5.2. Pharmacological drugs used in the treatment of chronic venous disease
The means of basic pharmacotherapy for chronic venous disease are phlebotropic drugs (synonyms: FLP, venoactive drugs, phleboprotectors, venotonics), which represent a heterogeneous group of biologically active substances obtained by processing plant raw materials or chemical synthesis, united by the ability to increase venous tone, as well as reduce the severity of venous -specific symptoms and syndromes.
The classification of the main phlebotropic drugs is presented in Table 5.
Table 5. Classification of main phlebotropic drugs
| Group | Substance | Sources of raw materials |
| γ-benzopyrones (flavonoids) | Diosmin | Japanese Sophora (Saphora japonica) |
| Micronized purified flavonoid fraction (MPFF) | Rutaceae (Rutaceae aurantiae) | |
| Rutin and hydroxyethylrutosides (HER) | Eucalyptus (Eucalyptus spp.), Buckwheat (Fagopyrum esculentum) | |
| Saponins | Horse chestnut seed extract, escin | Horse chestnut (Aesculus hippocastanum L) |
| Ruscus extract | Butcher's broom (Ruscus aculeatus) | |
| Other plant extracts | Proanthocyanidins (oligomers) | Grape seeds and red grape leaves |
| Ginkgo dicotyledonous extract + heptaminol + GER | Ginkgo dicotyledonous | |
| Synthetic drugs | Calcium dobesilate | Synthetic |
| Diosmin | Semi-synthetic |
5.3. Mechanism of action of phlebotropic drugs
Phlebotropic drugs increase the tone of peripheral veins and lymphatic vessels due to their effect on the norepinephrine-dependent mechanism, as well as due to some drug-specific effects (Table 6).
Table 6. Therapeutic effects and mechanisms of action of phlebotropic drugs
| Effect | Phlebotropic drug |
| Anti-edematous and capillary-protective | All phleboprotectors |
| Analgesic (venous pain) | MOFF, red grape leaf extract |
| Venotonic | All phleboprotectors Note: butcher's broom extract is a partial agonist of venous ɑ1-adrenergic receptors (neutralizes nitric oxide in the arterial section of the capillary bed) |
| Lymphotropic | MOFF, butcher's broom extract |
| Rheological | MOFF, troxerutin, rutin |
| Profibrinolytic | MOFF, troxerutin, diosmins |
| Anti-inflammatory | MOFF, Gingko dicotyledonous extract, diosmin |
| Inhibition of leukocyte-endothelial adhesion | MOFF |
| Venous valve protection | MOFF |
| Venous wall protection: | |
|
|
What are venotonics?
Venotonics (phlebotonics) are drugs that improve the condition of the vascular wall.
They have two main effects:
Venotonic – increase tone, i.e. tension of the venous wall, and due to this they reduce the distensibility of the veins and prevent stagnation of blood in the veins.
Angioprotective - increase the resistance of capillaries to damage, improve microcirculation, and therefore nutrition of the vascular wall.
Venotonic drugs are used mainly for venous diseases and for the treatment of acute hemorrhoids, because in this case, the venous outflow is also impaired, but only through the veins of the rectum.
5.4. Clinical effectiveness of phlebotropic drugs
The main indication for the use of phlebotropic drugs are symptoms associated with CVD: heaviness in the legs, discomfort, itching, pain along the varicose veins, paresthesia, night cramps and other vein-specific complaints; chronic venous edema, as well as trophic skin disorders, including venous ulcers. Numerous clinical trials indicate that in the early stages of the disease (C0S-C2S) all phlebotropic drugs have a good therapeutic effect on subjective symptoms, but not external manifestations (telangiectasia, varicose reticular and saphenous veins) of CVD.
However, when conducting pharmacotherapy of early stages of chronic venous disease, preference should be given to phlebotropic drugs, whose effectiveness and safety have been proven in randomized controlled clinical trials.
Chronic venous edema (C3) is an absolute indication for the prescription of phlebotropic drugs.
