A person cannot independently find out whether there is a blood clot. Read the article, it describes diagnostic methods and the first signs of thrombosis.
A thrombus is a collection of white blood cells, red blood cells and platelets that form a clot that blocks the flow of blood. Localized in the veins and arteries of various organs. If a blood clot blocks a vein or artery, it is a major health hazard and can even be fatal. In this article, we will look at how to find out if there is a blood clot in the body, how to diagnose it, and how to help a loved one if the blood clot has broken loose.
How to find out if a person has blood clots in the body in the vessels: symptoms, signs
Thrombus
A thrombus is a blood clot that completely or partially closes the lumen of a vessel, formed due to stagnation of blood in various organs. Thrombosis is a disease in which the presence of blood clots in the human body is confirmed by a doctor.
Important: This diagnosis should only be made by a doctor. If you notice the first signs or symptoms, you should immediately consult a doctor.
So how can you tell if a person has blood clots in their blood vessels? Some symptoms indicate this, but depending on the location of the blood clot in a particular organ, they vary significantly. Signs of blood clots in the body and their location:
- In the brain it can cause dizziness, headaches, and fainting.
- In the lower extremities - swelling, bluish skin, bruising.
- In the heart - pain in this organ, arrhythmias, ischemic heart disease, hypotension, shortness of breath, numbness of the hands.
- In other organs there will also be noticeable disruptions in their functioning.
The very presence of blood clots in the body is usually without symptoms, and the person feels unwell only in the organ where the blood clot is located. The worst thing is a complication, namely the detachment of a blood clot.
Remember: In such cases, there is a high probability of disability and death. The process occurs rapidly, in most cases minutes count - heart attack, stroke, pulmonary embolism, failure of other organs.
In such cases, a person needs urgent medical attention. The administration of necessary medications should be carried out as soon as possible and only by qualified personnel to avoid complications.
Contraindications to vascular MRI
A vascular MRI scan should not be performed if the patient has metal objects in the body, such as a pacemaker, insulin pump, or vascular clips. The electromagnetic field from an MRI machine can interfere with the normal functioning of these devices. And parts made of ferromagnets move and heat up under the influence of a magnet.
It is allowed to undergo MRI with titanium dentures, as well as dental implants and braces made of ceramics, plastic or polymers. Magnets do not work on these materials.
If the patient is afraid of closed spaces, the procedure can be performed in a state of medicated sleep.
How to determine whether there are blood clots in the legs, is a blood clot in the leg dangerous?
thrombus
is a blood clot that completely or partially blocks the flow of blood in the vessels. Thrombophlebitis or thrombosis is the presence of a blood clot in the vessels of the legs. Is a blood clot in the leg dangerous? It all depends on the complexity of the disease and the location of the blood clot. There are diseases associated with the formation of blood clots:
- Thrombophlebitis, thrombosis - causes inflammation and subsequent necrosis of nearby tissues, the temperature of the affected area is usually increased.
- Phlebothrombosis is when one or more blood clots are located in the veins of the lower extremities. With this disease, the temperature of the affected area is normal or the limbs may even be cool.
- Thrombosis can be arterial or venous . The difference lies in the mobility of the formed blood clots. So, in the first case, the probability of mobility of clots is high. In the second, it is practically reduced to zero, due to the lack of pressure and the presence of valves in the veins, which are an additional barrier to the mobility of blood clots.
A blood clot in the leg is dangerous because it poses a health threat. If a doctor diagnoses such a disease, the patient is first prescribed drug treatment, so that the blood clot should resolve on its own. If this does not happen, blood clots are “broken” using modern technologies: laser and other techniques.
How to determine if there are blood clots in the legs:
- A person may suspect this disease if he has swelling and cyanosis, usually of one leg.
- Only a doctor can diagnose the presence or absence of the disease using ultrasound.
- If the diagnosis is confirmed, treatment is prescribed.
Remember: All of the above diseases are dangerous, because if left untreated, they can lead to gangrene, and ultimately the loss of a limb.
In addition, with the blood flow, clots can move to other organs and cause their failure and lead to death.
