Thrombophlebitis (TF) is an inflammatory process that affects the wall of venous vessels, resulting in the formation of blood clots. Depending on the stage of development, several types of the disease are distinguished.
Signs of the development of pathology are an increase in body temperature, redness and thickening in the area of the affected vein, pain, etc. These symptoms should be the reason for mandatory contact with a specialist who will conduct an examination and identify the cause of these symptoms.
Medical offers its clients high-quality and professional assistance from a phlebologist in the diagnosis, treatment and prevention of vein diseases, including varicose veins. In the clinic, equipped with modern equipment and equipment, you can receive high-quality services from experienced doctors at reasonable prices.
What is venous thrombophlebitis?
The disease is an inflammatory process that takes place in the venous wall, and is accompanied by the formation of blood clots (thrombi), which have different densities and close the lumen of the vein. As a result, partial or complete blockage of blood vessels occurs.
The pathology has an acute and chronic form, and can occur in superficial and deep veins. TF is most often diagnosed in the lower extremities, but it can also affect the venous vessels of any other parts of the body. If therapy is not carried out correctly and on time, it can cause undesirable consequences, including:
- purulent abscess;
- blood clot separation;
- blood poisoning.
Thrombophlebitis of the superficial veins has more severe symptoms compared to the disease affecting the deep veins. However, in both cases, timely diagnosis is very important, which will allow you to begin treatment without wasting time, and thereby avoid worsening the situation.
Varieties
Thrombophlebitis is classified into types according to various criteria. First of all, a deep and superficial pathological process is distinguished. This depends on the depth of the inflamed vein. It is important to classify thrombophlebitis according to its duration:
- The acute form is characterized by pronounced symptoms. Symptoms may last from several days to a month. Against the background of exacerbation, the risks of developing complications increase significantly.
- The chronic form is characterized by cyclicity with periods of exacerbation and completely asymptomatic remission. The symptoms of the pathology are not pronounced and, most often, are manifested by pain under increased loads.
Types of thrombophlebitis of the lower extremities
Depending on the affected area, the following types of thrombophlebitis of the lower extremities are distinguished:
- TF of the superficial veins begins with the appearance of mild pain in the skin located along the saphenous veins. The skin changes its hue to red and becomes inflamed, its temperature rises. Also, in some cases, there is a slight increase in the temperature of the whole body, which remains elevated for about 6 days. Symptoms of this type of pathology include swelling of the limb in which a blood clot has formed. Condensed areas of various sizes may appear on it, which can be easily palpated. Painful sensations appear while walking.
- Deep vein TF, manifestations of which occur only when the blood clot enlarges. If a blood clot breaks off, chest pain, shortness of breath, and expectoration of blood occur. The development of pathology is indicated by swelling, pain during movement, and a change in the shade of the skin to bluish.
The severity of the disease is determined by the size of the filling and its location in the body. Symptoms are completely absent if there is no blockage of the vessel. This makes it much more difficult to identify the problem in a timely manner.
Septic thrombophlebitis of veins is also distinguished. It occurs due to purulent melting of a blood clot and transmission of infection through the bloodstream.
Based on characteristics such as the location of the affected area, TFs are distinguished:
- upper and lower extremities;
- vessels of internal organs.
Pathogenesis of the disease
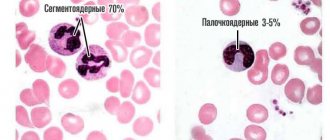
Thrombophlebitis and phlebothrombosis develop according to a simple pattern. First, there is a sharp decrease in blood flow, then the damaged vascular endothelium provokes the release of interleukins (they are responsible for platelet aggregation), while simultaneously increasing their adhesiveness. As a result, blood clots form - pathological blood clots that attach to the walls of veins, arteries and even in the cavity of the heart.
Depending on the type of blood clots, thrombosis is distinguished:
- Parietal - a blood clot is attached to the wall of the vessel, but most of the lumen is preserved. This phenomenon is typical not only for thrombophlebitis, but also for some other diseases (aneurysm of the heart, blood vessels, chronic heart failure, etc.). In the case of mural thrombosis, one part of the thrombus is attached to the wall of the vein, and the other hangs freely into the lumen. With an increase in the speed of blood flow, small oscillatory movements, or awkward getting out of bed, such a clot can break off and provoke a pulmonary embolism.
