This is necessary because, in our understanding, taking pills by the handful is absolutely normal, although even today medicine has not studied all the options for drug interactions. Moreover, vitamin complexes, dietary supplements and herbs are also pharmacologically active substances and can enter into various reactions with the pills we take for the same cold, cough and other things. At best, such a “medicinal smoothie” will simply turn out to be ineffective and will “transit” through your body. Another option may be the development of adverse reactions, ranging from allergies to ulcers or gastritis.
What intervals should there be between taking pills?
When a doctor tells us to take a medicine, for example 1 tablet 2 times a day, we perceive this as 2 times a day within 16-17 hours of the time during which we are awake. Doctors mean 24 hours.
Check with your doctor about the specific time of taking the medicine prescribed to you, for example, 2 times a day, how is that? If the appointment sheet says 8:00 and 20:00 or 10:00 and 22:00 there will be no misunderstandings, the same goes for how to take pills 3 times a day or how to take pills 4 times a day.
And this is not due to the fact that it makes taking medications more inconvenient for you, but because the body works not only while we are awake, but also when we are sleeping.
Therefore, if the doctor prescribes the drug 2, 3, 4 times a day, the interval between taking the pills should be 12, 8 and 6 hours respectively, and not the time when it is convenient for us or when we remember that we need to take a pill.
Recommended Vitamins and Minerals
For morning intake, the following vitamins are recommended: C, D, and some groups C. In the evening, it is worth taking vitamin B3 and magnesium.
It is not recommended to take vitamins on an empty stomach, as this can lead to gastrointestinal upset, vomiting and diarrhea. Therefore, it is better to consume them in the morning with food.
For best results, some beneficial active substances should be consumed with food that contains enough fat. This is due to the fact that they can only dissolve in fat, so if you take such vitamins in the morning with a low-fat meal, then taking them can be considered useless. Fat-soluble active substances include:
Vitamin A
It has a positive effect on vision, the functioning of internal organs, and reproductive function. There is no exact evidence as to what time of day is best to take it, so you can do it at any convenient time.
The vitamin is present in the dietary supplement beta-carotene. Both elements are considered fat-soluble, which means they need to be taken with food that contains fat.
Vitamin B
Improves the functioning of the entire body and maintains its health for a long time. If there is a lack of certain B vitamins in the body, then fatigue is noted. A lack of clarity can also be caused by unclear consciousness. Some vitamins in this group may interfere with restful sleep. For example:
- AT 6. You may have vivid and colorful dreams. Improves memory of dreams. It is advised to take these vitamins in the morning;
- AT 12. Promotes energy production, which leads to insomnia, so they should also be taken in the morning.
For some diseases, doctors prescribe consumption of excessive amounts of vitamin B12, which reduces sleep duration. But if you take B12 in combination with other vitamins in this group, then problems with sleep should not arise.
Vitamin B3, on the contrary, improves sleep and helps you fall asleep faster. Anecdotal evidence suggests that taking an excessive dose allows people to fall asleep quickly and stay asleep. But it should not be taken with alcoholic drinks, since the effect of the vitamin can increase several times.
Vitamin C
Strengthens the immune system. Protects cells from the negative effects of free radicals. The vitamin is water soluble, so it does not need to be taken with food. Some people, due to the consumption of excessive amounts of the vitamin, experience disturbances in stomach acidity and may experience gastrointestinal upset. If taken with food, adverse reactions can be avoided.
According to research, it is best to take the vitamin before 3 pm.
Vitamin D
This vitamin has a large number of functions that it performs in the body. It strengthens the immune system, together with calcium, strengthens bones, and has a positive effect on the functioning of the nervous system. Natural production of vitamins occurs when the skin is exposed to sunlight. But it is better not to overuse this, since prolonged exposure to the sun can lead to burns and skin cancer.
The vitamin is fat-soluble, so it is taken with food. Can be taken at any time of the day.
Vitamin E
Prevents cell damage, improves the functioning of the immune system, dilates blood vessels. Should be taken with food containing fats at any time of the day.
Vitamin K
Thickens the blood. Takes part in building strong bones. Prevents the appearance of cancer cells, helps with diabetes. The fat-soluble vitamin is taken with food at any time of the day.
Calcium
Strengthens bones. Many people are deficient in this vitamin. From the age of 4 years, a person should receive 1100-1350 mg of calcium daily. Calcium citrate can be taken alone or with food. Calcium carbonate begins to work together with stomach acid, so it must be taken with food.
Magnesium
Helps improve the functioning of the nervous system, maintains blood pressure at the desired level, strengthens bones. Usually the required amount of the mineral comes with food. A lack of magnesium can manifest itself as vomiting, lack of appetite, lethargy, and fatigue.
Irregularity in taking medications
Medicines should be taken regularly to ensure an effective amount is maintained in the body at all times. When medications are taken haphazardly, without following a protocol, their blood levels may become too low to effectively fight the disease, such as stopping the virus from multiplying. This gives the virus a chance to mutate and become resistant to the drug. How to take medications correctly, what interval should be between taking pills and the exact time to take medications should be prescribed to you by your doctor.
MORNING DAY
Coenzyme Q10 Promotes energy processes in cells, delays the aging of the body, improves the body's protective abilities, i.e. immunity, and increases physical endurance. It is found in almost all cells, most of all in organs that require a lot of energy to function - in the heart, brain, liver, kidneys. CoQ10 is better absorbed when taken with dietary fat, ideally with breakfast or lunch, to avoid negative effects on sleep.