Call your doctor or nurse if you have:
- pain has intensified, swelling has increased, or both of these symptoms are observed on the arm or leg where the blood clot has formed;
- there is pain, swelling, or both of these symptoms on the other arm or leg;
- breathing problems;
- severe or persistent headache;
- nosebleeds;
- bleeding gums;
- blood in your urine, stool (feces), vomit, or sputum you cough up through your mouth;
- heavier menstrual bleeding than usual;
- continuous bleeding;
- a bruise that does not go away;
- you fell or were injured in any way;
- you are planning a dental procedure or surgery;
- you stop taking your blood thinner for any reason;
- unexpected, unexplained side effects occurred;
- have any questions or concerns.
to come back to the beginning
Blood clot in the heart: what is it, symptoms, what to do?
Blood clot in the heart
If a blood clot is located in the vessels of the heart, then if it breaks off, it can lead to a heart attack, or its free movement to other organs and blockage of blood vessels. When a blood clot appears in the left atrium, the patient may experience the following symptoms:
- Fainting
- Numb hands
- Dyspnea
- Low blood pressure
- Heartache
- Pale skin
If a blood clot is found in the heart on the right:
- Cyanosis or blueness of the skin
- Dyspnea
- Weakness
- Hand tremors
- Nausea
The thrombus can move between the ventricles or be attached to a certain place by a kind of stalk. What to do at the first symptoms of a blood clot in the heart?
- Providing first aid consists of calling an ambulance.
- Providing assistance on your own is prohibited!
- The risk of an acute condition resulting in the death of the patient within a few minutes is very high.
- Therefore, the speed of providing qualified medical care is important.
Upon arrival, doctors immediately administer anticoagulants, for example:
- Heparin
- Enoxaparin
- Nadroparin
- Dalteparin
The patient should also receive treatment with fibrinolytics:
- Thromboflux
- Streptokinase and others
Important to know : If a person notices the first symptoms of such an ailment, it is necessary to urgently call doctors, otherwise the consequences may be irreversible.
How to check if there are blood clots in the heart?
Ultrasound of the heart
Stagnation of blood in the body leads to such a serious disease as thrombosis. It is difficult to identify immediately or independently, due to the lack of obvious symptoms. But how can you check if there are blood clots in the heart?
The patient should consult a doctor if he is concerned about:
- Chest pain
- Dyspnea
- Tachycardia
With a moving thrombus, the following are possible:
- Frequent fainting
- Pale skin
- Suffocation
- You may also feel dizzy often
- Break out in a cold sweat
To check whether there are blood clots in the heart, the cardiologist refers to the following types of diagnostic procedures:
- Ultrasound of the heart.
- Ultrasound of the abdominal cavity.
- Echocardiography.
- X-ray of the heart.
- Scintigraphy - shows what is happening inside the blood vessels and their position in the body.
- Dopplerography - measures heart pressure, speed, direction of blood flow in this organ.
- MRI helps to see the heart from the inside and determine the presence of a particular disease.
You should know: Call an ambulance immediately if a person experiences sharp, severe chest pain and blurred vision. Without timely medical care, a blood clot can break off and lead to a heart attack, stroke, or death.
Risk factors for thrombosis
Certain circumstances may increase the risk of blood clots. The following risk factors are identified:
- Sedentary lifestyle. With little physical activity, blood flow in your deep veins slows down, which can lead to blood clot formation.
- Recent surgeries. Some surgeries may cause your blood to become thicker, or it may become stagnant if you have surgery and a long period of bed rest.
- Injuries.
- Some cancers.
When you are an inpatient, you may be exposed to more than one of these risk factors at the same time.
to come back to the beginning
Can a blood clot break off: is it dangerous, does a blood clot hurt?
Thrombus in the leg
As mentioned above, a thrombus is a clot of red blood cells, leukocytes and platelets that block the lumen of the vessel partially or completely. It depends on how it is attached:
- Parietal - attached to one side of the vessel wall.
- Central - located in the center and blood flows around it.
- Lining - encircles the vessel.
Does a blood clot hurt? Such a blood clot can be felt if it is in the superficial veins of the legs, in the form of a compaction. The surrounding tissues have a bluish tint. When you press on the damaged area, a sharp pain syndrome occurs.
Is a blood clot dangerous? Can it come off? It is dangerous when it is torn off, as it can block a vessel leading to a specific organ, causing negative consequences for the entire body as a whole.
