Chronic diffuse liver diseases often occur in women of childbearing age. The most common form of liver damage is chronic hepatitis of viral etiology, more rare are autoimmune and drug-induced hepatitis, cholestatic forms of damage (primary biliary cirrhosis, primary sclerosing cholangitis), alcoholic liver damage, non-alcoholic steatohepatitis (due to obesity, diabetes mellitus), Wilson's disease - Konovalova and others.
Recent decades have been marked by an increase in the number of people infected and suffering from viral chronic liver diseases (CLD), especially among young people, as well as the emergence of a number of new drugs that allow successful etiopathogenetic treatment of some forms of liver damage. This leads to an increase in the number of pregnant women and postpartum women suffering from CKD. Features of the course of CKD in pregnant women, management tactics for such patients, in particular, indications for drug treatment and issues of its safety have not been sufficiently studied.
Causes of chronic liver diseases
Chronic liver diseases - hepatitis - can be caused by a variety of reasons, the main ones:
- hepatitis viruses (hepatitis B virus, hepatitis C virus) are the most common cause of chronic hepatitis;
- a violation of fat metabolism, which leads to fat deposition in the liver (steatohepatitis);
- alcohol abuse (alcoholic liver disease);
- autoimmune disorders (autoimmune hepatitis, primary biliary cirrhosis, primary sclerosing cholangitis);
- long-term use of medications;
- genetic defects - hereditary liver diseases.
Diagnosis of diffuse changes
DIPVs are determined using an ultrasound machine. Ultrasound shows an increase or decrease in tissue density, changes in structure, and foci of inflammation. But this is not enough. And therefore, to confirm the presence of DI, a biochemical blood test and endoscopy of the gland are performed. An important role in diagnosis is played by anamnesis, that is, questioning the patient about the presence of complaints, instrumental examination and palpation. Additionally, a general blood test, stool urine analysis, and gastrointestinal endoscopy are performed. The purpose of the research is:
- the amount of pancreatic enzymes and glucose in the blood
- ratio of inhibitor to trypsin.
Ultrasound allows you to determine the size of the gland, the condition of the duct, the presence of tumors and seals. Additionally, computed tomography and ERCP are performed, which help identify the true causes of changes in the tissues of the enzyme-forming organ.
Hereditary liver diseases
Hereditary chronic liver diseases are quite rare, therefore, even with repeated examinations, they are not recognized by doctors and patients are treated for a long time for other diseases.
The main hereditary liver diseases include: Gilbert's syndrome, hemochromatosis, Wilson-Konovalov disease, etc.
Hemochromatosis is a disease of autosomal recessive inheritance, characterized by impaired iron metabolism, excessive absorption in the intestine, increased content in the blood and deposition in various tissues with increased structure and dysfunction of the liver, heart, and pituitary gland. Clinical symptoms in the early stages of the disease are nonspecific: weakness, fatigue, weight loss, joint pain. The examination reveals an increase in ALT and AST.
In the terminal stage, the classic triad manifests itself: skin pigmentation, cirrhosis and diabetes mellitus. For diagnosis, the level of iron in the blood, transferrin, ferritin, total iron-binding capacity, as well as ALT and AST are determined. Genetic analysis for hemochromatosis reveals the presence of hereditary factors - mutations of the HFE gene. Genetic testing is also carried out for close relatives of patients with confirmed hemochromatosis.
The goal of treatment is to remove excess iron from the body. Good results are obtained by bloodletting under the control of a clinical blood test and the patient’s well-being. In addition, drugs are used to help remove iron from the body and prevent the formation of cirrhosis. Timely initiation of therapy prolongs the life of patients by several decades.
Konovalov-Wilson disease is a hereditary disease based on increased absorption of copper in the intestine and decreased synthesis of the copper-binding protein ceruloplasmin in the liver. This leads to excessive accumulation of copper in the blood and its deposition in tissues with primary damage to the liver, central nervous system, kidneys, cornea and other organs. The clinical picture consists of symptoms of liver damage, neurological and mental disorders. In the early stages of the disease, symptoms of hepatitis, hepatomegaly, and splenomegaly (enlarged liver and spleen) appear. Later, signs of functional liver failure, portal hypertension, jaundice, and a slowly progressive form of cirrhosis increase.
