Heart Attack Symptoms
Because cardiogenic shock typically occurs in people who have had a severe heart attack, it is important to know the signs and symptoms of a heart attack. These include:
- Pressing, bursting or squeezing pain in the chest lasting more than 15 minutes;
- Pain radiating to the shoulder, arm, back or teeth and lower jaw;
- Increased frequency of attacks of chest pain;
- Prolonged pain in the upper abdomen;
- Dyspnea;
- Sweating;
- A looming feeling of fear;
- Fainting;
- Nausea and vomiting.
If you see your doctor right away when these signs or symptoms appear, you can prevent the possibility of developing cardiogenic shock. Prompt treatment of a heart attack increases the chances of survival and reduces damage to the heart. Don't ignore these symptoms if they last more than five minutes. Call an ambulance immediately. If you cannot call an ambulance, ask someone to take you to the nearest hospital.
Resuscitation measures
In case of loss of consciousness and respiratory arrest, urgent resuscitation measures must be performed. Artificial respiration is performed mouth to mouth. To do this, the person’s head needs to be tilted back, placing a cushion made of a towel or any other fabric under the neck. The person performing resuscitation must inhale air, cover the victim's nose with his fingers, and exhale air through the victim's mouth. You need to take up to 12 breaths in one minute.
During the provision of first aid, it is necessary to monitor the patient’s pulse. If a person loses consciousness and heartbeats cannot be heard, chest compressions must be performed. To perform it, the patient is placed on his back, the surface must be hard. The person performing the massage should position himself to the side of the patient. The heels of your palms should press down on the chest area in the middle. Pushes are performed with straight arms; there is no need to bend them. The frequency of pressing is at least 60 shocks per minute. If an elderly person is being resuscitated, the number of pushes per minute is up to 50, for children - 120 pushes. Important! When performing artificial respiration and chest compressions simultaneously, you should alternate 2 breaths with 30 shocks.
Causes
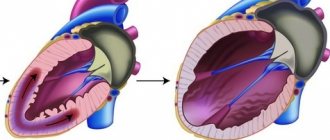
Cardiogenic shock occurs when the heart loses its ability to pump enough blood to the rest of your body. The most common cause of cardiogenic shock is damage to the left ventricle, the main pumping chamber of the heart, due to lack of oxygen due to a heart attack.
A heart attack occurs when one or more of the arteries that carry oxygenated blood to your heart (coronary arteries) becomes blocked. Sometimes, over time, a narrowing of the coronary arteries occurs due to the deposition of cholesterol on their walls. The formation of these deposits, called plaques, in the arteries throughout the body is called atherosclerosis.
During a heart attack, one of these plaques may rupture, forming a blood clot at the site of the rupture, blocking blood flow through the arteries. Without oxygenated blood entering the heart, the heart muscle weakens and cardiogenic shock develops.
In rare cases, cardiogenic shock develops when the right ventricle of the heart is damaged. From the right ventricle of the heart, blood travels to the lungs, where it is enriched with oxygen before being sent to the rest of your body. Damage to the right ventricle causes the heart to lose its ability to pump blood effectively to the lungs, causing the body to not receive enough oxygen.
Although a heart attack is the most common cause, other conditions that cause cardiogenic shock include inflammation of the heart muscle (myocarditis) or infection of the heart valves (endocarditis). Causes include drug overdose or poisoning from substances that affect the pumping function of your heart.
Classification
Classification of cardiogenic shock according to the severity of the patient’s condition involves three forms:
| Clinical manifestations | 1st degree (mild) | 2nd degree (moderate) | 3rd degree (severe) |
| Duration of shock | less than 5 hours | from 5 to 8 hours | more than 8 hours |
| Blood pressure in mm Hg. Art. | at the lower limit of normal 90/60 or up to 60/40 | upper at 80-40, lower at 50-20 | not defined |
| Tachycardia (beats per minute) | 100–110 | up to 120 | dull tones, threadlike pulse |
| Typical symptoms | weakly expressed | left ventricular failure predominates, pulmonary edema is possible | pulmonary edema |
| Response to treatment | good | slow and unstable | absent or short-term |
Complications
If not treated promptly, cardiogenic shock becomes a fatal condition. Another serious complication of cardiogenic shock is organ damage.