This is why a detached blood clot is dangerous - pathologies, the consequences of which can be irreversible:
- Stroke occurs when a blood vessel in the brain is blocked.
- A heart attack is when a blood clot enters the heart.
- Pulmonary thromboembolism - when a blood clot migrates to the lungs.
- Swelling, inflammation of the tissues of the legs and the development of subsequent gangrene, threatening amputation.
- Failure of the liver, kidneys.
We have all been hearing about the danger of such a pathology for a long time. Doctors talk about this from TV screens. Therefore, when the first signs or unpleasant pain symptoms appear, you should immediately contact a doctor for examination and diagnosis.
A blood clot has broken off - how to find out: can you feel and see a blood clot, is it possible to save a person?
Thrombus
Only a doctor can see the presence of a blood clot using ultrasound diagnostics. It is almost impossible to feel it, but you can only feel the consequences of its presence in the body. Also, when you press on the skin in the area where the blood clot is located, you will feel pain.
If a blood clot breaks off, how can you tell, can you feel it or see it? If an attached blood clot has come off, you can tell by the person’s condition. Depending on the location of the vessel, painful symptoms may be as follows:
- In the brain , this will lead to a stroke. As a result, asymmetry of facial features, difficulty swallowing, and unclear speech.
- heart attack is possible in - pressing, sharp pain in the chest, or complete blockage of the heart vessels, which leads to death.
- In the intestines - a feeling of sharp pain in the abdomen and peritonitis.
- If a blood clot has blocked a vessel in the leg , swelling, blueness, redness, and severe pain are observed. In the absence of proper treatment - gangrene and amputation.
- Blockage in the lungs , also known as pulmonary embolism, is an acute condition that requires immediate hospitalization. It is characterized by a lack of oxygen, due to which the patient’s skin acquires a blue tint, shortness of breath is observed, and untimely assistance can lead to respiratory arrest and death.
Is it possible to save a person and how to provide first aid?
- An ambulance must be called immediately.
- In this case, painkillers and antispasmodics are important, but they should be taken only as directed by the emergency doctor.
- You also need to help the person find a comfortable position.
Often the correct actions of people around them help a person with an acute condition save a life.
Can a blood clot form after a leg injury, surgery, or blood draw?
Blood clot in the leg
Post-traumatic blood clot formation is not uncommon. Its serious consequences frighten and worry many people. When might he appear? Can a blood clot form after a leg injury, surgery, or blood draw?
- Any strong mechanical impact on the human body can cause damage to the vessel wall.
- Platelets rushing to help release thromboplastin and thrombin. These elements increase blood viscosity.
- In the injured area, a future thrombus is formed from fibrin fibers.
- This is a natural reaction of the body aimed at protecting against blood loss.
Surgical operations, blood drawing, and punctures in the body are directly related to the dissection and injury of blood vessels.
- With excessive platelet activity, the formation of an enlarged clot is inevitable.
- It may not have any negative impact in the future, or it may become a big problem.
- It all depends on the individual characteristics, health status, and lifestyle of the person.
Leg bruises are also not harmless.
- With a strong blow, a hematoma is formed - a bruise.
- This is a manifestation of rupture of small capillaries with slight hemorrhage.
- However, larger vessels located nearby may also be damaged.
To avoid severe outcomes and the development of thrombosis, you need to know the possible causes of blood clots and try to minimize them in your life.
Benefits of MRI
Magnetic resonance imaging is performed without the use of radioactive substances, and therefore does not have harmful radiation effects on the body. This procedure is harmless and can be repeated several times, for example, to monitor the progress of treatment.
MRI, unlike similar research methods, allows you to simultaneously see in the images all parts of the vascular system: both arteries and veins. This feature is necessary when it comes to injuries with large hematomas.
The design of a magnetic resonance imaging scanner allows you to obtain digital images of blood vessels in any projection and with any degree of approximation. After completing the examination, the specialist will have a three-dimensional model of your vascular system, which will allow you to make a more accurate diagnosis and prescribe the correct treatment.
Is it possible to detect and feel a blood clot on your own? Does a blood clot hurt in your leg?