- Obstructive (occlusive) - complete closure of the lumen by a thrombus is noted, as a result of which blood stops circulating through the affected area of the vein or artery. In this case, the patient must be treated urgently, as there is a risk of gangrene or death.
The thrombus-forming process can progress and lead to the enlargement of veins to impressive sizes. The location of the thrombus occurs along the length of the bloodstream. In the first few days, the clot is weakly fixed on the surface of the vessel. On days 5-6, it becomes more securely attached to the inner wall, which is why it begins to become inflamed.
Within 6 months, 70% of patients experienced an improvement in venous patency. In other cases, damage occurs to the vessels supplying the vein wall. This process is accompanied by gross fibrinous changes in the walls and disruption of the venous valves. As a result of the pathological process, there is a significant increase in pressure in the veins of the lower leg, and the general clinical picture is accompanied by the development of chronic venous insufficiency.
Reasons for education
Blood clots stick together much faster in the area where the pathological lesion occurred. This provokes a more rapid narrowing of the lumen and disruption of tissue nutrition. Key factors contributing to the development of the disease include:
- excess weight;
- lower limb injuries;
- varicose veins;
- incorrectly administered injection;
- the presence of tumors in the digestive system;
- low level of physical activity;
- previous operations;
- pregnancy;
- prolonged stay in an uncomfortable position;
- alcohol abuse and smoking;
- hormonal treatment and contraception;
- autoimmune processes.
Women are at higher risk of developing the disease due to high estrogen levels. It has also been proven that COVID-19 in 70% of cases causes an overreaction of the immune system, which causes a large number of blood clots to form.
Why does the disease occur?
Often the pathological process is triggered by the presence of several factors, which are called “Virchow’s Triad”:
- increased blood clotting (indicator significantly exceeds the norm) - the result of an excess/lack of blood clotting inhibitors, a protein with anticoagulant properties;
- poor condition of the walls of the vascular system (the structure at the cellular level is disrupted);
- phenomena of stagnation, accompanied by a slowdown in blood flow.
The etiology of thrombophlebitis also often involves:
- narrowing/expansion of blood vessels in the area of varicose nodes;
- slowdown of metabolic processes;
- dysfunction of hematopoiesis.
The listed pathological changes in the body, which cause vascular thrombophlebitis, do not arise out of nowhere. The etiology of phlebitis may be associated with:
- excess body weight;
- genetic predisposition to varicose veins, phlebothrombosis;
- sedentary lifestyle;
- dehydration and insufficient fluid intake;
- treatment with medications that negatively affect blood clotting;
- pregnancy, childbirth;
- nicotine addiction;
- injuries of the lower extremities;
- cardiovascular diseases;
- surgical intervention not only on the lower extremities, but also in the peritoneum and pelvic organs;
- age-related changes in the walls of blood vessels (elasticity decreases, blood viscosity increases);
- infectious and purulent-septic infectious processes;
- hypothermia;
- allergies;
- acquired problems with blood clotting;
- malignant tumors.
Also, the risk of developing phlebitis increases if there is information in the medical record about a heart attack, stroke, large blood loss and complications of the postpartum period. The risk group includes people who lead a sedentary lifestyle, suffer from arterial hypertension or have a weakened immune system.
Symptoms and signs of thrombophlebitis
Symptomatic signs of TF vary depending on the form of its course. In the case of acute pathology, its symptoms appear within the first two weeks. The subacute form is characterized by the manifestation of symptoms within a month.
If we are talking about TF of the superficial veins, then its signs are painful sensations when palpated, redness of the skin in the affected area, and the appearance of a clear venous pattern. TF of the deep veins is characterized by swelling. Symptoms also include:
- difference in temperature between healthy and affected areas;
- pain that increases with exercise;
- tissue tension;
- chills, etc.
Among the symptoms of the disease, there are also those that can only be detected during medical diagnosis. This:
- decreased blood circulation rate;
- thickening of vascular walls;
- occlusion;
- valve dysfunction;
- increased blood viscosity.
Thrombophlebitis, the symptoms of which are described above, requires urgent medical intervention if the swelling and pain are pronounced, and there is also fever or shortness of breath, accompanied by coughing attacks and spasms in the chest. These symptoms indicate an increased risk of blood clots breaking off and subsequently entering the lungs, which will lead to death.
