- Classification of diuretics
- When are diuretics used?
- How to take diuretics
- Can it be taken by children?
- Treatment with diuretics
Diuretics are medications with a diuretic effect.
When they enter the body, they prevent the reabsorption (reabsorption) of water and salts dissolved in it in the renal tubules. This increases the rate of urine formation and excretion. In simple terms, diuretics are substances that help the body remove water and salts from the body. Experts have proven that with a decrease in reabsorption by just 1%, the volume of urine doubles. Even when taking medications with little effect, patients report frequent and more abundant urination.
General information about diuretic herbs
Herbs with diuretic effects are naturally occurring diuretics. They remove stagnant fluid from the body. If the dosages and doctor's recommendations are followed, the drugs do not cause harm to the patient.
Impact on the human body
The removal of fluid from the human body is due to the suppression of the action of the enzyme carbonic anhydrase. It promotes moisture retention in tissues by regulating hormonal balance.
Beneficial features
Diuretic herbs have the following beneficial properties:
The beneficial effects of diuretic herbs on the body.
- Relieves swelling. The tissues are freed from excess fluid. The lumen of physiological ducts increases. For example, blood vessels, veins and arteries. This occurs by reducing the pressure of excess moisture on the fabric. As a result, all organs function better and the load on them is reduced.
- Cleanse the body. Excess moisture removes various decay products, impurities and toxins. This prevents them from penetrating deep tissues and the bloodstream. As a result, it is possible to prevent intoxication and improve well-being in case of poisoning.
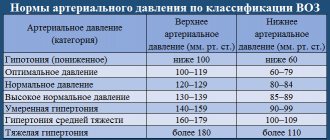
- Regulate pressure. When using diuretic herbs, the vascular lumen increases. It becomes easier for the heart to circulate blood, which leads to lower blood pressure and less strain on the muscle. Blood pressure becomes more stable, and surges occur less frequently.
- Supports kidney function. When taking diuretic herbs, the filtering function is stimulated. The kidneys are better at purifying water from impurities.
- Eliminating stagnation. Diuretics prevent water retention in the body. This is especially true for the urinary system. Herbs promote active fluid circulation. This prevents the development of infections and the formation of stones.
Some herbs have additional properties. For example, they can kill bacteria or promote the breakdown of kidney stones.
Many plants contain vitamins and minerals, which improve the patient’s general condition.
Treatment with diuretics
When prescribing diuretics, doctors adhere to the principles of rational therapy:
- At the first stage, a medicine with a moderate effect is prescribed.
- At the beginning of therapy, a minimum dosage of the drug is recommended with a gradual increase until the desired effect of diuretics is achieved. With intensive treatment, it is normal to increase the daily volume of urine by 800-1000 ml, and with maintenance therapy - by no more than 200 ml per day.
- For the majority, the optimal combination of diuretics with different mechanisms of action is optimal.
- To achieve a therapeutic effect, medications must be taken daily for the period recommended by your doctor.
It is important to be aware of the side effects of diuretics. Accidental or intentional abuse of such drugs leads to disruption of water and electrolyte balance. With prolonged use or an incorrectly selected dosage of diuretics, the risk of side effects increases:
- dehydration;
- heart rhythm disturbances;
- excessive decrease in blood pressure.
Headaches and muscle pains, nausea, vomiting, disturbances in the functioning of the gastrointestinal tract, weakness and convulsions, and drowsiness may also be observed. If you are hypersensitive to the drug, an allergic reaction may occur.
With prolonged diuretic therapy, mandatory monitoring of potassium and creatinine is indicated. If these indicators deviate significantly from the norm, a diuretic dosage adjustment or its complete discontinuation is required.
Indications for use
The main indications for the use of homeopathic diuretics include cystitis, swelling, cardiovascular pathology, etc.
Swelling
Herbs directly affect the water-salt balance and remove excess moisture from the body.
This reduces swelling. However, for a sustainable effect, you need to identify the cause of swelling and fight it. In this case, plants are used only as a symptomatic remedy. An additional benefit of herbs is that they can be used to treat several conditions. They improve the condition of the cardiovascular and urinary systems at the same time.
Mechanism of action of diuretics[edit | edit code]
The main thing in the mechanism of action of diuretics is their effect on the kidneys, the structural and functional unit - the nephron, on the processes that occur in it (glomerular filtration, tubular reabsorption, secretion).