Blood clot in the leg
Thrombosis is one of the serious diseases of the circulatory system. The reasons for the development of this pathology are injuries, surgical interventions, hormonal disorders, and increased blood viscosity. Is it possible to detect and feel a blood clot on your own? Does a blood clot in your leg hurt?
It will not be easy to independently detect a blood clot visually or by palpation. However, if you suspect the presence of blood clots, you should pay attention to the combination of symptoms. Signs of a blood clot in a vein are:
- Tissue swelling.
- Red or bluish areas on the skin near the vessel, their soreness.
- Increased body temperature.
- Pain that increases with movement of the affected limb.
- With long-term absence of treatment, the vascular network begins to stand out significantly.
With thrombophlebitis, superficial thrombosis, the pathological process develops closer to the skin. It will not be difficult for a knowledgeable person to feel a blood clot; upon palpation, the patient will feel pain and discomfort. But the pain syndrome may not appear if a small vessel is clogged and other veins and arteries take over its role.
Remember: There is no need to try to find a blood clot yourself, as this can be dangerous. The blood clot may be loosely attached to the wall of the vein or artery and may break off.
The best solution would be to consult a doctor who will conduct an examination, a series of studies and make an accurate conclusion about your health status.
Functional studies
Functional techniques are the simplest, non-invasive and painless diagnostic measures when studying the lower extremities for vascular diseases. However, due to their obvious limitations, they do not give the doctor an idea of the full picture of the pathology. They are used during initial examinations to determine the presence of the disease and understand what exactly it is associated with. Then the patient is prescribed more in-depth studies aimed at detailing the condition of the organ or tissue.
1. Measurement of the brachial-ankle index - used if vasoconstriction of the lower extremities is suspected. This involves simultaneously measuring blood pressure levels in the shoulder and ankle areas. Normally, their indicators are the same. If the blood supply to the legs is impaired, the pressure in the ankle area is reduced.
2. Rheovasography (RVG) - performed using an electrical device resembling an ultrasound machine. Helps identify abnormalities in the ongoing process of peripheral and cerebral hemodynamics. The specific result is read from the rheogram reflected by the device.
3. Functional tests to detect defects and determine the patency of deep or communicating veins include a set of actions with a variety of motor and palpation manipulations on the part of the doctor and the patient. All that is needed to carry them out is an elastic bandage, a rubber tourniquet, the hands of a doctor and the presence of the patient.
Do people die from a blood clot: mortality statistics
Thrombus
The formation of a blood clot can occur in different parts of the body and it is very difficult to predict where exactly the blood clot is located. At a critical moment, it breaks away and begins to move, which is instantly fatal. People die from blood clots if treatment is not started in a timely manner and the person does not seek the help of doctors for a long time.
- Mortality statistics are such that more people die from thrombosis than from breast or prostate cancer.
- More than 10 million cases of thromboembolism occur worldwide each year.
Smoking, alcohol, and stress can develop this disease. If you want to be healthy, you should pay more attention to physical education, do morning exercises and worry less. It is also necessary to eat properly and drink clean water. This will guarantee your good health.
Is it possible to prevent a blood clot: prevention
Sport is the best prevention of thrombosis.
Every year in Russia alone, hundreds of thousands of people die from stroke. The most common type of stroke is ischemic, caused by a blockage of a blood vessel or a blood clot. It occurs 4 times more often than strokes due to vascular rupture. Is it possible to prevent a blood clot?
- Prevention of thrombosis involves thinning the blood. We need to accelerate it so that there is no stagnation.
- Any physical exercise will help you do this . You should exercise at least 30 minutes a day. It is important to walk a lot in the fresh air.
- People who are inactive most often suffer from stroke , so prevention in the form of daily physical activity is mandatory.
As mentioned above, in order to avoid the appearance of blood clots, you need to follow a drinking regime. You should drink at least two liters of water daily. To be completely sure, you can take medications that improve blood circulation. But this should be done only after consulting a doctor.
Remember : Self-medication is dangerous!
Treatment and prevention of thrombosis
Treatment of thrombosis includes anticoagulant and antiplatelet therapy, thrombolytic therapy, installation of an inferior vena cava cava filter, and surgical removal of the thrombus [5].