Zinc Zinc contributes to the normal functioning of the immune system, fertility and the reproductive system. Zinc is an important mineral. It is found in large quantities in foods rich in protein - fish, seafood, nuts, seeds. Take zinc during the day with food, as it can cause nausea if taken on an empty stomach. Do not take it at the same time as calcium or iron.
Iodine Iodine takes care of the synthesis of thyroid hormones and skin health. Iodine does not accumulate in the body, so it must be taken regularly. Iodine is a trace element that occurs naturally in or added to food. The richest sources of iodine are seaweed, shrimp, cod liver and milk. Research has found that iodine increases energy, so take it after lunch to boost your energy levels.
Taking antihypertensive drugs before bed is better at reducing cardiovascular risk
Goals
To test whether taking antihypertensive medications at bedtime provides a greater reduction in cardiovascular risk compared with waking up.
Introduction
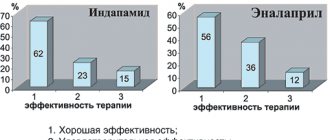
Data from many prospective clinical studies indicate improvements in blood pressure (BP) during sleep and the formation of a more physiological pattern of diurnal blood pressure fluctuations (dipping) when medications for the treatment of hypertension are taken before bedtime rather than upon awakening. Side effects do not increase. Such differences are due to the influence of circadian rhythms both on the pharmacokinetics and pharmacodynamics of medications, and on the mechanisms of blood pressure regulation. For example, the peak activity of the renin-angiotensin-aldosterone system (RAAS) occurs during sleep. Accordingly, a single dose of drugs that block angiotensin-II receptors and ACE inhibitors before bedtime, as well as combinations of these drugs with calcium channel blockers and diuretics, leads to a significantly greater reduction in blood pressure during sleep without reducing the therapeutic effect during the day.
Controlling blood pressure during sleep through proper timing of medications is clinically important. Results from numerous independent prospective studies and meta-analyses indicate that mean sleep BP measured by ambulatory BP monitoring is a significantly more accurate predictor of cardiovascular risk than daytime measurements, ambulatory BP monitoring, or 24-hour mean BP. The most important results from studies involving periodic assessment of BP during follow-up support the therapeutic effect of lowering mean systolic BP (SBP) during sleep. The emergence of a physiological pattern of diurnal blood pressure fluctuations (dipping) reduces the risk of cardiovascular disease, regardless of treatment-induced changes in blood pressure measured in the doctor's office and/or while awake.
Despite growing evidence of the effect of timing of hypertension medications on BP, particularly during sleep, studies examining long-term effects, including the Heart Outcomes Prevention Evaluation (HOPE), specifically assessed the effect of taking antihypertensive medications in the evening/before bed on reducing the risk of cardiovascular events. vascular diseases. However, these studies were not compared with morning dosing.
The Monitorización Ambulatoria para Predicción de Eventos Cardiovasculares (MAPEC—Ambulatory Blood Pressure Monitoring to Predict Cardiovascular Risk) study is the first currently known prospective randomized trial specifically designed to test whether BP and the risk of cardiovascular events improve with regularly taking antihypertensive medications before bed, compared with taking them after waking up. After a median follow-up of 5.6 years, there was a significant reduction in sleep BP and a lower incidence of cardiovascular disease. These data, based on a relatively small group of 2156 patients with hypertension, await confirmation in a primary care clinical setting.
Project Hygia is a research network designed to make ambulatory blood pressure monitoring a routine diagnostic procedure to determine what plays a role in hypertension treatment, response to treatment, and cardiovascular risk.
Methods and results
In this multicenter, controlled, prospective study, 19,084 patients with hypertension (10,614 men/8470 women, age 60.5 ± 13.7 years) were assigned (1:1) to take ≥1 daily dose of hypertension medications at bedtime (n = 9552 ) or take medications upon awakening (n = 9532). At each scheduled clinic visit (at least once a year) throughout the observation period, ambulatory blood pressure monitoring was performed for 48 hours. During 6.3 years of follow-up, 1752 participants had a primary CVD outcome (CVD death, myocardial infarction, coronary revascularization, heart failure, or stroke). Patients who took the medication before bed compared with those who took the medication after waking up had a significantly lower risk ratio—adjusted for age, sex, type 2 diabetes, chronic kidney disease, smoking, HDL cholesterol, and sleep systolic blood pressure , the relative reduction in systolic blood pressure during sleep and previous cardiovascular events—the primary CVD outcome [0.55 (95% confidence interval (CI) 0.50–0.61), P <0.001] and each of its individual components ( P <0.001 in all cases), i.e., cardiovascular death [0.44 (0.34–0.56)], myocardial infarction [0.66 (0.52–0.84)], coronary revascularization [0.60 (0.47–0.75)], heart failure [0.58 (0.49–0.70)], and stroke [0.51 (0.41–0.63)].
Conclusion
If patients with hypertension who are prescribed ≥1 antihypertensive drugs regularly take them before bedtime, and not after waking up, the condition improves: there is a more pronounced decrease in blood pressure during sleep (dipping). In most cases, the number of major cardiovascular complications is significantly reduced. .
Figure 1. Kaplan-Meier cumulative hazard curves for cardiovascular disease outcomes by medication regimen (after awakening or before sleep).
(A) Cardiovascular disease outcome: total mortality from cardiovascular disease, myocardial infarction, coronary revascularization, heart failure, and stroke; log series test: 140.1, P < 0.001. (B) Total incidence of cardiovascular disease: total mortality from cardiovascular disease, myocardial infarction, coronary revascularization, heart failure, stroke, angina, peripheral arterial disease, and transient ischemic attack; log series test: 174.0, P < 0.001.