To understand the mechanism of action of diuretics, let us briefly consider the process of urine formation. Each kidney contains about 1 million non-communicating nephron formations, consisting of a vascular glomerulus (glomerulus), glomerular capsule and tubules. In the renal glomerulus, plasma is filtered from the capillaries into the capsule cavity. The endothelium of the capillaries does not allow blood cells and proteins to pass through. The filtrate is called primary urine, which enters the kidney tubules from the glomerulus through the capsule. Filtration in the kidneys requires that the blood pressure in the glomerular capillaries exceed the oncotic pressure of the blood plasma. With a decrease in blood pressure, filtration in the glomeruli decreases; with an increase, on the contrary, it increases. The glomerular filtration rate depends not only on the blood supply to the kidneys, but also on the number of functioning nephrons.
Glomerular filtration in an adult averages 100 ml/min. During the day, 150-200 liters of fluid are filtered in the kidneys, and only 1.5-2 liters of urine are excreted, i.e. 99% of the primary urine is again absorbed (reabsorbed) in the tubules. The tubules are divided into proximal, which passes into the loop of the nephron (Henle) (V-shaped convoluted tube), and distal, through which urine passes from each nephron into the collecting ducts, and from them into the renal pelvis and through the ureters into the bladder.
The reabsorption process occurs throughout the nephron. In order to increase diuresis by 2 times, it is necessary to increase glomerular filtration by 2 times, which is practically impossible to do, or to reduce reabsorption by only 1%. Thus, urine formation can be significantly increased by reducing tubular reabsorption (Fig. 3.11). In addition to water, sodium, chlorine and potassium ions are reabsorbed in the tubules. It should be taken into account that in the tubules it is necessary to reduce the reabsorption of sodium ions, and water passively follows this osmotically active ion.
The effect of increasing filtration and decreasing reabsorption by 10% on the amount of diuresis
Sodium reabsorption in the kidney tubules occurs as follows. From the lumen of the tubule, Na+ enters the cell through the apical membrane. It is believed that sodium transport within the cell is carried out using a special carrier protein, the synthesis of which is regulated by aldosterone. Aldosterone binds to receptors in cells, is transferred to the nucleus and, influencing DNA, stimulates the synthesis of messenger RNA, which promotes the activation of the synthesis of the carrier protein in the ribosomes. Sodium, which entered the tubule cell, creates a fund (pool) of sodium, which is subsequently actively reabsorbed. Reabsorption is carried out using special pumps that are located on the basement membrane of the tubule wall cells. Several types of such pumps are known, one of them transports Na+ in exchange for K+. Others reabsorb Na+ together with SG or HCO~. This active transport of sodium is carried out due to the energy produced by mitochondria located near the basement membranes.
Reabsorption of sodium by epithelial cells of the renal tubular wall
About 70-80% of the total filtered Na+ is reabsorbed in the proximal tubules, followed by passive reabsorbment of water and SG. Carbonic anhydrase reabsorbs hydrogen carbonate (HCO3). The point of application of diuretics may be the proximal nephron, but their effect is insignificant, since a decrease in reabsorption in the proximal tubule entails a compensatory increase in it in the nephron loop and the distal tubule.
Active transport of Na+ and SG occurs in the nephron loop; its wall is impermeable to water. The action of diuretics primarily occurs in this part of the nephron; they are called loop diuretics. Blockade of sodium reabsorption in this department causes the greatest natriuresis.
Diagram of the nephron and localization of the action of diuretics (Farmakolopya, 2001): 1 - xanthines; 2 - diacarb; 3— mannitol; 4— furosemide, ethacrynic acid; 5 - dichlothiazide; 6— spirolactone, triamtren
Urine formation is completed in the distal nephron and collecting ducts. Transport processes here are controlled by hormonal influences. The sodium-retaining effect of the mineralocorticoid aldosterone and the water-retaining effect of the antidiuretic hormone (vasopressin) are manifested. Passive secretion of K+ from nephron cells occurs through the apical membrane along an electrochemical gradient. The distal tubule and collecting ducts can also be the point of application of diuretics (aldosterone antagonists, triamterene and others), but they are ineffective. Blocking Na+ reabsorption in this compartment, when about 90% of the filtered Na+ has already been reabsorbed, can increase its excretion by only 2-3% - the filtration charge. Sodium transport in the kidneys is also regulated by other factors. This is an atrial natriuretic hormone that is released from the atria when they are stretched, which causes an increase in glomerular filtration rate and inhibition of sodium reabsorption in the collecting ducts. In addition, there is natriuretic hormone - a low-molecular compound that enters the blood when volumoreceptors are stimulated and, like ouabain, blocks Na*, K+-ATPase in the kidneys, which reduces Na+ reabsorption. Substances that act as potential regulators of sodium excretion include estrogens, somatotropin, insulin (increase Na+ reabsorption), progesterone, parathyroidin, glucagon (reduce Na+ reabsorption). Factors that are formed in the kidneys (kinins, prostaglandins, dopamine, etc.) also act locally.