Complications of anticoagulant therapy must be kept in mind: major bleeding, heparin-induced thrombocytopenia and warfarin-induced skin necrosis [5]. To reduce the risk of continued thrombus formation, NSAIDs are used [2]. For the purpose of secondary prevention, small doses of heparin are prescribed. Non-drug treatment methods are also prescribed - elastic bandaging, compression hosiery, local hypothermia and exercise therapy [2, 4].
Prevention of thrombosis includes a number of measures used in situations of increased risk of thrombosis.
Primary prevention of atherothrombosis:
- systematic physical activity in the form of walking or morning exercises;
- blood pressure control, maintaining working blood pressure below 140/90 mmHg;
- control of blood sugar levels (less than 6 Mmol/l), early detection and treatment of diabetes mellitus;
- weight loss, body mass index less than 25 kg per m2;
- a diet limited in cholesterol and high-density fat (total cholesterol less than 5 mmol/l), fruits and vegetables;
- smoking cessation [3,7].
Primary prevention of venous thrombosis:
- compression underwear;
- bandaging with elastic bandages;
- drinking plenty of fluids, especially after surgery;
- regular exercise, walking, especially when traveling;
- prohibition of taking alcohol and sleeping pills in large doses;
- prohibition of the use of compressive shoes and clothing [2,5,6].
Sometimes, during periods of particular risk, anticoagulants are prescribed several days before the flight. There is no point in taking aspirin in such cases [5].
If you have blood clots in your legs, can you walk in heels, smoke and drink alcohol?
If you have thrombosis, it is forbidden to wear heels.
We are always told about the dangers of alcohol and smoking on the body. We can say with confidence that these habits provoke the development of thrombosis. For healthy people, as well as for patients with blood clots in the legs, it is harmful to smoke, drink alcohol and for women to walk in heels. Read more below.
Smoking:
- Doctors who often encounter a similar disease have concluded that tobacco plays a big role in the development of thrombosis.
- A person who smokes puts himself at great risk, as the blood thickens and a blood clot can form in the vessels.
- Accordingly, smoking is also harmful in the presence of thrombosis.
Drinking alcohol is also very dangerous for health:
- When a person is in a normal state, his blood moves through the veins at the correct speed.
- As soon as you drink a little strong alcohol, it begins to thicken and move through the veins at high speed.
- People believe that alcohol thins the blood, but this is not true. The speed of blood flow simply increases.
- At this moment, if there are blood clots in the body, they can break away from their base and death will occur instantly.
Women love to dress well and wear high heels:
- If a woman has varicose veins, then such shoes are strictly prohibited.
- The legs will be constantly under tension and this will cause stagnation of blood in the veins, which will have a detrimental effect on health.
- Also, such shoes can provoke the formation of a blood clot.
- If you already have blood clots in your legs, wearing heels is prohibited!
Sitting for long periods of time also has a negative impact on health. Therefore, for example, office workers and people who like to sit at the computer for a long time need to take breaks every hour for 10-15 minutes.
Advice: Try to move more, smoke less and do not drink alcohol, wear the right orthopedic shoes. This will help protect yourself from unwanted consequences.
Question to the doctor: how to avoid thrombosis
What can you do to reduce your risk of blood clots? What role does heredity play in the occurrence of thrombosis? What examination do you need to undergo to check the condition of your blood vessels? What research methods are used today? Does everyone at a certain age need anticoagulants? These and other questions from patients are answered by a cardiovascular surgeon at the National Medical Research Center for Surgery named after. A.V. Vishnevsky, candidate of medical sciences, associate professor Zaurbek Akhsarbekovich Adyrkhaev.
– What role does heredity play in the occurrence of thrombosis?
– From the point of view of heredity, there are several factors that may predetermine an increased risk of thrombosis. The first of them is genetic mutations, of which there are at least 12. In arterial thrombosis, this is also congenital hypercholesterolemia and hyperhomocysteinemia. These and other hereditary factors that can, at the level of blood rheology, predetermine an increased susceptibility to thrombosis - both venous and arterial - can be identified using laboratory diagnostics.
– Are arterial thrombosis and atherosclerotic plaques the same phenomenon?
– Plaques can increase the risk of arterial thrombosis - narrow the lumen of the vessel and thereby contribute to a change in the spectrum of blood flow in this area. Or they fragment - and then their pieces can come off, closing the lumen of the vessel or locally impeding the flow of blood in it, which leads to a decrease in the speed of blood flow and the formation of blood clots in this area.
