Venectomy: what is it?
One of the most common vascular operations is venectomy - removal of superficial veins in the legs with redirection of blood outflow into the deep main vessels. The procedure is prescribed for advanced varicose veins.
Venectomy is a low-traumatic operation and is easily tolerated by patients. However, this is a rather radical method, which is prescribed when absolutely necessary.
Contraindications for venectomy are:
- infectious and inflammatory processes in the legs;
- deep vein thrombosis;
- pregnancy, breastfeeding period.
There are quite a few methods of venectomy in modern surgery: according to Babcock, Narat, Troyanov-Trendelenburg. The method of performing the operation is selected individually, based on the patient’s indications and complaints. Regardless of the technique, the procedure is performed in stages:
- Ligation of the great saphenous vein.
- Excision of the problematic vessel through a small incision in the groin area.
- Removal of a pathological vein using a vein extractor probe.
- Treatment of perforated veins.
Venectomy can be complemented by other therapeutic techniques by introducing sclerosants.
Why is miniphlebectomy necessary?
With this procedure you can get rid of virtually any varicose veins.
And in some cases, even remove the trunk of the GSV (great saphenous vein) on the lower leg and eliminate the altered areas of the SSV (small saphenous vein). As an independent operation, miniphlebectomy allows you to get rid of varicose veins affected by the tributaries of the saphenous main veins in the absence of both horizontal and vertical reflux. But if one occurs, then phlebectomy is first used. This combination has an excellent cosmetic effect.
Endovascular laser ablation
EVLT is a modern method of combating varicose veins using a laser. The operation is low-traumatic and therefore absolutely painless. EVLT is prescribed for:
- elimination of cosmetic defects in the form of varicose veins;
- elimination of pathological symptoms;
- preventing lymphovenous stagnation;
- prevention of complications (thrombosis, trophic skin defects, ulcers, pigmentation, etc.).
Contraindications to EVLT are:
- inflammation of the skin at the site of the planned operation;
- ischemia, heart attack, stroke;
- pulmonary failure;
- infectious diseases;
- pregnancy and lactation.
Endovascular ablation in the ACMD clinic is carried out using a radial high-tech laser under continuous ultrasound control. A probe with a laser emitter is inserted into the lumen of the affected vessel through a small puncture, which seals the walls of the vessel.
EVLT can be combined with miniphlebectomy, which allows you to achieve the desired therapeutic result without significant tissue trauma. The procedure takes place quite quickly (from 40 minutes to 1 hour) and is accompanied by a short rehabilitation period without the risk of bleeding, tissue scarring and the appearance of scars.
Postoperative period
Mini punctures in the skin heal on their own and do not require stitches. There are no scars or scars left as the incision diameter is extremely small.
After surgery, it is enough to wear elastic medical knitwear or special bandages for 3-4 weeks. The wounds are closed with adhesive stickers. After the specified time, the patient comes for a follow-up examination.
Pain during the rehabilitation period is either mild or completely absent, so painkillers are not required. But if discomfort still occurs, the doctor prescribes drugs from the group of anti-inflammatory non-steroidal drugs or paracetamol. The course of treatment is 1-2 days.
Miniphlebectomy: the essence of the procedure
Miniphlebectomy is the removal of varicose veins through small punctures in the skin under local or general anesthesia. Indications for surgery are:
- phlebeurysm;
- thrombophlebitis and thrombosis;
- varicose nodes.
Miniphlebectomy is not performed during pregnancy, lactation, or in the presence of acute chronic heart disease, pulmonary insufficiency, infectious diseases and hypertension.
The operation is performed through very small (up to 2 mm) punctures in the skin, after which there are no scars. After the procedure, it is recommended to wear compression stockings and be observed by a phlebologist for 1 year.
Combined phlebectomy
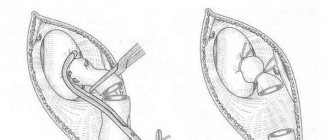
Combined phlebectomy consists of two main stages. The first stage is invagination (inversion) stripping - this is the removal of the GSV trunk using a special probe, which bluntly isolates the vein from the surrounding tissues (by turning it inside out - intussusception - and gradually tearing it off), which ensures less trauma and a good cosmetic result. Today, intussusception stripping is the main method of partial removal of the GSV. To do this, use a special thin metal probe (PIN probe, PIN stripping). With PIN stripping, one incision is required in the groin (after crossectomy); a probe with a thread fixed on it is passed through the lumen of the entire segment to be removed and brought out through a small puncture on the lower leg. In the area of the probe head, the vein is dissected, the thread is taken out through the hole and tied to the vein. Thus, the surgeon’s efforts are transferred to the vein through a fixed thread, causing it to evert and be removed. The vein is easily removed through a puncture in the lower leg. The main advantage of PIN stripping is the absence of a full incision (and therefore no stitches) on the lower leg, which improves the aesthetic result of the operation. In general, intussusception safenectomy is associated with less tissue trauma, a low risk of complications, better cosmetic effects (minor hemorrhages), and the absence of sensory disorders.