If the heart cannot pump enough oxygenated blood to the rest of your body, damage to the liver, kidneys and other organs develops. When the liver and kidneys are damaged, cardiogenic shock is worsened because the kidneys release chemicals into the blood that support muscle function and the liver produces proteins that help blood clot. With long duration of cardiogenic shock, permanent organ damage can develop.
Diagnostic methods
Diagnosis of cardiogenic shock requires immediate action. Doctors will check for signs and symptoms of shock and then order additional tests to determine the cause of your condition. Methods for diagnosing cardiogenic shock include:
- Blood pressure measurement. People with shock often have low blood pressure. If a person in shock is taken to hospital by ambulance, blood pressure is measured before admission to hospital.
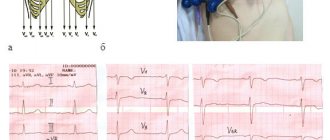
- Electrocardiogram (ECG). This is the first test to diagnose a heart attack. It is often done at the same time as a survey about symptoms. The test involves recording the electrical activity of the heart using electrodes attached to the skin. The pulses appear as "waves" displayed on a monitor or printed on paper. Because the heart muscle cannot conduct electrical impulses normally when damaged, an ECG can help determine whether you are having a heart attack or are in the process of having one.
- X-ray of the chest organs. A chest x-ray will help your doctor evaluate the size and shape of your heart and its blood vessels.
- Blood tests. Blood tests can determine if you have kidney or liver damage, detect signs of heart infection, and also determine if you are having a heart attack. Another type of blood test (arterial blood gas test) is also ordered to determine the amount of oxygen in the blood.
- Echocardiogram. This test uses sound waves to produce images of the heart. During echocardiography, sound waves are sent to the heart from a wand-shaped device (transducer) placed on the chest. Sound waves bounce off the heart and back through the chest and are processed electronically to produce a video image of the heart. An echocardiogram can help identify areas of damage to your heart and problems with the heart's pumping function.
- Catheterization of coronary arteries (angiography, coronary angiography). This test will look for narrowing and blockage of the coronary arteries. Liquid contrast dye is injected into the arteries of the heart through a long, thin tube (catheter) that is passed through an artery in the leg or arm to the arteries of the heart. As the contrast agent fills the arteries, they become visible on X-rays, revealing areas of blockage.
Additionally, during catheterization, your doctor may remove the blockage in the artery through coronary angioplasty and stenting. Angioplasty uses tiny balloons that are inserted through a blood vessel into the coronary artery to widen the blocked area. After angioplasty, a mesh tube (stent) is placed inside the artery to maintain sufficient lumen and prevent re-narrowing in the future.
Cardiogenic shock
A lack of blood supply to tissues can be caused by severe heart pathologies, in which the pumping function of the myocardium is impaired. This could be a heart attack, cardiogenic shock, acute blood loss, or another condition requiring emergency medical attention. At the same time, cardiogenic shock can also develop as a complication of primary cardiovascular pathologies.
What is cardiogenic shock?
In the medical literature, cardiogenic shock is an acute disorder of the blood supply to organs caused by severe impairment of the pumping function of the heart. This is a serious and often fatal condition that develops in acute and chronic diseases. In particular, cardiogenic shock may be associated with left ventricular failure.
To understand the mechanism of development of this condition, it is necessary to have an understanding of the functioning of the cardiovascular system. The heart is a powerful four-chamber muscular pump, thanks to whose contractions blood enriched with oxygen and nutrients is supplied to all tissues of the body. Rhythmic heartbeats are controlled by the internal conduction system of the myocardium and external influences. If the contraction force is insufficient, the rhythm is inconsistent or another disorder of the heart activity occurs, hemodynamic disturbances occur and the organs receive an insufficient amount of blood.