– What are the differences between a blood clot and a plaque? Do they have different structures?
– A plaque is a denser formation, while a thrombus is a blood clot. A fresh blood clot is purplish-red in color, soft, and somewhat reminiscent of a slug in structure.
– Why does it form in some people and not in others? What is the mechanism of this blood thickening?
– All vascular doctors know the rules of Virchow’s triad (Rudolf Virchow is a German pathologist, a pioneer in the pathophysiology of thrombosis). In order for the process of thrombus formation to be started, three factors must occur: a slowdown in blood flow, damage to the endothelium (the internal lining of the vessel) and coagulopathy (increased blood clotting). Only in the presence of these three factors is the formation of a blood clot possible. One factor is not enough, but if it is present, as a rule, others join it and sooner or later begin to manifest themselves. Simply put, if a patient has a hereditary coagulopathy, he is already at risk. He may go on a long 8-hour flight, fall asleep on the plane and not wake up because his coagulopathy will be accompanied by a factor such as a decrease in blood flow.
– In what cases does it decrease?
– Under prolonged static loads - if a person stands for a long time, or sits, or rides in a car, flies on an airplane... In a word, being stationary contributes to the formation of venous thrombosis. At risk are also patients who have some kind of concomitant pathology - cancer, gynecological diseases that require taking hormonal medications. By the way, oral contraceptives also increase these risks.
Arterial thrombosis very rarely occurs without the presence of systemic atherosclerosis. Another risk factor for their occurrence is, of course, heart rhythm disturbances. If a patient, even with mild atherosclerosis, has atrial fibrillation, then against its background blood clots form in the heart, which can migrate and close the vessels, including the main ones - up to the aorta and iliac arteries, causing acute ischemia of the vessels of the legs.
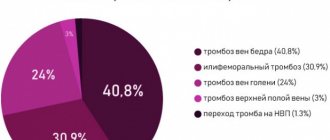
– In what parts of the body do blood clots usually form?
– With venous thrombosis, the most common location is the deep veins of the legs. The danger is that the blood clot quickly rises from the lower extremities into the femoral iliac veins. This carries enormous risks of pulmonary embolism - what is often popularly called a “blot clot.” This is the most dangerous complication of venous thrombosis, and, of course, if it is not diagnosed in time, it poses a real threat to the patient’s life.
With arterial thrombosis, the most common complication is embolism in the aortic bifurcation, when the iliac arteries close, as well as embolism in the arteries of the legs. The arteries most commonly affected are the crural arteries and the superficial femoral arteries, although others may also be affected. Here we are already talking about saving the limb, because, as a rule, such patients experience acute ischemia, which requires emergency surgical intervention to restore blood flow in the leg. And if this is not done in the coming hours, the patient may lose his leg.
– And if there is thrombosis, but it is asymptomatic, what should prompt a person to go to the doctor?
– Here we will also have to separate venous and arterial thrombosis. In the first case, this is usually a feeling of tension in the lower limb, sometimes visually assessed swelling, pain and redness along the veins that are visible on the leg. These moments should, of course, alert you, especially if this happens after those episodes that we talked about - taking hormonal drugs, pregnancy in women in the 3rd trimester, long journeys, sedentary work... If a person feels tension, swelling and pain in the limb, as well as redness and hyperemia along the vein, of course, he should consult a doctor.
If thrombosis is localized only in the veins of the leg, often the patient may even go unnoticed, and we will find out about it later - when he is examined for some other reason. By doing an ultrasound, we see that the veins are changed, and even if there are no blood clots, there are signs that the patient has suffered thrombosis.
As for arterial thrombosis, it is difficult to miss. If blood flow in any segment of a limb suddenly stops, the patient will somehow feel it. Of course, this is acute pain, coldness of the limb. The longer the ischemia lasts, the more neurological complications appear - in the form of numbness of the leg, limitation of movement in the ankle and knee joint. In later stages, of course, swelling appears.
The most difficult stage is the formation of so-called contracture in the knee and ankle joints, when the patient can no longer move the leg independently due to severe pain as a result of muscle spasms. The color of the leg changes, it first becomes pale, then a marble color appears. Severe episodes of acute ischemia are accompanied by dangerous complications such as phlegmon of the foot, etc.