According to the meta-analysis, the most pronounced anti-edematous effect is demonstrated by MOFF (Detralex), which is the first choice drug for chronic venous edema. Hydroxyethylrutosides (Venoruton) and butcher's broom extract (Cyclo 3 fort) also reduce chronic venous edema and can serve as second-line drugs. The effectiveness of non-micronized (native) diosmin against chronic venous edema is not significantly different from placebo. To evaluate the effectiveness of other phlebotropic drugs for chronic venous edema, it is necessary to conduct randomized clinical trials using standardized protocols. Venous trophic ulcers. Currently, the results of only one meta-analysis are known, including 5 randomized controlled trials, according to which MOFF in combination with standard compression therapy accelerates the healing of trophic ulcers with an area of up to 10 cm2 by an average of 5 weeks.
Perioperative period. It is advisable to use phlebotropic drugs to accelerate medical and social rehabilitation and prevent unwanted side effects during phlebosclerosing and surgical treatment of chronic venous disease. Currently, the positive effect of MOFF has been confirmed, significantly reducing the intensity of postoperative pain, swelling and severity of hemorrhages after endovascular and surgical treatment of CVD.
Summary data on the effectiveness of phlebotropic drugs in the treatment of different stages of CVD are presented in Table 7.
Table 7. Efficacy of phlebotropic drugs against various symptoms and syndromes associated with CVD
| Disease class | Individual entrepreneur | Duration of treatment | Level of evidence of effectiveness |
| C0,1,2 + vein-specific symptoms | All individual entrepreneurs | 2-3 months | A-C |
| C0-2 + venous pain |
| At least 3 months | A-B |
| C3 (chronic venous edema) |
| At least 3 months | A, B |
| S4-6 | MOFF | At least 6 months | A-C |
*currently available evidence base is insufficient
Properties of drugs
Venotonics are divided depending on their composition into herbal, synthetic and semi-synthetic. The composition of herbal phlebotropic preparations includes biological additives and active compounds (saponins, flavonoids). Almost all phlebotropic medications have shown high effectiveness in treating subjective symptoms at the earliest stages of their course. Detralex has pronounced anti-edematous properties and best fights chronic venous edema. Drugs such as Cyclo 3 Fort and Venoruton also work well as a treatment for such a disease; they can be used as second-line drugs.
According to multiple clinical studies, Detralex in combination with compression therapy significantly increases the healing rate of small venous ulcers. In addition to all of the above, phlebotropic drugs increase the level of rehabilitation after treatment of venous disease through surgery and reduce the likelihood of side effects after surgery.
5.5. Safety of oral phlebotropic drugs
Phlebotropic drugs are well tolerated by the vast majority of patients. Undesirable dyspeptic (abdominal pain, diarrhea, vomiting, etc.) and autonomic (insomnia, dizziness, etc.) are noted by no more than 5% of patients. Undesirable side reactions typical for various phlebotropic drugs are presented in Table 8.
Table 8. Possible undesirable side reactions when using various phlebotropic drugs
| A drug | Skin reactions | Dyspeptic reactions | Other unwanted side effects |
| Oxerutin and rutosides | Frequent, especially in combination with topical forms | Frequent | |
| Escin (horse chestnut extract) | + | Dizziness, headache, urticaria | |
| Ruscus extract | + | ||
| Grape seed and red leaf extract | + | Frequent | Dizziness, headache, urticaria, tachycardia |
| Ginkgo dicotyledonous extract + troxerutin + heptaminol | + | + | |
| Diosmin** | + | + | Dizziness, weakness, tachycardia, etc. |
| MOFF* | + | Rare autonomic reactions such as weakness and dizziness | |
| Calcium dobesilate** | + | + | Agranulocytosis |
* MOFF is safe for long-term (6 months or more) use, and the frequency of unwanted side reactions does not increase
** Synthetic drugs are more likely to cause dyspeptic reactions.
5.6. The use of phlebotropic drugs in pregnant women
In the second and third trimesters of pregnancy, MOFF, diosmin, hydroxyethylrutosides and a combination of Ginkgo dicotyledonous extract with heptaminol and troxerutin are allowed. At the same time, the lack of serious clinical studies on the use of phlebotropic drugs in pregnant women makes their use justified only in cases where the benefits of using phleboprotectors outweigh the potential negative reactions. It is not recommended to prescribe phlebotropic drugs during breastfeeding.