Main criteria for cardiogenic shock:
- Ineffectiveness of the pumping function of the myocardium.
- Myocardial ischemia against the background of an increase in heart rate.
- Deterioration of renal perfusion.
- Edema of the lung tissue.
- Hypoxia and metabolic changes in tissues.
Cardiogenic shock is a rare condition that develops against the background of severe pathologies of the heart and blood vessels. Irreversible changes in organs associated with insufficient blood supply can develop within the first minutes of an attack. Emergency resuscitation is almost always required.
8
24/7
State forms
In most patients, cardiogenic shock, characterized by low blood pressure and inadequate blood supply to organs, is caused by either insufficient cardiac output or low systemic vascular resistance. Depending on the cause of occurrence, there are four main forms of pathology:
- Actually cardiogenic shock, characterized by primary myocardial dysfunction and insufficient efficiency of the muscle pump. Signs of this form include tachycardia, insufficient capillary refill, hypotension and increased sweating.
- Hypovolemic shock is an acute disorder of the cardiovascular system caused by significant blood loss.
- Obstructive shock is a consequence of impaired blood circulation through the vessels as a result of pericardial tamponade, blockage or dissection of an artery.
- Distribution shock. This form of the disorder is usually caused by the accumulation of blood in the venous section. Patients with distributive shock have high cardiac output, low blood pressure, and good capillary refill.
Clarifying the form of the disorder is important for providing first aid.
Causes
As a rule, cardiogenic shock is the result of damage to cardiac structures or vascular pathologies.
Main reasons:
- Left ventricular failure of the heart, characterized by low blood output.
- Organic damage to the myocardium as a result of ischemic disease, heart attack, chest injury or surgery.
- Significant blood loss and improper distribution of blood in the body.
- Inflammation of the muscle tissue of the heart.
- Infection of the heart valves.
- Congenital defects of the heart structure.
- Taking narcotic and toxic drugs that can affect myocardial function.
The following risk factors are also important:
- Age from 55 years.
- History of chronic diseases of the cardiovascular system and lungs.
- Family history of heart disease.
- Diabetes mellitus and high blood pressure.
- Female.
These factors may increase the likelihood of developing cardiogenic shock, but are not the direct causes of the condition.
Symptoms and signs
Symptoms depend on the cause, the severity of the patient’s condition and other factors. Often, signs of shock are combined with symptoms of previous pathologies.
Main manifestations:
- Fast breathing.
- Severe shortness of breath.
- Sudden increase in heart rate (tachycardia).
- Loss of consciousness.
- Weak pulse.
- Low blood pressure.
- Excessive sweating.
- Cold hands and feet.
- Dizziness and nausea.
You should also consider the following signs of myocardial infarction, which may precede a state of shock:
8
24/7
- Feeling of heaviness in the chest.
- Prolonged chest pain. Also sometimes described as a squeezing pain in the center of the chest.
- Irradiation of pain to the area of the upper extremities, back, neck and lower jaw.
- Breathing problems.
- Dizziness.
- Nausea and vomiting.
If such signs appear, you should immediately seek medical help.
Diagnostic methods
Cardiogenic shock, for which emergency assistance is required already in the first minutes after the attack, is diagnosed in the intensive care unit or intensive care unit. Doctors need to quickly find out the cause of the pathology, the clinical picture and the severity of the patient’s condition. At the first aid stage, shock is identified by symptoms and objective signs, including auscultation data, low blood pressure, weakened pulse and impaired consciousness. In the hospital, instrumental and laboratory tests will be required to confirm the diagnosis and identify the etiology of the disease.
Special diagnostic methods:
- Electrocardiography – registration of the bioelectrical activity of the heart. To do this, special electrodes connected to a cardiogram recording device are placed on the patient’s body. Based on the test results, one can judge the presence of a structural pathology that prevents the normal propagation of an impulse in the myocardium.
