Pericarditis is inflammation of the outer lining of the heart. Most often it is infectious, rheumatic or post-infarction. Pericarditis has the following symptoms:
- Weakness;
- Constant pain behind the sternum, which intensifies when inhaling;
- Cough;
- Severe shortness of breath.
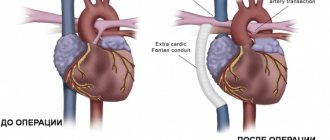
Pericarditis occurs with fluid leaking between the pericardial layers (observed with exudative pericarditis). This pathology is dangerous due to the development of suppuration and cardiac tamponade (when accumulated fluid compresses the heart and blood vessels) and may require immediate surgical intervention.
Pericarditis can be a symptom of a systemic, infectious, cardiac disease, as well as a complication of various pathologies of internal organs or injuries. Often it is pericarditis that becomes of paramount importance in the clinical picture of the disease, and other manifestations of pathology fade into the background. Diagnosis of pericarditis is not always made while the patient is alive; in approximately 4–7% of cases, signs of past pathology are determined only at autopsy. Pericarditis can occur at any age, but, as a rule, occurs among the adult and elderly population, and the incidence of pericarditis in females is higher than in males.
With serous pericarditis, the inflammatory process spreads to the serous tissue membrane of the heart (parietal, visceral plate and pericardial cavity). Permeability increases and blood vessels dilate, leukocytes infiltrate, fibrin is deposited, adhesions are added and scars are formed, pericardial layers become calcified and the heart is compressed.
Pericarditis has the following causes:
- Rheumatism (endocarditis and myocarditis are also affected);
- Tuberculosis (when infection spreads from foci in the lungs through the lymphatic ducts to the lymph nodes.)
Both diseases are manifestations of an infectious-allergic process.
Certain conditions increase the risk of developing pericarditis, including:
- Infectious and viral diseases - influenza, measles;
- Bacterial processes - tuberculosis, tonsillitis, scarlet fever;
- Sepsis;
- Fungal and parasitic infection;
- Pneumonia;
- Pleurisy;
- Endocarditis (lymphogenous or hematogenous route);
- Allergic damage (serum sickness, drug allergy);
- Systemic connective tissue diseases (lupus erythematosus, rheumatoid arthritis, rheumatism and others);
- Heart pathologies (myocardial infarction, endocarditis or myocarditis);
- Surgical interventions;
- Malignant processes;
- Metabolic disorders (toxic effects due to uremia and gout);
- Radiation damage;
- Heart malformations (pericardial cysts and diverticula);
- Edema;
- Hemodynamic disturbances (as a result, fluid accumulates in the pericardial space).
At the Yusupov Hospital, patients with pericarditis are provided with all types of treatment by highly qualified doctors. Specialists collect all anamnestic data in detail and conduct diagnostic studies using the latest equipment. The staff of the Yusupov Hospital takes care of their clients not only in a hospital setting, so patients with pericarditis are given precise clinical recommendations after discharge.
Classification of pericarditis
There are primary and secondary pericarditis. The disease can be limited, occupying the base of the heart, partial, or general diffuse (the entire serous membrane is involved).
Considering clinical data, pericarditis can be acute or chronic.
Acute pericarditis develops quickly, lasting no more than six months, among them there are:
- Fibrinous pericarditis (dry);
- Exudative;
- Serous-fibrinous pericarditis;
- Hemorrhagic;
- Purulent;
- With and without cardiac tamponade.
Chronic pericarditis develops slowly, lasts more than six months and is divided into:
- Effusion pericarditis;
- Adhesive;
- Exudative-adhesive;
- Asymptomatic;
- Pericarditis with functional disorders of cardiac activity;
- Pericarditis with extracardial adhesions;
- Constrictive;
- Pericarditis with dissemination of inflammatory granulomas.
Non-inflammatory pericarditis includes:
- Hydropericardium;
- Hemopericardium;
- Chylopericardium;
- Pneumopericardium;
- Effusion due to myxedema, uremia, gout.
Pericardial neoplasms include:
- Primary tumors (benign and malignant);
- Secondary;
- Paraneoplastic syndrome.
Among the rare diseases of the pericardium, pericardial and coelomic cysts are distinguished separately. Such cysts can be congenital or acquired.
Symptoms and possible complications
The volume of transudate in uncomplicated hydropericardium usually does not exceed 100-200 ml. An increase in this indicator should always raise suspicion that an inflammatory process is involved.