Folk remedies
Along with drug treatment, traditional methods can give good results. However, you should not blindly believe and thoughtlessly try everything on yourself. The doctor should control the treatment regimen, the admissibility and effectiveness of folk remedies.
- White cabbage. Cabbage leaves need to be softened, one side greased with oil and secured with a bandage on the painful area. Leave the compress on all night.
- Kalanchoe pinnate. Grind the leaves and fill the jar halfway with them. Fill the rest of the jar with vodka. Next, leave for 7 days in a dark place, shaking the contents periodically. Strain the finished tincture. Rub the sore leg from the foot to the groin in the direction of the vein. So for a month 2 rubles/day.
- Apple vinegar. Mix 2 teaspoons of vinegar and honey in a glass of water. Drink half a glass before meals 2 times a day.
- Mumiyo. You can make a tincture for internal use and ointment:
- for the tincture you need to mix 10g of mumiyo with 0.5l of water - drink 1 tablespoon/1 ruble per day, 10 days
- For the ointment, you need to mix mumiyo with Vaseline (or peach oil) in a ratio of 1 to 5 - smear 3 times a day, leave for 1 hour, 10 days.
Diagnostics
To diagnose the disease, you should contact a qualified specialist. He will conduct an examination and prescribe additional measures to study the patient’s condition, including:
- Ultrasound;
- phleboscintigraphy;
- angiography;
- phlebography.
Any experienced phlebologist will suspect TF already during a visual examination, during which he will detect dense and painful nodes located under the skin of a red tint. However, to accurately confirm the diagnosis, an ultrasound examination of the veins in the legs should be performed. This method will allow the doctor to examine thrombotic masses in the lumen of the vein and assess the degree and nature of thrombosis.
After examining the patient, the phlebologist receives data that will help him prescribe appropriate therapy. Yuzhny MC specialists conduct research using modern equipment from trusted manufacturers, which, combined with their qualifications, allows them to accurately identify the disease and begin its treatment.
Which doctor should I contact?
If there are clear signs of the development of TF or other vascular diseases (varicose veins, gangrene, thrombosis, tropical ulcers, etc.), you should consult a phlebologist. His competence includes examining the patient in order to make a diagnosis and subsequently prescribe treatment. You can also contact a specialist in this profile to receive clarification on preventive measures.
You can make an appointment with a phlebologist at a medical clinic, where experienced specialists work who have confirmed their qualifications with many years of successful experience in identifying and eliminating diseases of the venous system. The clinic is equipped with the latest technology, which allows diagnosis and treatment to be made even more efficiently and quickly.
Treatment of thrombophlebitis
The treatment regimen for thrombophlebitis is determined by the doctor based on the results of the patient’s examination and the stage of development of the disease. Today, both conservative treatment and surgical intervention are used to combat pathology. Only the attending physician has the authority to prescribe a particular therapeutic method.
At the present stage of development of medicine, pathology therapy does not necessarily involve a complex surgical operation. In some cases, it is possible to treat a person on an outpatient basis by taking medications prescribed by a phlebologist. At the same time, it is important to avoid any amateur activity in prescribing drugs in order to avoid aggravation of symptoms.
Some patients may be advised to wear compression stockings and elastic bandages if their general condition allows it. Drug treatment sometimes includes anticoagulants and anti-inflammatory drugs.
Operation
Surgery for TF is indicated in the following cases:
- the presence of signs of disease in the proximal part of the veins;
- combination of pathology with damage to the superficial vascular network;
- localization of the disease in the distal part of the vessels (does not require urgent surgical intervention, a planned operation is performed);
- thrombophlebitis of the deep veins of the lower extremities. In this case, the operation is prescribed taking into account the characteristics of the individual’s body.
In modern surgical practice, several types of operations are used to eliminate TF. Despite their differences, each type guarantees a good result. Popular techniques include:
- Crossectomy. During this type of operation, pathological areas of blood vessels are crossed in the area of the saphenofemoral junction.
- Stitching of the vena cava of the lower limb, which is carried out to narrow its lumen. This will not interfere with normal blood circulation, but will prevent it from carrying a large clot.