If this process develops quickly, it can lead to wet gangrene, when the patient can no longer be helped. Therefore, it is so important not to miss the first symptoms - sharp pain that becomes permanent, coldness of the leg, change in skin color. And, of course, you should not try to treat yourself with home remedies; you should urgently consult a doctor.
– How does Dopplerography of leg vessels differ from ultrasound, and in what cases is this study performed?
– Doppler examination mainly shows the speed characteristics of blood flow; it is not aimed at determining the condition of the internal lining of the vessel, visualizing plaques or blood clots that nest there. Today this is no longer informative, and in our routine practice we are switching to color duplex scanning. It allows you to obtain complete data on both the speed characteristics of blood flow and the condition of the vessel as a whole: the thickness of its wall, the degree of inflammation, if any, the presence or absence of atherosclerotic plaques, how much they narrow the lumen of the vessel, whether there are blood clots in it or not, how much they spread, how many centimeters of the vessel they occupy, how tightly they are fixed to the wall (which is also very important).
– We are talking about the legs, but there are blood clots in the vessels of the head. Or is this a different story?
– Such thrombosis leads to a serious complication – stroke. Today in Moscow, and throughout Russia, a huge number of vascular centers have been opened, which are designed to combat acute coronary syndromes and acute strokes. Thrombosis results in a so-called stroke in progress, that is, the patient has the entire clinical picture of a stroke (a part of the body, an arm or a leg goes numb, speech is impaired, etc.). If an ambulance arrives on time for such a patient, it will take him to one of the vascular centers, where an attempt will be made to either systemic or local thrombolysis (dissolution of blood clots), or mechanical thromboextraction, when this thrombus is removed from the artery using special devices. Now there are all the possibilities for this, and these conditions are being dealt with quite successfully. The main thing is to do everything on time, to get into the so-called therapeutic window (from 6 to 12 hours).
– There is an opinion that after a certain age everyone needs to take blood-thinning drugs, and everything will be fine.
– Let’s start with what a person can do himself to protect himself as much as possible. The first and main thing is an active lifestyle. Aerobic exercise is needed. I tell my patients: you should walk 30-60 minutes a day, and not at a walking pace, but accelerating up to 3-4 km per hour. Do Nordic walking, swim, do whatever you like best, but be sure to move! And you should spend at least half an hour a day in the air, and spend it actively. Of course, you need to stop smoking - this is a proven fact of the risk of atherosclerosis and any complications of atherothrombosis.
The third thing is, of course, nutrition. Now the most popular diet, which is heard in all recommendations, is the Mediterranean diet. It is accessible and easy and enjoyable to stick to. The principles are very simple: limiting the consumption of animal fats and red meat (up to 1-2 times a week), the predominance of vegetable fats and fish, the basis of the diet is plant foods and plant proteins.
And another important point. In order to reduce the risk of blood clots, you need to maintain an adequate hydration regimen. A person must consume the required amount of liquid per day, and this is no less than a liter and a half (with soup, jelly, water, tea - it is not necessary to drink only clean water). By consuming liquid, you achieve blood thinning physiologically. If a person regularly does not get fluid and there is not enough fluid in his bloodstream, naturally, the blood will thicken, and the concentration of red blood cells per 1 ml of blood will increase. In this situation, he can, for example, go to the bathhouse and return from there with venous or arterial thrombosis. By sweating, a person loses up to several liters of fluid, which means that the same amount must be replenished.
Now about the drugs. I believe that no one should take anything without a doctor's recommendation. Outpatient therapists are now very educated in the field of prevention and possible complications of cardiovascular diseases, so every person should be observed in a clinic, undergo medical examination, which is being revived in our country, and if there are problems, register with a cardiologist or therapist, who, in accordance with will prescribe therapy based on indications. But you can’t take a drug that you’ve heard of or that your neighbor has been prescribed.
Previously, to reduce the risk of heart attacks and strokes, everyone was prescribed aspirin - but now studies have begun to appear that indicate the dubious benefits of uncontrolled and universal prescription of aspirin. 40 percent of people are generally tolerant to this drug, that is, when taking aspirin, they do not get the effect for which they take it. And no one who prescribes this aspirin monitors the expected effect. But everyone has a negative effect on the stomach and has long been proven.