When the effusion volume is less than 100 ml, no subjective manifestations are observed. An increase in the amount of transudate is manifested by the following symptoms:
- Chest pain that gets worse when bending forward.
- General weakness, pale skin.
- Increased sweating.
- Tachycardia, which is not always fully felt by the patient due to weak heart contractions.
- Rapid shallow breathing.
- Edema of the lower extremities.
With a further increase in fluid volume (adaptive capabilities allow the pericardium to accommodate up to 1000-1500 ml), the intensity of symptoms increases and blood pressure decreases. In rare cases, it is possible to develop a life-threatening complication - cardiac tamponade, in which the accumulated transudate compresses the organ so much that adequate contractions become impossible. This condition is accompanied by severe weakness, increasing shortness of breath, fear of death and requires immediate medical intervention.
Pericarditis and myocarditis: what is the difference?
The main distinguishing feature is that myocarditis is an inflammatory lesion of the heart muscle, and pericarditis is an inflammation of the lining of the heart. Myocardial symptoms may include fever, rapid heart rate, fatigue, difficulty breathing, and chest pain. Patients with pericarditis often complain of sharp chest pain, difficulty breathing, and pain when taking a deep breath. For diagnostics use:
- Chest X-ray;
- Electrocardiogram;
- Echocardiogram;
- UAC;
- Biopsy of areas of the heart muscle.
Causes
Hydropericardium is not considered as an independent disease; it is a complication of other pathological processes in the body. Therefore, there are quite a few possible reasons for the development of this condition. These include:
- Heart failure - effusion is formed due to congestion.
- Intoxication with chemical reagents (mercury, heavy metal salts), tumor decay products.
- Cachexia. In malnourished patients, hydropericardium may develop due to a decrease in the size of the heart, which ceases to sufficiently fill the pericardial cavity.
- Inflammatory diseases of the urinary system and renal failure. The volume of fluid in the pericardial sac increases due to disturbances in acid-base and water-salt metabolism, and may also be a manifestation of swelling of the internal organs at the last stage of kidney dysfunction.
- Severe anemia - disruption of cellular respiration processes leads to the formation of transudate.
Hydropericardium is also one of the symptoms of such congenital heart disease as left ventricular hypoplasia. In addition, this pathology can accompany chest injuries.
Publications in the media
Exudative pericarditis is an advanced form of inflammation of the pericardium with accumulation of effusion in the cavity of the pericardial sac. If fluid accumulates rapidly, then even with 200 ml of effusion, symptoms of cardiac tamponade may occur. With the slow accumulation of exudate, even a significantly larger volume does not cause clinical symptoms. Exudative pericarditis with cardiac tamponade can be acute and subacute. Etiology. The most common causes of exudative pericarditis: • Acute pericarditis - viral (including as a probable cause in idiopathic pericarditis) or idiopathic • Malignant tumors • Exposure to radiation • Trauma • Diffuse connective tissue diseases (SLE, rheumatoid arthritis) • Postpericardotomy syndrome • Dressler's syndrome • The accumulation of fluid in the pericardial cavity can cause any disease that affects the pericardium • In most patients, the etiology of pericardial effusion cannot be determined even during surgery.