Damage to the nervous system is manifested by hand tremors, speech impairment, prolonged muscle spasms, decreased intelligence up to dementia. A typical sign of the disease is the deposition of a greenish-brown pigment containing copper in the cornea - Kayser-Fleischer rings. Treatment is aimed at removing excess copper from the body - a special diet with a limited copper content and drugs that bind and remove copper.
What is diffusion?
Diffuse changes in the pancreas are detected by ultrasound.
Pathological changes in pancreatic tissue can be local (focal) or diffuse (mixed). The term diffusion is used in physics and chemistry. And considering this term from the point of view of these sciences will allow us to better understand the essence of the processes occurring in our body.
The term diffusion comes from the Latin word, and means interaction, spreading. In other words, this is the penetration of molecules or atoms of one substance between molecules or atoms of another substance.
The phenomenon of diffusion can be observed when ink is poured into water. In anatomy, diffusion means the interpenetration and replacement of some tissue cells by others. This phenomenon is often observed in the pancreas, where pathologically altered cells coexist with healthy ones. Therefore, diffuse transformations of the pancreas are usually detected by ultrasound.
Symptoms of liver disease
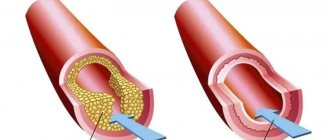
Symptoms of liver disease include frequent nausea, heartburn, a very unpleasant, pungent odor of sweat, yellowish skin color, dark yellow urine, diarrhea, discoloration of feces to dark brown or light yellow, sometimes green. Also, liver disorders can lead to acne in adulthood, frequent feelings of hunger or strong and frequent thirst, itching of some thin areas of the skin, and blurred vision. For example, a person may begin to confuse white with yellow, suddenly feel either cold or hot, and cannot sleep at night, experiencing fever and rapid heartbeat. Hair and eyebrows may begin to fall out. Convulsions occur, papillomas form, and the development of atherosclerosis of the brain, heart, intestines, and blood vessels of the legs begins.
Typical cases of organic and functional liver problems are easily recognized by their characteristic symptoms. But some situations make it difficult for even experienced hepatologists (specialists who deal with liver diseases) to make a correct diagnosis. It all depends on the specific type of disease, the individual characteristics of the body, the presence or absence of concomitant pathology.
- Discomfort and pain in the projection of the liver;
- Enlargement of the liver;
- General weakness and malaise;
- Headache;
- Impaired mental and thinking abilities;
- Increased skin sweating and swelling;
- Yellowness of the skin and sclera;
- Skin rash;
- Increased fragility of blood vessels and tendency to bleeding;
- Signs of hypovitaminosis;
- Stool instability, changes in the nature and color of stool;
- Increase in abdominal size;
- Increased venous pattern on the skin of the abdomen;
- Unmotivated weight loss;
- Bitterness in the mouth;
- Cracks on the surface of the tongue and its coating with a white or brown coating;
- Temperature reaction of varying severity.
Pain due to liver damage can be of a different nature. They can be interpreted like this:
- Minor pain in the right hypochondrium in the form of aching pain, bloating and heaviness. Characterize a sluggish pathological process of inflammatory toxic or other origin. This type of pain in the liver is most likely caused by an increase in the size of the organ and overstretching of the liver capsule. Patients cannot clearly identify one pain point;
- Intense widespread pain in the right hypochondrium. They are rare and speak of either a pronounced inflammatory, purulent, traumatic pathological process, or damage to the bile ducts by stones;
- Severe local point pain in the projection of the liver. It is not typical for liver damage and in most cases is associated with pathology of the gallbladder and extrahepatic bile ducts;
- Complete absence of pain in the liver. It is very common in indolent liver diseases, which remain undetected for a long time and are detected only at the stage of liver failure or cirrhosis.
Based on the characteristics of the skin, one can determine the functioning of various organs, including the liver.