- Echocardiography is the main imaging method in cardiology. Ultrasound technology is used to send high-frequency sound waves to the heart and form an image. Monitoring the heart's performance on a monitor in real time allows you to detect the pathological area and assess the degree of pumping dysfunction.
- Vascular X-ray – visualization of the blood vessels of the heart. As a rule, this method is used to find the root cause of the development of a state of shock. Before taking the image, the doctor injects a contrast agent intravenously to improve the accuracy of the study. Based on the results of coronary angiography, one can judge the cause and degree of narrowing of the vessel.
- Blood test for infectious disease, toxicology and enzymes indicating damage to the muscular lining of the heart.
- Computed tomography and magnetic resonance imaging are methods for obtaining images of the heart and blood vessels in high resolution. This is the most effective method for detecting the affected area in the heart.
The patient’s life depends on the timeliness and completeness of the diagnostic search.
Treatment options
Medical care for cardiogenic shock should be aimed at restoring the pumping function of the heart, improving blood supply to organs, eliminating the root cause of the condition and eliminating complications. As a rule, the patient’s condition is initially stabilized in intensive care to restore vital functions and is subsequently sent for treatment of the underlying cause of the condition. This may be drug or surgical treatment.
Therapeutic purposes:
- Connecting the patient to a mechanical ventilation system to saturate the body with oxygen.
- Intravenous infusion of saline, plasma or blood to eliminate hypovolemic shock.
- Administration of inotropic drugs to improve the pumping activity of the myocardium. It could be norepinephrine or dopamine.
- Aspirin to reduce blood clotting. In a state of shock, there is a risk of vascular blockage.
- Thrombolytic agents needed to dissolve blood clots blocking blood flow to organs. The sooner a patient with a heart attack receives such a drug, the better the prognosis.
- Antiplatelet drugs, which are aimed at preventing the formation of new blood clots.
Also, cardiogenic shock, the clinical picture of which is associated with hypoxia of the muscle cells of the heart, requires special medical procedures to restore blood flow. The following methods are used:
- Angioplasty and stenting – removal of blockage or narrowing of the coronary arteries.
- Extracorporeal membrane oxygenation – mechanical support of blood circulation and oxygen saturation of organs.
Surgical methods of treatment:
- Coronary artery bypass surgery to create a bypass of blood flow past the area of narrowing or blockage.
- An operation aimed at restoring the heart and blood vessels after injury.
- Implantation of assistive devices that improve pumping function.
- Heart transplant if other methods do not help.
It is important to understand that cardiogenic shock, the treatment of which is not always effective, is a complication of severe previous diseases, including myocardial infarction. Timely seeking medical help when the first symptoms appear significantly improves the prognosis.
8
24/7
Medications
Medicines to treat cardiogenic shock are prescribed to improve blood flow through the heart and improve the pumping function of your heart.
- Aspirin. Aspirin reduces blood clotting and maintains blood flow through the narrowed artery. Take aspirin on your own while waiting for emergency services to arrive, only if your doctor tells you to do so if you are experiencing symptoms of a heart attack.
- Thrombolytics. These drugs help dissolve a blood clot that is blocking blood flow to the heart. The sooner you are given a thrombolytic drug during a heart attack, the better your chance of survival and less damage to your heart. Thrombolytics are prescribed if emergency catheterization of the heart arteries and stenting cannot be performed.
- Antiplatelet agents. Doctors in the emergency room may give you other drugs that are similar to aspirin to prevent new blood clots from forming. These include drugs such as clopidogrel (Plavix) and other platelet glycoprotein IIb/IIIa receptor blockers.
- Other blood thinning drugs. You will likely be prescribed other medications. These include heparin, to reduce the likelihood of dangerous blood clots. Heparin is given intravenously or subcutaneously for the first few days after a heart attack.
- Inotropic drugs. Dopamine or epinephrine is prescribed to improve and maintain heart function.