Considering the principles of functioning of the urinary system, it becomes clear that drugs that stimulate urination can directly affect the urinary function of the kidneys or change their hormonal regulation.
The use of diuretics, primarily as a means of symptomatic therapy aimed at reducing edema, also has an important pathogenetic effect on the complex chain of reactions in diseases that are accompanied by the retention of salts and water in the body.
There are more than 20 drugs in the arsenal of diuretics. Which of them should be preferred in a given situation should be helped by knowledge of pharmacokinetics, mechanism of action, possible side effects, and more.
List of the best diuretic herbs
The list of the best diuretic herbs includes milk thistle, thyme, calendula, horsetail, bearberry, etc. They differ in their effects and dosages.
Milk thistle
Milk thistle not only has a diuretic effect, but also cleanses the liver of toxins, accelerating cell regeneration. In the pharmacy the product can be found in the form of seeds, powder or meal. The first option is preferable, but you will have to grind the grains yourself to release the active substances. 2 tsp. raw materials pour 1 tbsp. boiling water, cover and leave for 15 minutes. Then the liquid is drained and drunk up to 3 times a day, regardless of meals.
Thyme
Thyme stimulates urination, relieves pain and inflammation, and destroys bacteria. It stimulates the digestion of food and, in case of pulmonary diseases, facilitates the removal of fluid from the bronchi. To prepare the medicine 1 tbsp. l. dried herbs, pour 200 ml of boiling water, leave for 20 minutes and filter. The product is drunk half an hour before meals, up to 4-5 times a day.
Thyme removes water and toxic substances from the body.
Calendula
Calendula relieves swelling and inflammation, destroys bacteria and viruses, strengthens the walls of blood vessels, and also activates regeneration processes. To brew tea, 2 tbsp. l. inflorescences are poured with 0.5 liters of boiling water. Cover the container with a lid and place in a dark place for 15 minutes. At the end, the liquid is filtered. Drink 100 ml of tea up to 3 times a day.
Horsetail
Horsetail enhances fluid removal, stops bleeding, enhances tissue regeneration and relieves inflammation. The plant has an antimicrobial effect, improves the condition of the renal ducts and vascular walls, which is most useful for cystitis and pyelonephritis. The medicine is prepared from 4 tbsp. l. dry horsetail. It is poured with 0.5 liters of boiling water and left for 20 minutes. The product is drunk warm. Dosage - 2 tbsp. l. infusion up to 3 times a day 30 minutes before meals.
Bearberry
Bearberry helps remove excess moisture from the body by irritating the kidney tissue. The product has anti-inflammatory and antiseptic properties. To prepare the decoction 1 tbsp. l. dry leaves are ground to a powder. 250 ml of hot water is poured into the mass. The mixture is placed in a water bath for 20 minutes, then allowed to brew for 40 minutes and filtered. After this, the volume is adjusted to the original volume by adding water. The drug is taken 50 ml half an hour after meals up to 3 times a day.
Bearberry normalizes metabolism and eliminates swelling.
Rose hip
Rosehip not only removes moisture from tissues, but also has an anti-cancer and anti-inflammatory effect. It protects the kidneys and liver, prevents the development of cancer, and heals wounds. 1 tbsp. l. The berries are passed through a meat grinder, placed in a saucepan and poured with 0.5 liters of boiling water. Cover the container with a lid and steam for 30 minutes. Then filter the liquid, pour in another 2 cups of boiling water and leave again for half an hour. Ready-made tea is drunk up to 3-4 times a day, 250 ml.
Nettle
Nettle has a diuretic, anti-inflammatory and antibacterial effect. It stops bleeding, normalizes the activity of the immune system, blood sugar and cholesterol levels. The product reduces pain in the back, neck and lower back, cleanses the body of toxins. The decoction is prepared from 1 tbsp. l. leaves and 1 tbsp. water. The mixture is brought to a boil. Leave the container under a towel in a warm place for 1 hour. The finished broth is filtered. Take up to 1-2 glasses daily; for internal bleeding, the portion is increased to 1 liter.
Chamomile
Chamomile is not only a diuretic, but also an antispasmodic. This helps ease urination during cystitis. The product relieves inflammation, calms a person, dilates blood vessels, improves blood circulation. The infusion is prepared from 2 tbsp. l. inflorescences and 250 ml of boiling water. The mixture is left covered until completely cooled. The finished product is taken 1 tbsp. before meals up to 3 times a day.
Chamomile decoction is used in the treatment of many diseases, including cystitis.
Birch
Birch leaves are a natural diuretic, antiseptic and anti-inflammatory agent. They are often used for inflammatory pathologies of the urinary system. A decoction is prepared from 2 tsp. crushed leaves and 200 ml of hot water. The product is infused for 20 minutes, then filtered. Take 100 ml before meals twice a day.