Miniphlebectomy is the removal of varicose veins through miniature punctures that do not require sutures and heal with virtually no scar, using a special set of instruments. At the present stage of development of phlebology, miniphlebectomy is the leading method for eliminating varicose veins, which in terms of cosmetic effect is in no way inferior to its alternative - compression sclerotherapy, but requires less material and time costs (the patient completely gets rid of the disease during one operation). During a miniphlebectomy, pre-marked veins are removed through small skin punctures (1-2 mm!) made with a special scalpel. First, the surgeon, using a spatula, clears the vein from the surrounding tissue, then, using a hook (dissector), picks up the vein and pulls it through the puncture, grabbing it with a special small clamp (mosquito). Next, the vein is intersected with clamps, the head segment, excluded from the bloodstream by the previous stages of combined phlebectomy (stripping, ligation of perforators), is removed by screwing onto the clamp, and the remaining part is removed from the next puncture. There are no stitches on the punctures, and they heal with virtually no visible scarring. Also, the miniphlebectomy technique is used to eliminate perforating discharge in the absence of trophic disorders - with perforating veins of small diameter, it is enough to simply remove the subcutaneous tributaries in the projection area of the perforator in order to turn it off from the blood circulation and cause subsequent obliteration.
Sclerotherapy for varicose veins
Sclerotherapy is an innovative method of treating vascular diseases, based on the introduction of chemical sclerosants into the vascular lumen, which cause the walls to weld together and the subsequent natural resorption of the vein. The technique has almost no contraindications, is accompanied by a minimal risk of complications, and is easy and painless for patients. The operation is performed without incisions, so there are no scars left after the operation.
Indications for sclerotherapy are:
- varicose veins;
- telangiectasia (“stars” of small vessels);
- varicose veins in reticular form;
- benign tumor neoplasms in the vascular and lymphatic systems.
Sclerotherapy is not performed during pregnancy, lactation, or if you are allergic to sclerosing drugs. The individual reaction to sclerosing agents is checked in advance. Other contraindications for therapy are:
- severe atherosclerosis;
- active thrombophlebitis;
- repeated thromboses in the past;
- congenital and acquired severe heart diseases;
- inflammatory and infectious skin diseases at the site of surgery.
For sclerotherapy, ultra-thin sterile needles with a diameter of 0.2-0.5 mm are used. There is no pain during the procedure, there may only be slight discomfort, which is eliminated with local anesthesia. Injections are administered into pre-marked areas. Several punctures can be performed in one procedure (3-5 for main forms of varicose veins, 10-15 for multiple manifestations of varicose veins). A sclerotherapy session lasts 10-25 minutes. Depending on the severity of the pathological process, from 1 to 5 sessions may be required.
The specialists of the ACMD clinic will select the optimal treatment method for each patient. Come to the ACMD clinic to get rid of vascular diseases once and for all!
Preparing for surgery
Before the operation, the patient must undergo a standard examination: donate blood for a general analysis, markers of hepatitis C and B, for RW and HIV, and undergo fluorography.
Those over 40 years old must also submit the results of an electrocardiogram and a physician’s report. Sometimes they are supplemented with simple blood clotting tests (to identify disorders of coagulation hemostasis) and Duke bleeding duration (to identify vascular-platelet dysfunctions).
Technique of the procedure
It is aimed at preventing varicose veins and has replaced another technique - excision of varicose tributaries of the main venous vessels according to Narat. During the procedure, special hooks are used, which are inserted through mini-punctures in the skin (with a cross-section of 1-2 millimeters).
- Before the procedure itself, varicose veins are marked on the affected area with their precise positioning.
- Local anesthesia is then performed. Usually, a 0.25 percent solution of novocaine is sufficient for this. Other anesthetics are used if you are allergic to this drug. The substance is injected paravasally. At the same time, you can see how it moves along the bed of the vessel, forming a coupling. Often this approach makes it possible to more accurately identify small branches that were not identified during marking.
- Miniature punctures are made mainly along the lines of force. The distance between the incisions may vary depending on the compliance of the vein, its strength and other factors. It is most convenient to perform punctures in the area where the perforators originate and the veins divide.
- This is followed by the introduction of varixes with hooks, followed by stretching and tearing off the vein from outside the incision. There is no need to ligate (bandage) the veins, since even with active bleeding from the central zone, it is stopped by local compression during the procedure.
- Upon completion of the operation, adhesive stickers are applied to the wounds. The entire area can also be bandaged by placing rollers along the “bed” of the removed veins. A medical knitwear (compression bandage) is put on over everything. The optimal level of compression is the second degree (from 23 mm Hg/st to 32 mm Hg/st).
- After short-term medical observation, the patient is sent home. Staying in the recovery room is not always required.