With such diseases, the skin may be:
- Pale or dark-skinned with severe sweating and swelling of the subcutaneous tissue, especially in the face and limbs;
- Dry, flaky with multiple scratch marks and cracks;
- Jaundice. By the nature of this type of skin changes, one can determine the origin of jaundice. In case of liver problems, jaundice is of moderate intensity and is represented by an orange tint. When carrying out the differential diagnosis of jaundice, this criterion allows us to exclude mechanical types (brown skin tone) and hemolytic types, accompanied by a lemon-yellow skin tone;
- With the presence of striae. Striae are stretch marks of the skin, mostly of the abdomen, in the form of bluish stripes of thinning. The reason for their appearance is a hormonal imbalance, both in the male and female body, when the liver is not able to neutralize excess steroid hormones.
In most patients with liver pathology, along with changes in skin color, various rashes appear.
- Pustular elements, tendency to folliculitis and furunculosis. They are based on an immune imbalance that occurs against the background of a decrease in the liver’s ability to synthesize immunoglobulins;
- Allergic rash of the type of spots and papules. It is caused by a violation of the detoxification function of the liver, which underlies the occurrence of allergic reactions to environmental conditions familiar to the body;
- Hemorrhagic rash. Small hemorrhages over the entire surface of the skin, which are called petechial rashes, are typical manifestations of a decrease in the synthetic function of the liver. First of all, the proteins that make up the blood coagulation system are affected. Such patients have an increased tendency to form hematomas at the slightest injury.
It is characteristic that any type of skin rash in liver diseases is accompanied by severe itching. It becomes especially persistent when yellowing of the skin is combined with rashes. This symptom is explained by the fact that bilirubin, which is not neutralized by the liver, is deposited in the skin, causing irritation. In addition, other toxic metabolic products are concentrated in the wide microcirculatory network of the skin, which additionally causes irritation and itching. In this regard, when examining patients with liver pathology, you can notice scratch marks, especially on the lateral surfaces of the abdomen and forearms.
What are diffuse changes in the pancreas?
A pathogenic change in tissue can be chronic and not manifest itself for a long time.
In older people, especially with pathologies of the cardiovascular system, blood circulation, and those suffering from diabetes, healthy pancreatic tissues often die under the influence of pathogenic circumstances, and in their place connective or adipose tissue is formed.
This condition is not recognized as a disease and therefore cannot be treated. But ultrasound shows increased echogenicity with normal organ sizes. Such transformations are observed in the following violations:
- blood supply to the enzyme-forming organ
- functioning of the biliary tract
- liver function
- metabolic and endocrine processes.
Similar symptoms are characteristic of pancreatitis and dystrophic metabolic disorders. If the diagnosis of pancreatitis is not confirmed, then DIP is not recognized as a disease and treatment is not prescribed. The object of spreading changes, as a rule, is the pancreatic parenchyma, that is, the glandular tissue that performs the main functions of the organ. A pathogenic change in tissue can be chronic and not manifest itself for a long time.
Diet
In case of diffuse changes in the liver, it is necessary to follow a special diet. In fact, healthy eating rules are not difficult to follow. It is more difficult to overcome psychological dependence on harmful products. Willpower, a positive attitude and a healthy, varied menu help with this.
The following foods, drinks and dishes must be excluded from the patient’s menu:
- black tea, coffee;
- tomatoes and juice from them;
- any alcoholic and low-alcohol drinks;
- sweet soda;
- fat meat;
- any strong broths;
- barley, millet, pearl barley;
- mayonnaise and other fatty sauces;
- sausage and any smoked meats;
- fatty fish;
- white bread and baked goods;
- fatty fermented milk products;
- marinades, salted and spicy vegetables;
- mushrooms;
- legumes;
- fresh berries and fruits;
- chocolates and other confectionery products;
- spices.
In case of diffuse changes in the liver, it is necessary to eat such dishes and drinks as:
- weak green tea, dried fruit compote, rosehip decoction;
- rye and bran bread, crackers from it, unsweetened biscuits;
- dietary meat: chicken, turkey, rabbit, veal;
- lean fish - pike, pike perch, cod;
- vegetable oil and butter in small quantities;
- skim milk and dairy products;
- eggs;
- boiled and stewed vegetables;
- buckwheat, oatmeal, rice porridge;
- leaf salad;
- fresh bell pepper;
- pasta;
- marmalade, honey, fruit jam.
You need to eat small portions 5-6 times a day. Preference should be given to steamed, boiled and baked products. Soups and aspic are prepared from lean meat and fish. You can eat a small amount of squash caviar, vinaigrette, and sauerkraut. Sugar is replaced with xylitol. The amount of salt should not exceed 3 grams per day.
