Errors in blood pressure measurements interfere with correct diagnosis
March 14, 2021 marks the 100th anniversary of the death of the Russian surgeon Nikolai Sergeevich Korotkov, who proposed a non-invasive method of auscultal (sound) measurement of blood pressure (BP) back in 1905. And although the Korotkoff method has been used for a long time, errors are still made in measuring blood pressure. On March 3, 2020, the traditional “Scientific Tuesday” of the Federal State Budgetary Institution “NMITs TPM” of the Ministry of Health of Russia was devoted to the issues of measuring blood pressure. , Doctor of Medical Sciences, Professor V.M., reviewed the current international recommendations for measuring blood pressure. Gorbunov.
He gave examples of specific recommendations for blood pressure measurement developed by the American Heart Association (AHA) and the Lancet Commission on Hypertension Group and discussed in detail various aspects of this procedure.
Talking about office blood pressure measurement (measurement within the walls of a medical institution), Vladimir Mikhailovich presented interesting data on mathematical modeling of the prevalence of arterial hypertension (AH) with a normal diet and with a reduction in daily salt intake using the example of Canada. The expected effect of the intervention is only 5 mm Hg. However, even such a seemingly insignificant reduction in blood pressure in the population would have a huge effect: the prevalence of hypertension would decrease from 3.5 to 2.5 million patients, or by 30.3%. This implies the need for extremely careful and accurate blood pressure measurements.
The speaker noted some important elements of standard blood pressure measurement that need to be addressed. Outside of measurement, the mercury column of the tonometer must be at zero, the tonometer must not be damaged, and the numbers must be clearly visible. Aneroid (mechanical) tonometers require regular calibration.
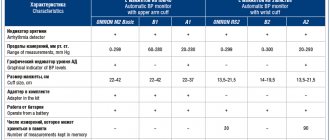
As for electronic tonometers, according to Professor V.M. Gorbunov, the oscillometric algorithms used in them are different and are not disclosed by the manufacturers. Therefore, these devices must be validated according to an international protocol in an independent clinical study. However, in some patients, measurements may be inaccurate due to the limitations of the oscillometric method, which most accurately estimates mean, but not systolic or diastolic blood pressure. As the specialist noted, the validation of electronic blood pressure measurement devices is a critically important point when choosing them for clinical purposes.
To avoid errors when measuring blood pressure in a health care setting, it is important to record readings to the nearest 2 mmHg. avoid arbitrary rounding to 5 or 10 mmHg. Art. At the patient’s first visit to the doctor, blood pressure measurements should be taken on both arms, and subsequently measurements should be taken on the arm on which higher pressure is recorded. At each visit, the patient must take at least two measurements. The Expert Committee recommends the use of arithmetic averages for clinical decisions.
As Vladimir Mikhailovich said, when measuring blood pressure, four types of errors can occur: those associated with the patient, with the procedure itself, with the device and with the observer. Thus, the patient’s intake of food and caffeinated drinks, smoking before the procedure, a full bladder and the well-known so-called “white coat effect” can lead to errors in measurements.
Procedural errors include measuring blood pressure after insufficient rest, incorrect patient positioning (crossed legs), low cuff placement (below heart level), talking during the procedure, and deflating air too quickly. Erroneous data can also be obtained with an inappropriate cuff size. However, the speaker noted, the error arising due to the last two reasons, well known to doctors, is significantly lower than when the basic conditions for preparing the patient and performing the procedure are not observed (insufficient rest, smoking, talking).
Observer errors include arbitrary rounding of the obtained figures, which in 80% of cases gives inaccurate results of systolic and diastolic blood pressure, a single measurement (according to the 2019 AHA recommendations, blood pressure figures can be significantly higher than the true ones, which leads to gross errors in the classification of patients with hypertension) and inaccuracies in determining Korotkoff sounds.