- Installation of a vena cava filter in the vein that supplies the leg. It is a design whose purpose is to retain large blood clots in order to prevent them from entering the general bloodstream.
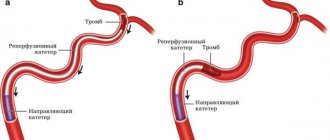
- Endovascular method of catheter thrombectomy. It is carried out to completely remove clots from the lumen of deep veins and regenerate their patency. This leads to improved blood circulation and a reduced risk of progression of pulmonary embolism.
Laser treatment
The disease has been successfully treated for many years using laser. This technique, which allows you to relieve inflammation, pain and swelling, is carried out a day or two after the exacerbation subsides and is one of the most common today.
Laser treatment of the disease involves inserting a special device into a vein. It produces a temperature effect that leads to sealing of the damaged vein and stops the process of formation of blood clots in it. The main advantage of the manipulation is that it can be performed on an outpatient basis and there is no need to make surgical incisions on the skin.
Conservative
Conservative therapy for TF can only alleviate the symptoms of the disease. However, it is not effective in completely eliminating the threat of dangerous complications due to its inability to radically solve the problem.
This treatment includes:
- Consumption of non-steroidal medications that have an anti-inflammatory effect and relieve pain.
- Mandatory elastic compression. It is recommended to choose stockings over bandages.
- Local therapy, which includes ointments and creams containing non-steroidal anti-inflammatory components.
- Anticoagulant treatment involves taking medications that thin the blood and reduce inflammation.
Physiotherapy
Thrombophlebitis, after the removal of the acute inflammatory process, is also subject to treatment with physiotherapeutic techniques. Physiotherapy as a method of combating thrombophlebitis is prescribed for the purpose of:
- suppression of blood clotting;
- slowing down the development of the process of sclerosis of veins;
- eliminate inflammation;
- hemodynamic regeneration;
- reducing pain.
The main physiotherapeutic techniques include:
- UHF treatment;
- infrared laser therapy;
- CHUV irradiation with erythemal doses;
- high-frequency magnetic therapy;
- electrophoresis with the use of medications that have an anti-inflammatory effect;
- applications of paraffin and ozokerite.
Contraindications to physiotherapy in the treatment of acute thrombophlebitis are:
- The patient's body temperature rises above 38 degrees.
- Purulent processes in the body.
- Ischemic thrombophlebitis.
In order to exclude the possibility of developing thromboembolism, it is prohibited to use TF in therapy:
- Magnetotherapy with a “running” magnetic field.
- Vibration therapy.
- Low frequency electrotherapy.
- Pulsed magnetic therapy.
Vaccinations
People with acute TF should refrain from vaccination against coronavirus infection. If at the time of vaccination a person does not have an exacerbation of the chronic form of the disease, then there is no need to fear the formation of blood clots under the influence of vaccination.
It is worth considering that infection with COVID-19 increases the risk of blood clots and an extremely undesirable outcome. In this regard, patients suffering from TF are recommended to undergo vaccination against coronavirus.
Today, there are rare cases of complications occurring after vaccination in the form of blood clots. However, both domestic and foreign recommendations for the use of vaccines do not include a tendency to blood clots among the contraindications. Therefore, it is appropriate to say that the risks of contracting COVID-19 are much higher than the rare complications that arise during the post-vaccination period.
Traditional methods
Treatment of the disease with folk remedies should be auxiliary in nature and used only with the approval of the attending physician. It can give positive results only at the initial stage of development of the pathology, but it is not effective in its advanced form. Folk remedies are indicated to prevent the development and possible complications of TF.
Discussion of traditional methods of treatment with a doctor is mandatory if a person does not want to worsen the situation. The fact is that some alternative medicine recipes include plants that stimulate the functioning of the adrenal glands and are contraindicated in patients suffering from hypertension.
Clinical forms of deep vein thrombosis
Vein thrombosis of the leg
Complaints of swelling of the foot, pain and tension in the calves, pain when pressing on the calf muscles. If thrombosis does not spread, it is almost asymptomatic. Sometimes there is thromboembolism of small branches of the pulmonary artery with cough and the development of pneumonia (pneumonia). Treatment of thrombosis of the veins of the leg can be carried out on an outpatient basis, under the supervision of a phlebologist with control ultrasound examinations.