– But new generations of antiplatelet agents have appeared.
“They are also not recommended for everyone, since they thin the blood so much that they carry the risk of bleeding. Yes, some people need them, especially after 50 years, but they should be prescribed by doctors according to indications. Everyone must do their job. The doctor is to treat, and the patient, being responsible for his health, tries to lead a healthy lifestyle as much as possible and consults doctors in a timely and periodic manner.
– You talked about a healthy lifestyle. And if, say, a blood clot already exists or is forming, can’t fitness provoke its movement?
– If at the age of 50 you decide to take up fitness for the first time in your life, of course, you should first be examined. Before starting classes, you must pass a basic fitness test. This is not at all the same as when they tell you how and what kind of exercise machine works; you should be consulted by a doctor who will determine your tolerance to physical activity and do tests under the control of an ECG and other devices.
– Let’s simulate such a situation. The person knows that there have been strokes and cases of blood clots in his family. And he wants to protect himself as much as possible. What examinations should he do to check the condition of the blood vessels?
– Firstly, a general and biochemical blood test, for a lipid profile - to find out the atherogenic index (the ratio of high and low density lipoproteins).
You need to take a coagulogram - look at blood clotting indicators, do an ECG, measure the ankle-brachial index, which reflects the state of blood circulation in the lower extremities. If this index is reduced, we can talk about systemic atherosclerosis. It is necessary to determine the level of homocysteine in the blood (an elevated level can also indicate atherosclerotic complications), and also perform an ultrasound of the carotid arteries.
I would also not overlook an abdominal ultrasound, which can look for an aortic aneurysm, which is often the first disease to manifest in a patient with atherosclerosis. And, of course, if a more in-depth examination is carried out, an echocardiogram will be required to see whether the heart muscle is functioning normally.
The brain, heart and lower extremities are the risk points for atherosclerosis and blood clots for a person who knows his hereditary predisposition to these diseases. And the listed studies are the minimum that will allow him to draw up a primary picture.
– And after this live in peace?
- Not certainly in that way. The person who has done all these studies should then go to the doctor. Even if the indicators are within the normal range, this may be the upper limit of the norm, which already indicates some changes. Only a doctor can determine the risks. And if changes in the vessels are detected, the examination must be repeated once a year.
Moreover, I recommend everyone to monitor their blood sugar, because diabetes is also one of the risk factors and worsens the prognosis in patients with atherosclerosis. As for venous thrombosis, you should pay attention to whether your legs swell at the end of the working day, whether you feel discomfort after long journeys and flights, whether it is difficult to put on boots or shoes. In this case, you need to do an ultrasound of the veins and again consult a doctor.
The main thing is not to self-medicate, it will never be effective. Take care of your blood vessels and overall health!
The full version of the interview was published in No. 5/20 of the Be Healthy magazine.
Could there be a blood clot in the arm?
Blood clot in the arm
According to research and the experience of doctors, blood clots can form in various organs and in any part of the human body, including in the arm. When this happens, a person experiences the following symptoms:
- The affected hand is colder than the other. Due to impaired blood formation, the affected hand becomes colder than the other. But such a symptom is difficult to notice on your own.
- Decreased sensitivity. First, bodily sensations become weak, and then pain sensitivity decreases. A person may not even notice when he is burned by hot objects.
- Swelling of the hand. When there is a blood clot in a vein in the arm, it causes swelling. This symptom is almost impossible to ignore, as it brings severe discomfort.
- Increased body temperature. This happens if a blood clot appears in a vein. Body temperature rises slightly. Usually it is kept at 37.5 - 38.0 degrees.
The first signs of a blood clot:
- The person feels quickly exhausted and tired
- Breathing is difficult
- Dizziness and fainting may occur
- Palpitations, headache
The main danger of thrombosis is that often this disease is not traced and is not felt in any way by the human body. Only some external changes may appear in the affected area, but people often do not attach any importance to this. Therefore, it is important to prevent thrombosis: daily physical activity, do not sit in one place for a long time, monitor your weight and nutrition, drink plenty of water. Good luck!