Linden
Linden normalizes digestion, removes moisture through the bladder and skin pores, and reduces body temperature. A compress of flowers relieves headaches and treats burns. 1 tbsp. l. dried raw materials are poured with 200 ml of boiling water. The product is drunk warm before meals. This is done 2-3 times a day.
Valerian
Valerian is a weak diuretic. It copes better with edema than with cystitis or pyelonephritis. However, the plant has a beneficial effect on the heart. It is recommended to be used together with other herbs. You can add mint in a 1:1 ratio. 1 tbsp. l. collection pour 1 tbsp. boiling water, drink 200 ml once a day.
Motherwort
Motherwort has general strengthening properties. It improves the condition of the immune and nervous system, relieves swelling, relieves cramps, cough and inflammation. The product reduces pain. 1 tbsp. l. motherwort is poured with 300 ml of boiling water. The finished infusion is drunk 150 ml twice a day.
Motherwort decoction is used to treat diseases of the nervous system.
Mint
Mint not only helps remove moisture, but also disinfects tissues. It helps with flu and colds, relieves pain, and improves digestion. Tea is prepared from mint: 2 tsp. crushed raw materials, pour 200 ml of boiling water for 20 minutes. After filtering, drink the product up to 2-3 times a day.
Oregano
Oregano is often used in gynecology. It normalizes hormonal levels, protects the genitourinary system from tumors, and relieves inflammation. Men treat urethritis, prostatitis and infections with oregano. Tea is prepared from 2 tsp. dry herbs and 250 ml of hot water. The mixture is infused for half an hour. It is drunk before meals or between meals, 50-100 ml three times a day.
The course of treatment should not exceed 1 week.
Clinical pharmacologist to assist the endocrinologist: the choice of oral glucose-lowering therapy
Currently, there is a wide arsenal of inpatient and outpatient agents that can affect almost all known links in the pathogenesis of type 2 diabetes mellitus (DM). There are many classifications of them, including division by main effect, by points of application, by mechanism of action, by duration, etc.
There are hypoglycemic agents and antihyperglycemic agents. The purpose of hypoglycemic drugs (sulfonylurea derivatives and meglitinides) is to stimulate the synthesis of endogenous insulin, as a result of which, among the positive aspects of treatment, negative events also occur: weight gain and an increased risk of developing hypoglycemic conditions.
Antihyperglycemic drugs (α-glucosidase inhibitors, biguanides, thiazolidinediones, incretin mimetics) improve peripheral glucose utilization, but do not have a stimulating effect on pancreatic β-cells. Due to this, the level of insulin in the blood does not increase and blood glucose does not decrease below normal [1].
Antihyperglycemic agents affecting the small intestine prevent complete absorption of carbohydrates in the intestine by inhibiting α-glucosidase enzymes that affect the pancreas (secretogens) - causing its β-cells to secrete endogenous insulin, and affecting hepatocytes, adipose and other peripheral tissues (sensitizers) - increase the sensitivity of target organs to insulin.
Examples of secretogenic hypoglycemic drugs are sulfonylureas (glibenclamide, gliclazide, glimepiride) and prandial glucose regulators - meglitinides (nateglinide, repaglinide). Sensitizers are represented by biguanides (metformin) and thiazolidinediones (pioglitazone, rosiglitazone).
A relatively new class of glucose-lowering drugs are incretin mimetics (vildagliptin, saxagliptin, exenatide, liraglutide), the insulinotropic effect of which is glucose-dependent and is realized only at elevated glycemic levels. When normoglycemia is achieved, the insulin concentration returns to the basal level, which helps reduce the risk of developing hypoglycemia while taking these medications. The mechanism of action of these drugs is glucose-dependent and does not interfere with the normal glucagon response to hypoglycemia [2]. The main classes of oral hypoglycemic drugs and their mechanisms of action are presented in Table. 1 and in Fig. 1.
The reader is presented with dozens of names of medicines belonging to different pharmacological groups, each with its own mechanism of action, evidence base and cost. With such an abundance of medications, within a short period of communication with the patient, as well as in conditions of comorbidity and forced polypharmacy, choosing the right medication in an adequate dosage regimen is very difficult to do - almost impossible, which dictates the need to designate the clinical and pharmacological niches of these drugs, as well as their advantages and disadvantages (Fig. 2–8).
α-glucosidase inhibitors should be used primarily for the prevention of type 2 diabetes mellitus in patients with early manifestations of insulin resistance. In addition, they are the drugs of choice for people with prediabetes, which is accompanied by postprandial hyperglycemia at normal fasting levels (reduction in HbA1c levels by 0.5–0.8%).