Thrombosis of the popliteal vein
Has a clear clinical picture. Severe swelling and tension of the lower leg, swollen saphenous veins, severe pain when walking. Thrombosis of the popliteal vein is very dangerous due to frequent pulmonary embolism, so treatment is best carried out in a vascular hospital. Most often, conservative therapy is carried out with antithrombotic drugs (heparin). If the patient had thromboembolism, then urgent surgical treatment is necessary - ligation of the femoral vein above the thrombus.
Thrombosis of the iliofemoral segment (ileofemoral phlebothrombosis)
It is characterized by a severe general condition, pronounced swelling of the entire lower limb, and severe pain. The saphenous veins are sharply dilated, the leg takes on a bluish color. With ascending deep venous thrombosis, thrombosis of the entire venous bed is possible with a block of venous outflow and the development of venous gangrene (blue phlegmasia), which is accompanied by high mortality. Pulmonary embolism often occurs with a fatal outcome. Treatment of ileofemoral phlebothrombosis is only in a hospital. For occlusive thrombosis, conservative treatment is possible, but it is better to remove the thrombus so that post-thrombotic disease does not develop. In case of floating thrombosis, urgent removal of the thrombus (thrombectomy) is necessary, possibly using innovative methods. A vena cava filter can be installed in cancer patients.
Thrombosis of the inferior vena cava
The most dangerous disease. Clinically, it manifests itself as a severe general condition, swelling of both legs. Kidney failure and blood in the urine often develop. With thrombosis of the hepatic segment, liver failure develops resulting in Bud-Chiari syndrome. Treatment of acute thrombosis of the inferior vena cava should be active. It is necessary to remove thrombotic masses, as surviving patients may develop severe inferior vena cava syndrome. For this, it is good to use our innovative methods and systemic thrombolysis. The effectiveness of this treatment is very high.
Who is at risk?
The risk group for developing the disease includes the following categories:
- Pregnant women, women after childbirth and on hormone replacement therapy.
- Patients with a malignant tumor.
- Women who have been using contraceptives for a long time.
- Patients with excessively limited physical activity.
- Patients with pathologies of the venous system.
The likelihood of developing the disease is also high for people:
- Over the age of 60.
- With a previous stroke and episodes of TF.
- Smoking abusers.
- Suffering from obesity.
It is worth remembering that regular physical activity and giving up bad habits stimulate normal blood circulation, which will avoid the formation of blood clots. People who are included in one of the above risk groups should contact a phlebologist for an examination and recommendations for preventive measures.
Risk factors for the development of thrombophlebitis
- pregnancy, childbirth, gynecological operations (including abortions).
- varicose veins;
- prolonged bed rest (for example, after surgical and orthopedic operations);
- infectious diseases;
- stroke leading to paralysis of the limbs;
- motionless body position during a long trip by car or plane;
- obesity;
- oncological diseases (including surgical treatment of malignant neoplasms, radiation therapy and chemotherapy);
- dehydration;
- the use of hormonal contraceptives and other sex hormone preparations for the purpose of replacement therapy;
- increased blood clotting (hyperhomocysteinemia, antiphospholipid syndrome, etc.);
- puncture and/or venous catheterization.
The more risk factors a patient has, the higher the risk of developing thrombophlebitis.
If you have one or more factors from the above list, consult a specialist about methods of preventing venous thrombosis.
Complications of thrombophlebitis
Thrombophlebitis, the treatment of which is ignored or carried out incorrectly, can cause a number of complications. If we are talking about pathological damage to the superficial veins, then serious complications are rare. But they cannot be ignored because of the damage they can cause to health:
- Sepsis.
- Streptococcal lymphangitis.
- Spread of infection in the subcutaneous tissue.
- Change in skin color over the affected vessel.
- Thromboemolia of the pulmonary artery.
- Deep vein thrombosis.
The situation is more serious with the development of deep vein disease. In this case, the following complications are possible:
- Stroke or heart attack for patients with congenital heart disease.
- Pulmonary embolism. Part of the blood clot that breaks off in a deep vein is carried by the bloodstream to the lungs. It can block arteries and cause a situation that is extremely life-threatening.
- Blockage of veins by blood clots, resulting in a complete blockage of blood flow in the vein.