Contraindications
Most of these drugs are highly tolerable. Minor side effects (vegetative or dyspeptic) are rare, occurring only in five percent of cases. The main contraindication for the use of a group of drugs is intolerance, allergy to the composition of the drug or a high risk of side effects. Among others, we can highlight:
- Pregnancy period. Venoruton, DoxyChem and Flebodia are approved for use only in the second and third trimester of pregnancy. Pregnancy is not a contraindication for Venolife. According to the instructions, the use of the drugs Aescusan and Detralex is not prohibited, but the use of the drug is not permitted either. The last word goes to the attending physician. And the drug Ginko Forte, according to the instructions for use, is strictly prohibited for pregnant women.
- Breast-feeding. While there is no reliable data on the effect of active substances on mother's breast milk, the use of phlebotropic drugs in nursing mothers is prohibited.
- Age. Venotonics Ginko Forte, Cyclo 3Forte (18), Phlebodia, Doxichem contain age restrictions in their instructions. Troxevasin and troxerutin have different age restrictions. For example, the instructions for using troxevasin are silent about such restrictions. And the instructions for troxerutin say that there are not enough experimental clinical trials for use under 18 years of age. Other phlebotropic medications do not contain age restrictions on the use of the drug.
5.8. Regimen for taking and dosing phlebotropic drugs
Adequate doses of phlebotropic drugs recommended by manufacturers should be prescribed, and standard treatment regimens and durations should be followed. Exceeding standard daily doses does not always increase the clinical effect, but increases the frequency of unwanted side reactions that disrupt the initiated course of pharmacotherapy. However, a number of studies indicate that in certain clinical situations, increasing the dose of a phlebotropic drug can increase its therapeutic effectiveness. In this regard, in situations where the benefit outweighs the potential risk, the dose of the phlebotropic drug may be increased after documented justification and obtaining informed consent from the patient.
It is advisable to prescribe phlebotropic drugs in the form of monotherapy or fixed combinations*, since the simultaneous use of two or more drugs belonging to related chemical classes does not enhance the therapeutic effect, but increases the likelihood of developing undesirable side reactions.
* fixed combination is a multicomponent drug
Phlebotropic drugs are prescribed in courses, the duration of which is selected empirically, based on the dynamics of symptoms and syndromes, the duration of remission, and the occurrence of undesirable side reactions. For patients with the initial stages of chronic venous disease (C0S-C2S), the duration of the standard course ranges from 1.5 to 3 months (2.5-3 months on average). For chronic venous edema (C3), trophic skin disorders, and especially open ulcers (C4-6), phlebotropic drugs can be prescribed for 6 months or more.
It is advisable to start a course of phlebotropic drugs with the period of expected exacerbation of the disease or a possible violation of the compression regime. Thus, the use of compression therapy is difficult in the hot season, when working in conditions of high temperature and humidity, as well as when it is necessary to comply with a dress code. A negative background, often leading to an exacerbation of the course of chronic venous disease, is created by a long forced stay in a sitting or standing position (many hours of air flights, travel by bus or car, etc.), an increase in work (heavy lifting, etc.) or household (housework or on a personal plot, caring for bedridden patients, etc.) physical activity.
In severe forms of CVI, especially in obese patients who experience insurmountable difficulties wearing compression bandages or medical hosiery, as well as when compression therapy is not possible, phlebotropic drugs are prescribed for continuous use. MOFF has the highest safety profile for long-term (6-12 months) use.
