammatory infiltration of the wound edges can be detected.
To diagnose a non-perforated corneal wound, in addition to anamnestic and clinical data, the following method is used: drops of a fluorescein solution (1%) are instilled into the conjunctival sac, followed by rinsing with a sodium chloride solution (isotonic). The injured area of the cornea will turn yellow-green.
Treatment
Analgesics are not used for injury to the cornea of the eye, because this delays the healing process. Epithelization occurs within a few days without leaving a trace. If the damage was deep, it is possible that after healing there will be an area of cloudiness, which (sometimes) reduces visual acuity. In general, the prognosis for corneal injuries is favorable.
Foreign body in the cornea of the eye
Foreign particles can linger on the surface of the cornea or penetrate deep into the eye tissue (usually metal particles). This depends on the flight speed, the presence of sharp corners and teeth on the foreign body. Penetrating into the tissue of the eye, the foreign body disrupts the integrity and causes the development of an inflammatory infiltrate, visible upon examination in the form of a rim. A vascular pericorneal reaction appears.
The predominant symptoms in the clinic are: lacrimation, photophobia, a feeling of “mote in the eye,” blepharospasm, pain in the eye. Conjunctival injection is present. If it is impossible to remove, the foreign body of the cornea can gradually be rejected independently through demarcation inflammation. When chemicals are introduced, encystation and the development of purulent keratitis are possible.
Treatment
After pre-anesthetizing, you need to remove the foreign body from the cornea using a cotton swab soaked in boric acid (2%). For deeply located particles, a spear or grooved chisel is used. The smallest particles of coal, gunpowder, sand, and stone are often not removed unless they cause painful reactions. But bodies that can oxidize (steel, iron, copper, lead, etc.) must be removed, otherwise they will cause an inflammatory reaction with the formation of an infiltrate. Foreign bodies in the cornea can penetrate the anterior chamber of the eye, causing it to completely empty. In such cases, hospital treatment is mandatory.
The prognosis for superficially located foreign bodies of the cornea is favorable - they do not leave traces. But the extraction of foreign particles from the deep layers leads to clouding, which reduces visual acuity.
Main “risk groups”
- People with moderate and high degrees of myopia;
- pregnant women;
- elderly people with diabetes.
The initial stages of the disease may not be accompanied by any symptoms , so if you are at risk, be sure to undergo vision diagnostics using modern equipment. This examination will reliably determine whether you need treatment. If you are scheduled for surgery, do not put off surgery for too long. Before surgery, you need to protect your eye from possible damage in every possible way.
If diseases of the retina of a dystrophic nature are detected, with its thinning and rupture in the periphery, it is strengthened using a laser. Otherwise, any sufficiently strong tension can lead to detachment, requiring immediate surgical intervention. It is better to prevent such a situation. Moreover, detachment can occur when urgent provision of qualified ophthalmological care is impossible (at the dacha, on a trip, etc.)
Retinal detachment
Retinal detachment is the separation of the retina of the eye from the choroid. When the retina ruptures, the intraocular fluid penetrates under it and peels off from the choroid. If retinal detachment occurs, you should immediately consult a doctor, as delay may result in blindness.
Retinal detachment is usually treated surgically. This can be extrascleral ballooning or filling (the purpose of such treatment is to achieve adherence of the retina to the choroid), then laser coagulation and vitrectomy are performed (used to remove scars and blood from the vitreous). Surgical treatment methods usually require restriction of visual work and physical activity. Read more about the treatment of retinal detachment.