In his speech, Professor V.M. Gorbunov noted that the concept of “office dimension” is becoming more and more blurred with the advent of new varieties of it. Today, there are measurements in clinical studies (carefully standardized, carried out according to a protocol), measurements in real practice - “casual” (without strict compliance with the requirements for the procedure and giving inflated indicators) and automatic office measurements (has many advantages, but gives somewhat underestimated blood pressure numbers and requires additional resources; not yet available in our country).
As Vladimir Mikhailovich said, one of the serious disadvantages of “casual measurements” is that in 20-45% of cases it leads to errors in classifying a patient with hypertension. In addition, during such measurements, high variability of results is noted; systolic pressure is overestimated by 10-15 mm Hg. Art. In addition, the results obtained weakly correlate with signs of target organ damage due to hypertension.
Professor V.M. Gorbunov also spoke in detail about the phenotypes of arterial hypertension and additional indicators of blood pressure, recalled the differences in the recommendations of the European and American Cardiological Societies for diagnosing and determining the degree of arterial hypertension, and provided a new screening algorithm for determining blood pressure phenotypes.
The report also discussed the practical significance of various indicators of blood pressure variability. In conclusion, V.M. Gorbunov focused on new approaches to determining ambulatory blood pressure standards based on assessing the risk of cardiovascular complications. New standards make it possible to more accurately formulate a diagnosis in patients with “problematic” blood pressure phenotypes (masked hypertension and “white coat” hypertension).
Medical significance of the oscillometric method of measuring blood pressure
Unfortunately, these so-called “major vascular diseases” are very common in Western European countries.
In the United States, the annual number of cases of myocardial infarction reaches 900 thousand, in the UK - 225 thousand;
in Germany - 275 thousand people suffer from this acute coronary disease. 40 - 50% of all these patients die during the initial 4 weeks of the post-infarction period. About 420 thousand patients in the United States, about 100 thousand in the UK and about 125 thousand patients in Germany suffer from stroke. 50% of them cannot continue their professional activities due to brain damage. Stroke and myocardial infarction account for 45% of all deaths in Western Europe. To prevent many diseases and maintain your health, along with such measures as a healthy lifestyle, balanced diet, control of cholesterol levels in the blood, quitting smoking, it is necessary to prevent an increase in blood pressure for as long a period of time as possible.
High blood pressure, however, is quite common. In developed countries, the overall prevalence of this disease reaches 20%. In the United States, for example, 56 million people suffer from this disease. The corresponding figures for Great Britain are 13 million, and for Germany about 16 million. Fortunately, modern medicine offers a wide range of therapeutic measures, including diet, physical activity, and pharmaceutical interventions. Any therapy, however, requires, first of all, a correct diagnosis of arterial hypertension. Only a doctor can make a correct diagnosis. Unfortunately, results obtained in the doctor's office alone are not sufficient to accurately diagnose hypertension: First, patients in the doctor's office are often subject to the so-called "white coat effect", which leads to an artificial increase in the patient's blood pressure level. Secondly, working patients do not have the opportunity to visit a doctor frequently. Therefore, when assessing blood pressure levels during the day, patients need to measure their blood pressure themselves. Measurements can be taken both at the workplace and at home. Measurement data should be entered into a “measurement diary” and presented to the doctor during visits. Today, there are two methods for measuring blood pressure: using automatic tonometers that measure pressure using the oscillometric method and using devices that measure pressure using the auscultatory method. The auscultatory method of measuring blood pressure, also called the Riva-Rocci method, is based on the detection of arterial pulsation sounds, heard as the blood tone passes under a cuff wrapped around the patient's shoulder. Most auscultatory devices are hand-held devices, that is, patients use a stethoscope to listen to the sounds of the pulse and determine the systolic and diastolic pressure based on the nature of the sound. This method only works well if patients are properly trained and have the appropriate experience. Unfortunately, many patients suffering from arterial hypertension are elderly. They often have reduced hearing and are unable to properly use hand-held auscultation devices. There are several automatic auscultatory tonometers on the market. Their disadvantage is their high sensitivity to noise interference. The microphone, which is part of these devices, perceives various sound signals that interfere with correct measurements. More than 10 years have passed since the oscillometric measurement method began to be used in devices for measuring blood pressure. This technique allows you to assess the level of arterial pressure using a cuff placed on any limb. When measuring at home, pressure is measured either at the shoulder or at the wrist. Shoulder devices show more accurate results. There is a camera inside the cuff that detects pulse changes in the flow of blood passing just under the cuff. All changes in pressure are recorded during the measurement. The oscillometric method has two main advantages:
- patients do not need to have the skills to interpret the nature of pulse changes
- patients do not have to engage in self-assessment of sound signals
In this case, it is important to observe some basic conditions: take measurements only at rest, any movements should be excluded, and the cuff should be at the level of the heart. No special skills are required for these measurements. Today, the buyer is offered a wide range of oscillometric instruments. The accuracy of these devices is very high, but it is not the same among different manufacturers, which is due to the design features of the devices and the use of technology in their production.