Drugs for the treatment of vein diseases
What does the whole world choose?
Treatment of varicose veins requires an integrated approach and should primarily be aimed at preventing complications of the disease. It is important to understand that it is necessary not only to combine various methods of therapy, but also to strictly follow the doctor’s prescription - this applies to both non-pharmacological treatment (wearing compression stockings, lifestyle changes, gymnastics, etc.) and to taking medications (venotonics ).
An integral part of the fight against varicose veins
- the use of phlebotropic drugs,
venotonics
, which can increase vascular tone and reduce the symptoms of the disease.
Types of venotonics
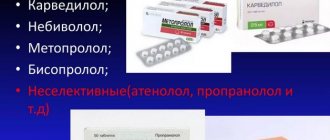
All drugs used in modern medicine for the treatment of varicose veins are divided into the following categories:
:
· external agents, which are mainly used to relieve symptoms in combination with drugs for oral administration;
· systemic drugs in the form of tablets or suspensions, their action is aimed not only at relieving symptoms, but also at treating the disease.
Drug therapy is considered an integral part of the treatment of varicose veins of the legs.
. With the help of medications, you can increase the tone of the veins, improve microcirculation and lymph flow, and prevent inflammatory complications. They are primarily aimed at the cause of the disease, their target is inflamed vein walls that have lost their tone. Therefore, such drugs form the basis of therapy [1].
Of the wide variety of venoactive drugs, Detralex
[2]. And it is not surprising: the drug has held a strong position in both domestic and international recommendations for many years [1, 3].
Detralex
works comprehensively: increases the tone of the veins, reduces capillary permeability, thereby helping to reduce symptoms such as pain, heaviness, fatigue in the legs, swelling [4].
Thanks to this, Detralex
helps prevent the occurrence of unpleasant complications and the further development of venous diseases [5, 6].
Therefore Detralex
has earned the trust of consumers: it is chosen by millions around the world.[9]
External agents are a variety of gels and ointments
.
Among these drugs is Detragel
, which has a unique composition [7].
It includes heparin, escin and essential phospholipids [8]. The product is quickly absorbed, does not stick and does not stain clothes. Thanks to its composition, Detragel
helps to cope with the symptoms of varicose veins: pain, leg fatigue and a feeling of heaviness [8].
Also, to treat varicose veins, you can apply externally tinctures, lotions and decoctions prepared according to folk recipes. However, such methods do not provide the necessary integrated approach, and their effectiveness has not been proven. In addition, they may not be as safe as they seem at first glance. For example, homemade herbal alcohol tinctures can be irritating to the skin. It is not even the use of folk remedies itself that can pose a serious danger, but rather the refusal to consult a doctor in favor of self-medication. After all, varicose veins do not go away on their own. Its progression can have much more serious consequences. In advanced cases, we are no longer talking about “nets” and “nodules” on the legs, but about thrombosis or trophic ulcers. That is why it is necessary to consult a doctor in a timely manner to prevent such developments.
THERE ARE CONTRAINDICATIONS. YOU MUST CONSULT A SPECIALIST
1. Russian clinical guidelines for the diagnosis and treatment of chronic venous disease. Phlebology, 2021, No. 3, volume 12
2. Surgical monitor: among venoactive (phlebotropic) agents. Spring, 2021.
3. Management of chronic venous disorders of the lower limbs. Guidelines according to scientific evidence. International Angiology 2021. 37(3):181-254. (International guidelines for the treatment of chronic diseases of the lower extremities)
4. Instructions for medical use of the drug Detralex®. RU No. LP-003635.
5. Pascarella L. Essentials of Daflon 500 mg: from early valve protection to long-term benefits in the management of chronic venous disease./Current Pharmaceutical Design. 2007; 13(4):p.431–444 (Pascarella L. Modern Pharmacy 2007; 13(4):pp. 431-444)
6. Sapelkin S.V. et al. Chronic venous diseases: valve function and leukocyte-endothelial interaction, possibilities of pharmacotherapy. Angiology and vascular surgery. Volume 23 No. 3/2017, 89.