Indications for prescribing glinides are type 2 diabetes mellitus when diet and exercise are ineffective. They are also designed to preferentially reduce postprandial hyperglycemia (0.5% to 1.5% reduction in HbA1c).
The clinical niche for the prescription of glitazones (thiazolidinediones) is reduced to type 2 diabetes mellitus, as monotherapy or in combination with a sulfonylurea drug, biguanides or insulin in the absence of effect from diet therapy, exercise and monotherapy with one of the above drugs (reduction of HbA1c level by 0 .5–1.4%).
Biguanides are the drugs of choice both for people with prediabetes, accompanied by fasting hyperglycemia and with normal sugar levels after meals, which indirectly indicates insulin resistance, and for patients with type 2 diabetes mellitus. Their administration is possible in the form of monotherapy and in combinations, primarily with secretogens (when the latter do not provide complete correction of hyperglycemia) and with insulin (in the presence of insulin resistance) (reduction of HbA1c levels by 1–2%).
The administration of sulfonylurea derivatives is usually associated with the presence of type 2 diabetes in cases where diet and exercise, the administration of α-glucosidase inhibitors and biguanides were ineffective (reduction in HbA1c levels by 1–2%).
Drugs with incretin activity (Fig. 7), which primarily affect GLP1, are prescribed for type 2 diabetes as an addition to therapy with biguanides, sulfonylurea derivatives, thiazolidinediones in case of inadequate glycemic control (reduction in HbA1c level by 0.8–1.8 %).
Another type of incretin mimetics are drugs that affect DPP4 (Fig. 8), which are advisable to prescribe for type 2 diabetes mellitus as monotherapy in combination with diet therapy and exercise; in combination with biguanides as initial drug therapy when diet therapy and exercise are insufficiently effective; as well as as part of two-component combination therapy with biguanides, sulfonylurea derivatives, thiazolidinediones or insulin in case of ineffectiveness of diet therapy, exercise and monotherapy with these drugs (reduction in HbA1c levels by 0.5–1.0%).
The mechanism of action of DPP4 inhibitors is as close as possible to the natural processes occurring in a healthy human body. Under their influence, there is a decrease in the frequency of protective snacks that patients eat to avoid hypoglycemia, a decrease in the absorption of fat from the intestine, an increase in energy expenditure, and an increase in lipid oxidation during meals [3]. In addition, in diabetes, as a result of increased apoptosis, β-cells lose their mass, which is reflected in significant impairments in their functions, the main of which is insulin synthesis. The physiological effect of this group of drugs supports the viability of pancreatic β-cells, increases their mass by 75% and reduces apoptosis by 65% [4]. A comparison of the main representatives of DPP4 inhibitors is presented in table. 2.
The cardiovascular effects of DPP4 inhibitors are reduced to reducing myocardial remodeling, improving endothelial function, reducing atherogenic lipoprotein fractions, lowering blood pressure (BP), reducing symptoms of circulatory failure, protecting the myocardium from ischemia, as well as functional restoration of the myocardium after ischemia and increasing the number of receptors to insulin in cardiomyocytes [5]. Cardiometabolism of DPP4 inhibitors is presented in Table. 3.
Summary data reflecting the advantages and disadvantages of the main classes of glucose-lowering drugs are presented in table. 4.
As can be seen from the table presented:
- in case of cardiovascular diseases, patients should avoid drugs with a high likelihood of developing hypoglycemia, which can be very dangerous for them;
- overweight patients should be prescribed antihyperglycemic drugs that do not promote further weight gain;
- when treating women of childbearing age, the possibility of pregnancy should be taken into account, in which tableted hypoglycemic drugs are contraindicated;
- all tableted hypoglycemic drugs are contraindicated in persons with diabetic ketoacidosis;
- in patients with alcoholic visceropathy and liver cirrhosis, the choice of hypoglycemic therapy should be based on the characteristics of the drug’s metabolism, as well as the duration of its action;
- in patients with CKD (including those resulting from diabetic nephropathy), glycemic correction should be carried out under the control of glomerular filtration rate (GFR).
The inability to maintain compensation of carbohydrate metabolism in patients on monotherapy, as well as the high risk of developing acute and chronic complications of diabetes mellitus in comorbid patients are sufficient grounds for combination treatment. In the case of combined glucose-lowering therapy, improvement in the effectiveness of treatment is a consequence of the combination of the mechanisms of action of drugs (for example, secretogens and sensitizers) [6]. Combination therapy is accompanied by an improvement in the quality of life of patients and is well tolerated by them, which is associated with a parallel effect on different parts of the pathogenesis of diabetes and with a decrease in the number of simultaneous administration of tablet drugs while improving the compensation of carbohydrate metabolism (Fig. 9).