This refers to the degree of possibility:
- suppression of extraneous noise
- correct interpretation of heart rate changes
- low heart rate measurements
- measuring very low or very high pressure
Due to incorrect behavior of patients during measurement, in particular due to lack of rest, the result of one measurement differs from another. Such errors are not a technology error; they are caused by the instability of the pressure level itself. Since the pressure level changes dynamically, one-time measurements should not be practiced. To find out the true level of pressure, it is necessary to take a series of repeated measurements. It is very important that patients undergoing treatment for high blood pressure prepare materials with measurement data for their treating physicians (keeping measurement diaries). They play a significant role in prescribing further treatment.
Conclusion: Oscillometric blood pressure measurement technology is reliable for accurately assessing blood pressure levels in patients suffering from hypotension or hypertension. Despite some technical and psychological limitations, this technology has important medical significance and is unique. Klaus Forstner
Doctor, MD cd Dipl.-Ing. Tamm, May 16th, 2002
Auscultatory method of measuring pressure
Auscultation (from the Latin auscultatio) is a method of studying internal organs, which is based on listening to sound phenomena associated with their activity.
A typical device for measuring pressure using the Korotkoff method is a mechanical tonometer with a phonendoscope. There are mercury and electronic tonometers that use the auscultatory method, but they are not widely used, so we will consider the procedure using a classic device.
How to correctly measure blood pressure with a mechanical tonometer.
- The cuff is placed on the bare shoulder and secured tightly with Velcro so that one finger can be inserted under the cuff.
- The edge of the cuff with the air tube should look down and be located 2 - 3 cm above the elbow.
- The head of the stethoscope is located above the radial artery in the bend of the elbow.
- Using a pump, air is pumped into the cuff, approximately 30 mmHg above the point at which arterial pulsation is no longer detectable.
- Using the release valve, air is slowly released from the cuff. At the same time, we listen to the pulse tones and monitor the pressure gauge needle. The indications at which sounds appear are noted as systolic (upper) pressure. When the sounds disappear, we detect the diastolic (lower) pressure.
Classification of Korotkoff sounds.
The sounds that we listen to using a phonendoscope can be divided into 5 phases:
01When the pressure approaches systolic, tones appear, the volume of which gradually increases.
02The intensity of the tones increases, and “russling” sounds appear.
03Tones reach maximum.
04The tones weaken and become quieter.
05Tones completely disappear.
In case of cardiovascular problems, deviations from this algorithm are possible.
Advantages of the auscultatory method.
- A generally accepted method of measuring blood pressure throughout the world, it is considered the standard of accuracy.
- High resistance to heart rhythm disturbances. Arrhythmia will not interfere with obtaining an accurate result.
- Hand movements or vibration during measurement do not have a significant effect on the correctness of the readings.
Disadvantages of measuring blood pressure using the Korotkoff method.
- A technically complex method that requires training and special skills. There is a high risk of human error. Not suitable for people with impaired hearing or vision.
- High sensitivity to extraneous noise and interference. Frequent errors due to displacement of the cuff and stethoscope.
- Determining blood pressure is difficult with weak Korotkoff sounds and such phenomena as “auscultatory failure” and “endless tone”.
- The need for regular checking and calibration of the sphygmomanometer.