Surgical interventions
Surgery to treat cardiogenic shock aims to restore blood flow through the heart. They are performed in specialized cardiac centers. Such interventions include:
- Angioplasty and stenting. Typically, when blood flow through the blocked artery is restored, the signs and symptoms of cardiogenic shock improve. Emergency angioplasty works to clear blocked arteries, allowing blood to flow freely to your heart. Doctors insert a long, thin tube (catheter) that is threaded through an artery in your leg or arm to the blocked artery in your heart. This catheter is equipped with a special balloon. When installing a stent in the area of narrowing, the balloon is inflated to restore the lumen of the artery. In addition, a metal mesh stent may be inserted into the artery to keep it open for a long time and restore blood flow to the heart. Doctors install stents that slowly release drugs into the blood to keep the artery wide enough.
- Balloon pump. Depending on your condition, doctors may place a balloon pump in your heart's main artery (aorta). The balloon pump inflates and deflates to mimic your heart and keep your blood flowing.
Operations
If drug treatment and the listed surgical interventions are ineffective, the doctor will recommend surgery:
- Coronary artery bypass grafting. Bypass surgery involves sewing veins or arteries to bypass the area of blockage or narrowing of the coronary artery. This restores blood flow to the heart. The doctor will suggest this surgery after the heart has recovered from a heart attack.
- Surgeries to repair heart damage. Sometimes the cause of cardiogenic shock is a rupture of one of the chambers of the heart or damage to the heart valve. To correct these problems, the doctor will suggest surgical treatment.
Pre-hospital emergency care
If signs of cardiogenic shock are detected, it is necessary to call an ambulance as soon as possible and provide emergency assistance to the person. To do this, follow these steps:
- Place the patient on any surface, the body should be in a horizontal position, legs slightly elevated. This position ensures better blood flow to the brain.
- During emergency care, it is important to provide fresh air into the room. To do this, you need to open the window or front door. Crowds should not be allowed near the victim.
- The person's neck and chest must be freed from clothing. If there is a tight collar, tie, scarf or other items, they should be removed.
- At the initial stage, you need to measure the patient's blood pressure. In cardiogenic shock it is always reduced. To normalize the indicators, you need to give the patient a drug that contains dopamine, metazone or hydrocartisone.
- If the person is conscious, taking analgesic medications is allowed.
After this, you should wait for the ambulance, and after the doctors arrive, tell them under what circumstances the shock developed.
First aid for the development of shock should be immediate.
Prevention
The best way to prevent cardiogenic shock is to prevent heart attacks. Lifestyle changes used to treat heart disease can help prevent a heart attack. These lifestyle changes include:
- Control of high blood pressure (treatment of hypertension). One of the most important steps to reduce your risk of heart attack and cardiogenic shock is to control your blood pressure. Regular exercise, managing stress, maintaining a healthy body weight, and limiting salt and alcohol intake will help control high blood pressure. In addition to recommendations for lifestyle changes, your doctor may prescribe medications to treat hypertension, such as diuretics, angiotensin-converting enzyme (ACE) inhibitors, or angiotensin receptor blockers.
- To give up smoking. Quitting smoking reduces the risk of having a heart attack. Several years after quitting smoking, a smoker's risk of developing a stroke is the same as a non-smoker's.
- Maintaining normal body weight. Excess weight contributes to the risk factors for heart attack and cardiogenic shock: high blood pressure, cardiovascular disease and diabetes. Losing just 10 pounds of weight will lower your blood pressure and cholesterol levels.
- Reduce cholesterol and saturated fat in your diet. Eating less cholesterol and fat, especially saturated fat, will reduce your risk of heart disease.
- Regular exercise. Exercise reduces your risk of having a heart attack. Exercise lowers blood pressure, increases high-density lipoprotein (HDL) levels, and improves the overall health of your blood vessels and heart. They will help you lose weight, control diabetes and reduce stress. Get regular exercise such as walking, jogging, swimming or cycling for 30 minutes every day.