However, the evolution of oral glucose-lowering agents continues - in November 2012, the first representative of the newest class of oral sodium-glucose cotransporter type 2 (SGLT2) inhibitors, dapagliflozin, was approved in Europe, and in March 2013, the Food and Drug Administration The Food and Drug Administration (FDA) has approved canagliflozin for the treatment of adult patients with type 2 diabetes mellitus. Registration applications for empagliflozin, ipragliflozin and luseogliflozin have also been submitted to US, European and Asian regulatory authorities, with large-scale studies currently ongoing.
The mechanism of their action is as follows. Due to the active reabsorption system, this glucose is almost completely reabsorbed in the proximal tubule of the nephron. The urine entering the loop of Henle is free of glucose. An increase in the concentration of glucose in the blood plasma leads to an increase in its filtration in the glomeruli. When the rate of glucose entry into the proximal tubule increases above 260–350 mg/min/1.73 m2, for example in patients with diabetes, excess glucose exceeds the reabsorption potential and it begins to be excreted in the urine. In a healthy adult, this corresponds to a blood glucose concentration of about 10–11 mmol/L (180–200 mg/dL). Since glucose is not able to freely penetrate the cell membrane, sodium-dependent glucose transporters (SGLT1 and 2) are involved in its absorption in the intestine and reabsorption in the kidneys [7]. Accordingly, SGLT inhibitors reduce blood glucose concentrations by stimulating its excretion in the urine.
Expert opinion regarding registered SGLT2 inhibitors that have become an alternative to metformin, including in cases of intolerance, is ambiguous. On the one hand, drugs of this class offer new opportunities in the treatment of diabetes: first of all, a new, insulin-independent mechanism of action, no negative effect on body weight and even a slight decrease in weight, favorable pharmacokinetic properties and generally good tolerability [8]. On the other hand, the mechanism of action of SGLT2 inhibitors is aimed at the clinical manifestations of diabetes, and not at its cause [9]. Due to SGLT2 inhibition, the degree of glycosuria depends on renal function, and since in patients with diabetes it decreases as the disease progresses, the long-term effectiveness of these drugs remains unknown. In addition, the presence of glucose in the urine has always been considered an undesirable phenomenon, and many doctors are not ready to prescribe drugs that cause glucosuria. The latter is also the cause of the most common side effects - urinary tract infections and fungal infections of the genitals [10].
The clinical and pharmacological niches of this class of drugs will be revealed by time, and the answers to many questions should be dispelled by the results of clinical studies of these drugs, but today there is no doubt about the postulate that when choosing a hypoglycemic drug, the doctor must remember that in each specific case adequate therapy for diabetes is possible only if the patient’s age, sex, gender characteristics, body weight, as well as the etiological and pathogenetic mechanisms of the development of the disease are taken into account.
Literature
- De Fronzo R. Pharmacologic therapy for type 2 diabetes mellitus // Ann Inter Med. 1999; 131:281–303.
- Dedov I. I., Shestakova M. V. Incretins: a new milestone in the treatment of type 2 diabetes mellitus. M., 2010. pp. 55–62.
- Rosenstock J. Comparison of vildagliptin and rosiglitazone monotherapy in patients with type 2 diabetes: double-blind, randomized trial // Diabetes Care. 2007, 30(2): 217–223.
- Matikainen N. Vildagliptin therapy reduces postprandial intestinal triglyceride-rich lipoprotein particles in patients with type 2 diabetes // Diabetologia. 2006, 49: 2049–2057.
- Duttaroy A. The DPP-4 inhibitor vildagliptin increases pancreatic beta-cell neogenesis and decreases apoptosis / Poster No. 572 presented at ADA, 2005.
- Balabolkin M.I., Klebanova E.M., Kreminskaya V.M. Combined hypoglycemic therapy and the possibility of achieving long-term compensation of carbohydrate metabolism in patients with type 2 diabetes mellitus // Russian Medical Journal. 2007, no. 17, p. 492–496.
- Hardman TC, Dubrey SW Development and Potential Role of Type-2 Sodium-Glucose Transporter Inhibitors for Management of Type 2 Diabetes // Diabetes Ther. 2011; 2 (3): 133–145.
- Experts Express Mixed Thoughts on Canagliflozin Approval. Medscape Medical News. Apr 18, 2013. https://www.medscape.com/viewarticle/782712.
- Kim Y., Babu AR Clinical potential of sodium-glucose cotransporter 2 inhibitors in the management of type 2 diabetes // Diabetes Metab Syndr Obes. 2012; 5:313–327.
- Ushkalova E. A. A new class of antidiabetic drugs - inhibitors of sodium-glucose cotransporters // Pharmateka. 2013, no. 16, p. 33–36.