Pathogenesis. The effect of pericardial effusion on hemodynamics largely depends on the rate of its accumulation and the distensibility of the outer layer of the pericardium. Rapid accumulation of fluid in the pericardial sac can lead to severe hemodynamic disturbances, while a gradual increase in its amount can remain virtually asymptomatic for a long time. Pericardial effusion makes it difficult for the heart to fill with blood, with a decrease in its inflow and stagnation, primarily in the systemic circulation. Clinical manifestations • Pericardial effusion is often detected during an x-ray (fluorographic) examination or during echocardiography. Its presence should be assumed in patients with tumors of the lungs or chest, in patients with uremia, with unexplained cardiomegaly, or an unexplained increase in central venous pressure. • Pericardial friction rub is not typical. • The gradual accumulation of fluid in the pericardial cavity is not accompanied by any complaints. An objective examination is usually uninformative. • With the accumulation of a significant amount of fluid •• Pain in the chest, worsens with breathing, coughing, sometimes radiating to the left shoulder, neck, less often to the epigastric region; often begins suddenly; decreases with changes in body position - bending forward and squatting •• Swelling of the face and neck during examination •• Symptoms associated with compression of the heart •• Expansion of the boundaries of relative cardiac dullness in all directions, reduction and disappearance of the apical impulse •• Kussmaul's symptom - increased swelling of the cervical veins during inspiration •• Increased central venous pressure, arterial hypotension, tachycardia (sometimes cardiac arrhythmias, often transient); Paradoxical pulse is characteristic. Additional studies • ECG - decreased voltage of QRS complexes with significant accumulation of fluid in the pericardial cavity. ST segment elevation and signs of complete electrical alternans are also possible: fluctuations in the amplitude of the QRS complex, P waves and T waves (the result of a change in the position of the heart in the chest with a large amount of fluid). • EchoCG is the most specific and sensitive method for diagnosing pericardial effusion: in two-dimensional mode, fluid is detected in the pericardial cavity •• With a small accumulation of fluid, a “free” space appears behind the posterior wall of the left ventricle •• With a moderate accumulation of fluid in the pericardial cavity, a “free” space is determined behind the posterior wall of the left ventricle with a thickness of more than 1 cm and its appearance in the area of the anterior wall, especially during systole •• A significant amount of fluid in the pericardial cavity is characterized by the detection of “free” spaces around the heart in all projections in both phases of the cardiac cycle. • X-ray examination : with a small and moderate accumulation of fluid in the pericardial cavity, the contours of the heart do not change. Cardiomegaly occurs when there is a significant accumulation of fluid in the pericardial cavity. The left circuit of the heart may straighten. Sometimes the heart takes on a triangular shape and its pulsation decreases. • Study of pericardial fluid. To clarify the cause of the hydropericardium, a puncture of its cavity is carried out and the resulting fluid is analyzed (tumor nature of the disease, bacteria, fungi) •• The cytological composition of the fluid is studied •• Bacteriological studies are carried out •• The protein content and activity of LDH are determined •• After centrifugation, an analysis is carried out for atypical cells • • For differential diagnosis with rheumatic diseases, the resulting fluid is examined for ANAT and LE cells •• The presence of hemorrhagic exudate (characteristic of tumors and tuberculosis) may be the result of an accidental puncture of the ventricular wall with a needle (blood from the ventricle coagulates, but not from the exudate). • A biopsy with morphological examination of pericardial tissue is possible.
TREATMENT is carried out in a hospital, if possible, taking into account its etiology. Management tactics depend on the volume of fluid in the pericardial cavity. If the amount of fluid is small, no therapy is required. Drug therapy • NSAIDs are used in average therapeutic doses • It is possible to prescribe GCs, for example, prednisolone at a dose of up to 60 mg/day for 5-7 days, followed by a gradual decrease. The use of prednisolone ensures fairly rapid resorption of effusion. Pericardiocentesis with the introduction of GC into the cavity of the heart sac is indicated if GCs do not have an effect within 2 weeks and a large effusion persists. Complications and prognosis depend on the etiology of the disease. Viral and tuberculous pericarditis are often complicated by cardiac tamponade or result in the development of constrictive pericarditis. Effusion associated with uremia, tumor, myxedema, diffuse connective tissue diseases usually requires specific treatment, much less often - pericardiectomy. Synonym. Pericarditis is effusion. See also Pericarditis, Cardiac tamponade, Constrictive pericarditis.
ICD-10. I30 Acute pericarditis
Diagnostics
The examination of the patient begins with a history and examination. During percussion, an increase in the size of the heart is determined.
As part of instrumental research, the following is used:
- Chest X-ray - reveals only a significant increase in fluid volume.
- X-ray kymography is a method of recording the pulsation of parts of the heart, as well as the great vessels. With hydropericardium, X-ray film reveals a uniform decrease in ventricular and atrial waves, and with large effusions, their complete disappearance.
- Echocardiography, which is the main method for identifying this pathology. Normally, the distance between the heart wall and the inner surface of the pericardium is 3-5 mm. An increase in the lumen according to ultrasound results to 10 mm or more proves the presence of significant effusion in the cavity.
- Diagnostic puncture of the pericardium is the only method that allows one to establish the exact nature of the pathological contents of the cavity of the heart sac. With hydropericardium, the fluid is transparent, yellowish, poor in protein, and may contain traces of fibrin, a small number of lymphocytes, and sometimes single erythrocytes.
As part of an extended diagnosis aimed at determining the underlying disease that led to the occurrence of hydropericardium, a general and biochemical blood test and a general urinalysis are prescribed. Ultrasound of the abdominal cavity and pelvis, CT scan of the chest and other studies may also be prescribed.