Diet
People suffering from TF or at risk of developing this disease should eat as little as possible foods containing vitamin K, which stimulates blood clotting. These products include:
- Bananas;
- Cabbage;
- Pork liver;
- Black currant;
- Soy;
- Beans, etc.
You should also be careful about foods that are involved in the formation of blood clots:
- Confectionery and baked goods.
- Fat meat.
- Canned food.
- Sausages.
- Walnuts.
It is recommended to limit the consumption of salt, sugar, sour cream and butter, and include more plant foods in the diet, including herbs, fresh fruits and vegetables, and grains. Consumption of lean meat and seafood is allowed.
People suffering from TF should eat beef liver, which strengthens the walls of blood vessels, as well as buckwheat, melon, oatmeal, cinnamon, ginger, onions, citrus fruits, dairy products, etc. It is best to steam, or boil or stew foods. Fried, salted and smoked foods are excluded. The daily volume of fluid consumed should not be less than 2.5 liters, not counting strong tea, carbonated drinks and coffee.
Prevention of thrombophlebitis
If you have questions about how to treat thrombophlebitis and what measures to prevent it, you should contact a competent phlebologist. He will give precise recommendations regarding activities that will reduce the likelihood of developing the disease. People with two or more risk factors should definitely see a specialist. Prevention, carried out in time, will help eliminate the inflammatory process and the formation of blood clots in the veins. Prevention of the disease is also carried out to prevent its complications. Preventive measures include:
- Massage.
- Healthy lifestyle.
- Proper nutrition.
- Choosing the right clothes and shoes.
- Taking care of hygiene.
- Constant physical activity.
- Timely elimination of colds and infections.
Walking, swimming, cycling and dancing will have a positive effect on your health. Hardening procedures will help strengthen the walls of blood vessels.
Why is it important to undergo treatment in a modern clinic?
Thrombophlebitis can be easily cured without surgery if the patient does not delay going to the doctor and does not self-medicate at home. This is why it is important to see a doctor at the first symptoms. The causes of the disease - inflammation of the vessel wall and blood clotting disorders - can only be eliminated through professional medical care provided by experienced doctors in a modern clinic. Not to mention acute forms of the disease, treatment of which is carried out only on an outpatient basis, since there is a risk of a threat to life.
What can be done for thrombophlebitis?
For patients with thrombophlebitis of the legs, regular moderate physical activity is recommended, as well as wearing compression stockings during the day on an ongoing basis. Daily walking in comfortable shoes will also help improve the condition of a person suffering from TF. Physical activity is allowed, but the degree of its intensity must be determined together with the attending physician based on the stage of development and type of pathology, as well as the individual characteristics of the patient’s body.
What is prohibited for thrombophlebitis?
If a person develops a disease, he is strictly prohibited from:
- Wear uncomfortable high-heeled shoes.
- Lift heavy objects.
- Engage in sports that involve intense stress on the limbs.
TF of deep veins is a restriction for visiting saunas, drinking bowls and baths. This is due to the fact that high temperatures significantly accelerate blood circulation, which has an extremely negative effect on the course of the disease.
It is strictly forbidden to gain extra pounds, and therefore a person must pay special attention to proper nutrition. Animal fats, which can be replaced with vegetable oils, should be excluded from the diet. The amount of salt consumed should be kept to a minimum in order to eliminate swelling. Quitting alcohol and smoking is mandatory for TF.
The difference between thrombophlebitis and varicose veins
TF and varicose veins have similar symptoms. However, their nature is different. In the case of varicose veins, the vessels are dilated and their walls are thinned. The result is impaired blood flow and the formation of nodes. In the case of thrombophlebitis, inflammation of the venous walls and thrombus formation occurs. The thrombus clogs the lumen of the vessel, which leads to disruption of blood flow and swelling of the affected vessel.
The key difference between the diseases lies in the pathological mechanisms underlying each of them. Disruption of the functions of the valvular venous apparatus and excessive expansion of their lumen occurs as a consequence of destructive changes in the vessels formed under the influence of harmful factors. But the pathology occurs only with impaired blood circulation in the venous line and trophism of the soft tissues located around the affected vessel. A complication of varicose veins that cannot be treated is thrombophlebitis.