A. S. Skotnikov*, 1, Candidate of Medical Sciences M. G. Selezneva**
* State Budgetary Educational Institution of Higher Professional Education First Moscow State Medical University named after. I. M. Sechenova, Moscow ** GBUZ City Clinical Hospital No. 5 DZM, Moscow
1 Contact information
List of other diuretic herbs
For convenience, diuretic herbs are divided into categories depending on their effect.
Medicinal fees
Among the medicinal fees, the following can be distinguished:
- Diuretic collection No. 1. Contains bearberry, cornflower and licorice in a 3:1:1 ratio. Removes moisture, destroys germs and suppresses infections.
- Diuretic collection No. 2. Contains licorice, bearberry and cornflower. The drug helps relieve pain in kidney pathologies and reduces foci of inflammation.
- Diuretic collection No. 3. Contains horsetail, juniper and wheatgrass root. The product is potent, so it is used with caution. Most often, the collection is prescribed to patients suffering from an allergy to licorice root.
- Collection of herbs No. 6. Contains lemongrass, corn silk, horsetail and chamomile. Helps restore water-salt balance.
Diuretic herbal mixtures are presented in various combinations.
Anti-inflammatory drugs
Relieving inflammation helps reduce pain due to pathologies of the urinary system.
This is useful for cystitis and pyelonephritis. Internal swelling disappears due to the elimination of stagnation and excessive blood flow to the damaged area. The most powerful anti-inflammatory diuretics are the following herbs:
- burdock root;
- pink radiola;
- stinging nettle;
- lingonberry leaves;
- parsley;
- corn silk;
- marshmallow
For hypertension and heart failure
For hypertension, it is advisable to take herbs that strengthen the walls of blood vessels. This promotes proper blood circulation and helps the cardiovascular system withstand high stress without side effects.
Herbal tea for hypertension strengthens the walls of blood vessels.
For heart failure and hypertension, the following herbs and berries are brewed:
- shepherd's purse;
- red rowan;
- swampy dried grass;
- barberry roots;
- motherwort;
- mint;
- lemon balm.
For facial swelling
If you experience frequent swelling of the face, it is recommended to pay attention to the symptom. Its location indirectly indicates the source of the problem. For example, swelling in the upper lip or brow ridges indicates cardiac pathology.
Swelling of the eyelids is a sign of kidney disease.
The following remedies help with facial swelling:
- half fell;
- flax seeds;
- beet leaves;
- corn silk.
A decoction of corn silk will eliminate swelling on the face.
For the kidneys
For infectious pathologies of the urinary system, horsetail and knotweed are used. Herbs increase fluid circulation, prevent congestion, destroy bacteria, and relieve inflammation from damaged tissues.
For swelling of the legs
Swelling of the legs is most often observed due to impaired lymph outflow, pathology of the liver, heart, thyroid gland, and renal failure.
To improve the condition, use chamomile, horsetail, bearberry, nettle or lemon balm.
For weight loss
Diuretic herbs are used as an adjuvant. On their own, they will not provide sustainable weight loss, but they can improve the results of diet and exercise. For weight loss, horsetail, bear ears, and lingonberry leaves are used. The latter are the mildest and safest remedy.
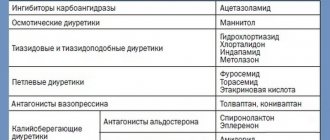
Classification of diuretics[edit | edit code]
Today there is no perfect classification that would take into account all aspects of the action of diuretics. Diuretics, having different chemical structures, differ in localization, mechanism, strength of action, speed of onset of effect, its duration, and side effects. For a long time, the classification of diuretics was based on their chemical structure. Attempts have been made to classify diuretics according to the nature of their effect on the kidneys. However, many diuretics also have extrarenal effects. Attempts to classify diuretics according to their ability to influence one or another part of the nephron are also associated with difficulties. The diagram (Fig. 3.14) shows that some of these drugs (xanthines, furosemide, ethacrynic acid, osmotic diuretics, etc.) act throughout the nephron. Therefore, it is rational to classify diuretics based on their mechanism of action.
Points of action of diuretics at different levels of the nephron
Depending on pharmacodynamics, modern diuretics are divided into three groups: saluretics, potassium-sparing diuretics, osmotic diuretics.
Saluretics include thiazide derivatives (hydrochlorothiazide, cyclomethiazide), thiazide-like (clopamide, chlorthalidone), loop diuretics (furosemide, torasemide, ethacrynic acid, bumetanide), carbonic anhydrase inhibitors (diacarb).
Potassium-sparing diuretics include triamterene, amiloride and spironolactone, eplerenone, which increase sodium excretion and have a slight effect on potassium excretion.