Read also
Hyperprolactinemia
Hyperprolactinemia is a persistent increase in the level of the hormone prolactin in the blood.
Hyperprolactinemia syndrome is a complex of symptoms that occur against the background of increased prolactin levels, the most characteristic... Read more
Thyrotoxicosis (hyperthyroidism)
Physiology of the thyroid gland: The function of the gland is to synthesize and secrete thyroid hormones. An increase in their number leads to more intense metabolism and vice versa. Thyroid function is regulated...
More details
Complications of diabetes
Diabetes mellitus (DM) is a systemic disease caused by absolute (type 1) insulin deficiency or insulin resistance (type 2), which causes impaired carbohydrate metabolism, manifested by chronic...
More details
Pheochromocytoma
Pheochromocytoma is a tumor of the adrenal medulla that produces catecholamines (adrenaline, norepinephrine, dopamine). Pheochromocytoma consists of chromaffin cells. Pheochromocytoma may have...
More details
Itsenko–Cushing syndrome
Itsenko-Cushing syndrome is a disease that occurs against the background of chronic hypercortisolism, i.e., an increased level of the hormone cortisol in the blood secreted by the adrenal cortex, or long-term treatment...
More details
Complications
Without timely and adequate treatment, diffuse nodular goiter can lead to serious consequences. Therefore, doctors recommend seeking professional help immediately if you discover 3 or more signs of the disease. An advanced stage of diffuse nodular goiter increases the risk of malignancy of the process and the development of thyroid cancer. It often leads to death.
Other complications are possible with diffuse nodular goiter. Choking, problems with swallowing, compression of nerve endings and metabolic disorders can negatively affect the condition of many internal organs and systems.
Prevention
To prevent DI, you need to completely abstain from alcohol.
How quickly DI will develop in the pancreas, and possibly also in the liver and other organs, depends on the patient. The process of dying of parenchymal cells can be slowed down if you follow simple rules:
- Completely abstain from alcohol;
- Develop a proper diet, eat often and in small portions;
- Minimize the consumption of fatty foods;
- Drink herbal teas and fruit juices prepared with your own hands;
- Avoid canned foods in any form.
DIPJ is not a death sentence. There is no reason to panic. Typically, such distortions indicate normal processes occurring in the body. But if DI is detected against the background of pain, then it is necessary to undergo further examination and be more attentive to yourself and your body.
Non-drug treatment
Therapy for any diseases of the heart and blood vessels should begin with lifestyle modification and the elimination of bad habits. The basic principles are:
- Rational nutrition and diet. Diet therapy in the presence of diffuse changes requires excluding fatty, fried, smoked foods from the diet, minimizing animal fats and increasing the consumption of vegetable fats. Refusal of pickled foods and overly seasoned dishes. Particular attention should be paid to the diet of people with high blood cholesterol levels and chronic coronary heart disease.
- Dosed physical activity. Physical activity is very important for the normal functioning of the heart muscle. However, it should be remembered that weightlifting and physical overload cause hypertrophy of the heart muscle, which increases its need for oxygen. Therefore, physical activity should be moderate. Walking in the fresh air, a short jog, and exercise in the morning are enough.
- Quitting alcohol and smoking.
- Correction of blood pressure when it increases by limiting salt and water intake.
- Weight correction for obesity under the strict supervision of a nutritionist.
- Normalization of work and rest schedules, full 8-hour sleep.
List of sources
- Gubergrits N. B., Linevskaya K. Yu., Belyaeva N. V. Differential diagnosis in gastroenterology. From symptom and syndrome to diagnosis and treatment: practical work. hands - Kyiv: Trush E. N. [ed.], 2021. - 623 p.
- Danilov M.V., Fedorov V.D. Pancreatic surgery. Guide for doctors. M.:b Medicine, 1995. 312 p.
- Zakharova O.P., Egorov V.I., Karmazanovsky G.G. Surgical treatment of pancreatic tumors: computed tomographic criteria for resectability. Annals of surgical hepatology. 2011. 16. No. 1. pp. 84-91.
- Zimmerman Ya.S. Chronic pancreatitis // Bulletin of the Pancreatology Club. - 2009. No. 1. - P. 38-47.