7. According to GRLS data among drugs registered in Russia as of March 15, 2018.
8. Instructions for medical use of the drug Detragel®. RU No. LP-001044
9. “Data from the GFK-Rus study on household purchases in the Russian Federation for the period from 07/01/2018 to 06/30/2019.”
As an advertisement.
5.9. Local dosage forms for the treatment of chronic venous disease
The therapeutic effect of local medications is largely due to the distracting effect due to the evaporation of volatile components (local hypothermia) and massage during application and rubbing of the drug. The seemingly rapid therapeutic effect of local drugs quickly wears off and requires their repeated use. It must be clearly understood that local dosage forms should be used in combination with compression therapy and systemic drugs.
Local dosage forms in the form of gels and sprays, including heparin, NSAIDs and phleboprotectors, are advisable to use for rapid relief of vein-specific symptoms (pain, feeling of heaviness and heat, local swelling, etc.). Their use is not recommended for asymptomatic forms of CVD.
The effectiveness of various ointments and gels is directly dependent on the concentration of the active substance. In this regard, when prescribing heparin-containing gels, preference should be given to drugs with a high concentration of the active substance of 500-1000 IU/gram.
Contraindications to the use of local dosage forms (with the exception of corticosteroids and dermatoprotectors) are damage to the skin (erosion, excoriation), dermatitis and eczema, as well as open trophic ulcers.
Methods of application
Symptoms are divided into objective and subjective. Subjective is expressed by pain, tingling, burning, a feeling of heaviness and itching. Patients often complain of pain in the legs, muscle cramps (mainly the calf muscles) and constant fatigue. Objective symptoms are expressed by changes in the skin, the appearance of trophic ulcers, edema, and dilation of the saphenous veins. To eliminate all types of symptoms listed above, phlebotropic drugs are used
Such venotonics are used in the treatment of pelvic congestion disease, as a prophylactic against edema during the menstrual cycle. To reduce pain. It is used in the postoperative period, after operations on the veins, as a prophylaxis. Do not use alone during the treatment of acute venous thrombosis and vascular blockage. For the treatment of such diseases, use strictly in combination with anticoagulants.
5.10. Antiplatelet and other drugs used in the treatment of CVD
Antiplatelet and hemorheologically active drugs (acetylsalicylic acid drugs 50-150 mg/day, pentoxifylline 1200-2400 mg/day) are advisable to prescribe in the presence of appropriate concomitant pathology (diabetes mellitus, obliterating atherosclerosis, etc.).
For chronic venous edema and trophic skin disorders (C3,4,5 according to CEAP), the use of polyenzyme drugs (wobenzym, phlogenzyme) in standard therapeutic dosages may be useful. Due to the fact that polyenzyme drugs in some cases can contribute to the destruction of biological membranes and exacerbation of the local infectious process, it is advisable to combine them with rational antibacterial therapy.
A comment
. For venous trophic ulcers, sulodexide can be used as an additional therapy. The role of multienzyme drugs in the treatment of chronic venous disease requires further study. The use of prostaglandins for the treatment of chronic venous disease is possible in the presence of trophic skin disorders and ulcers of mixed arteriovenous origin.
5.11. Monitoring the effectiveness of treatment
One should strive to objectify the assessment of the effectiveness of the treatment. For complaints and subjective symptoms, it is useful to use visual analogue scales and disease-specific questionnaires (CIVIQ, etc.). When monitoring the dynamics of chronic venous edema, it is advisable to use a measuring tape or more precise instruments (leg-O-meter, volumetric meter, etc.).
In case of trophic skin disorders, the effectiveness of the treatment is indicated by a decrease in inflammatory phenomena and the area of indurative cellulite, as well as signs of epithelization of a venous ulcer.
If there is no effect from the therapy, it is necessary to carry out additional differential diagnostics.