Osmotic diuretics (mannitol, urea), increasing osmotic pressure in the tubules, prevent water reabsorption. However, it should be noted that this systematization does not include diuretics that affect blood circulation in the kidneys; it is not very focused on the mechanism of action of the drugs.
To better understand the action of modern diuretics, a classification of diuretics is recommended, which takes into account not only the mechanism, but also the localization of their action.
I. By localization and mechanism of action.
1. Agents acting at the level of renal tubular cells.
1.1. Agents acting at the level of the apical membrane.
1.1.1. Competing for the sodium transporter, or non-competitive aldosterone antagonists—triamterene, amiloride.
1.1.2. Competing aldosterone antagonists are spironolactone, eplerenone.
1.2. Agents acting at the level of the basement membrane.
1.2.1. Carbonic anhydrase inhibitors - diacarb.
1.2.2. Thiazide diuretics - hydrochlorothiazide, cyclomethiazide.
1.2.3. Thiazide-like diuretics - chlorthalidone, clopamide, indapamide.
1.2.4. Loop diuretics - furosemide, ethacrynic acid, bumetonide, torsemide.
2. Osmotically active diuretics - mannitol, urea.
3. Drugs that increase blood circulation in the kidneys - xanthines, aminophylline, aminophylline, etc.
4. Preparations of medicinal plants - horsetail, bearberry leaves, birch buds, orthosiphon leaves, lingonberry leaves, leaves and stems of Lespedesa capitata, torment leaves, strawberries, etc.
From a clinical point of view, strength, speed of onset and duration of action are of practical importance when choosing a drug. Therefore, diuretics are classified as follows.
II. By force of action.
1. Strong diuretics - furosemide (Lasix), torasemide (Trifas), ethacrynic acid (Uregit), clopamide (Brinaldix), osmodiuretics (mannitol, urea), etc.
2. Medium diuretics - thiazides: hydrochlorothiazide (hypothiazide, dichlothiazide), cyclomethiazide and thiazide-like - chlorthalidone (oxodoline, hygroton), etc.
3. Weak diuretics - spironolactone (veroshpiron, aldactone), diacarb (acetazolamide), triamterene (pterophen), amiloride, xanthines aminophylline (euphylline), medicinal plant preparations (bearberry leaves, orthosiphon leaves, birch buds, etc.).
III. According to the speed of onset of the diuretic effect.
1. Fast (emergency) action (30-40 min) - furosemide, torsemide, ethacrynic acid, mannitol, urea, triamterene.
2. Medium-acting (2-4 hours) - diacarb, aminophylline, amiloride, cyclomethiazide, clopamide, chlorthalidone, etc.
3. Slow action (2-4 days) - spironolactone, eplerenone.
IV. According to the duration of the diuretic effect.
1. Short-acting (4-8 hours) - furosemide, torsemide, ethacrynic acid, mannitol, urea, etc.
2. Medium duration (8-14 hours) - diacarb, triamterene, hydrochlorothiazide, clopamide, aminophylline, etc.
3. Long-term action (several days) - chlorthalidone, spironolacgon, eplerenone.
Diuretics acting at the level of renal tubular cells Drugs that disrupt sodium transport across the apical membrane of renal tubular cells include triamterene, amiloride, spironolactone, and eplerenone. They act at the level of the distal nephron. These are drugs that reduce the processes of physiological reabsorption of sodium and water.
Herbal diuretic tablets
The most popular herbal diuretics are:
- Cyston;
- Urolesan;
- Phytolysin;
- Canephron.
Popular herbal diuretic tablets.
Diuretics in tablet form are preferable because manufacturers include a balanced complex of herbs. The ingredients enhance each other's effects. It is more convenient for patients to take medicine in tablet form rather than brew dried plants.
Precautions and contraindications
Contraindications depend on the type of herb. The list will be different for each plant. Experts recommend either collecting herbs yourself or buying them at a pharmacy. The first option is preferable, since the points of sale most often end up with cake from which most of the beneficial substances have already been removed.
However, it is better to collect plants either in the field or in the garden.
Do not pick herbs in environmentally unfavorable areas or near roads.
Rules for collecting medicinal herbs.
When choosing a diuretic, preference should be given to a plant that is already familiar to the body or at least grows in your region. This will reduce the risk of allergies. Undesirable reactions can worsen the patient’s condition, especially with infectious and cardiac pathologies.
When brewing medicines, you must follow all the rules regarding the proportions of ingredients, preparation technology, etc. You cannot independently change the dosage of ready-made products or extend the course. This can only be done by a doctor after assessing the patient’s condition. Herbal diuretics can be taken longer than synthetic ones, but this cannot be done on an ongoing basis. Otherwise, the metabolism will be disrupted and a deficiency of microelements will occur.