Doctors Cost
Price list Doctors clinic
Anemia is a whole category of syndromes characterized by a decrease in hemoglobin concentration and the number of red blood cells. This condition is diagnosed only by the results of laboratory tests; it is impossible to determine the disease by eye. Symptoms of anemia in adults can vary greatly. Therefore, the direction of treatment depends on the general state of health, the causes of the disease, age and gender, and concomitant pathologies.
Anemia - what is it and how dangerous is it?
This disease is also called anemia. This is a clinical-hematological syndrome that can occur as a consequence of one or another pathology. Hemoglobin protein is synthesized in the bone marrow with the participation of iron and is a component of erythrocytes - red blood cells. It delivers oxygen to the tissues and also helps to utilize carbon dioxide, delivering it to the lungs.
Such an important function easily explains the dangerous consequences of anemia. Firstly, even in conditions of a lack of iron in the diet, the body will fight anemia with all its might: first there will not be enough iron in the tissues and organs, and only lastly in the blood. This means that anemia often accompanies serious bone marrow diseases, tumors, and severe hematological diseases. It is important to pay attention to anemia as early as possible for this reason.
Secondly, a decrease in hemoglobin levels can lead to the following consequences:
- weakening of protective forces and increased susceptibility to aggressive environmental factors;
- decreased physical endurance and tolerance to intellectual stress;
- high risks of developing heart disease;
- high risks of developing purulent-septic processes.
Pregnant women deserve special attention. Anemia during pregnancy can lead to a high probability of spontaneous abortion, fetal malnutrition and intrauterine growth retardation, the appearance of hypoxia, and discoordination of labor. Physiological blood loss during childbirth or during a cesarean section will not cause complications in a healthy woman, but in an expectant mother with anemia it can also cause serious consequences.
Clinical manifestations of iron deficiency
The clinical manifestations of iron deficiency are diverse and can be reduced to two main syndromes: hypoxic and sideropenic. Hypoxic syndrome combines symptoms common to all anemia: pallor, increased heartbeat, tinnitus, headache, weakness. Sideropenic syndrome includes taste perversion, dry skin, changes in nails, hair loss, angular stomatitis, burning tongue, and dyspepsia. The variety of clinical symptoms of iron deficiency can be explained by a wide range of metabolic disorders, which are caused by dysfunction of iron-containing and iron-dependent enzymes [6, 8, 9, 26, 27].
Symptoms that are less associated with anemia, but may be a manifestation of iron deficiency, include neurotic reactions and neurasthenia, decreased performance, muscle weakness and general tolerance to physical activity, disorders of metabolic processes in the myocardium, peripheral circulation and microcirculation, low-grade fever [6] . Exotic symptoms of IDA include urgency to urinate/defecate, urinary incontinence due to weakening of the sphincter apparatus, and difficulty swallowing due to atrophic changes in the esophageal mucosa [5, 12]. According to modern data, restless legs syndrome (Willis-Ekbom disease) may be one of the most common clinical manifestations of iron deficiency [28, 29].
Anti-infective immunity disorders in patients with impaired micronutrient status and IDA are complex [30]. On the one hand, iron deficiency prevents the development of pathogenic microorganisms that require iron for their own growth and reproduction. On the other hand, iron deficiency indirectly leads to disruption of cellular resistance mechanisms and to infections (decreased microbicidal activity of granulocytes, impaired proliferation of lymphocytes). In general, the predisposition of patients with IDA to the development of infectious diseases is not as great as previously thought. Moreover, treatment of IDA with parenteral iron supplements increases the risk of developing infections, probably due to the availability of administered iron for the rapid growth of pathogenic microorganisms [7, 26].
Symptoms of anemia
Symptoms of anemia and treatment options may vary in patients of different age groups, gender, and general health. The most characteristic signs are the following:
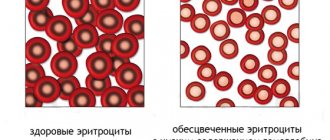
- pallor of the skin (from white to yellowish) and mucous membranes;
- hair loss (not patchy baldness, but uniform hair loss);
- brittle nails, changes in the structure of the nail plate, suddenly appearing white spots on the nails;
- change in taste sensations, burning sensation on the tongue;
- cracks in the corners of the mouth;
- menstrual cycle disorders in women;
- decreased physical activity, resistance to physical activity;
- muscle weakness;
- increased drowsiness;
- rapid mood changes, irritability;
- dizziness, periodic headaches, less often fainting;
- ringing in the ears, darkening or spots in the eyes;
- unusual gastronomic preferences, for example, the desire to taste paints, soil, chalk, etc.;
- pain behind the sternum, usually in the heart area.
In each specific case, not all of the listed symptoms may be observed. Sometimes anemia is discovered by chance, during the diagnosis of general health, when the patient came to the doctor for another reason. Thus, frequent respiratory diseases are a common consequence of anemia, and consulting a doctor allows you to identify the true causes of constant ailments.
Anemia: symptoms, treatment, prevention
Probably no one likes feeling lethargic, tired and overwhelmed. It’s one thing when such a condition appears periodically - after a hard day at work, severe stress, or after an illness. And it’s completely different when the state of “brokenness” becomes permanent: fatigue and weakness do not go away even after proper rest. And suddenly the skin becomes pale, the hands and feet are constantly freezing, the heart jumps out of the chest, the hair falls out and there is a ringing in the ears. This is a reason to sound the alarm and consult a doctor, since there can be a great many reasons for this condition. We will talk about one of them in our article. Today we will talk about anemia. What kind of disease is this? How dangerous is she? How to treat and prevent anemia? These, and more, questions will be answered by the therapist at the SMITRA Clinic, a doctor with more than 30 years of experience, Svetlana Aleksandrovna Marchenko.
What is anemia?
Erythrocytes (red blood cells) contain a complex protein - hemoglobin
, which is synthesized by the bone marrow with the help of iron. Its main function is to carry oxygen throughout the body: after delivering oxygen to the tissues, hemoglobin picks up carbon dioxide and delivers it to the lungs.
Anemia (or anemia)
is a condition in which there is a decrease in the amount of hemoglobin, sometimes with a decrease in the number of red blood cells. Because of this, the transfer of oxygen to tissues deteriorates and hypoxia occurs, i.e. oxygen starvation of tissues.
Causes and types of anemia
Anemia can be either an independent disease or a symptom or manifestation of a complication of another disease or syndrome.
Among the main causes of anemia are the following: 1.
Anemia that occurs when blood formation is impaired
.
These are, first of all, iron deficiency anemia (occurs due to a lack of iron in the body), anemia of pregnant and lactating women (during pregnancy and lactation, the volume of circulating blood in a woman’s body increases, which leads to its “dilution” and a drop in the proportion of hemoglobin in the total blood volume) . 2. Iron-saturated anemia
.
With such anemia, iron in erythrocytes is contained in sufficient quantities, but for various reasons cannot be used by the bone marrow for the synthesis of hemoglobin. Iron-saturated anemias include B-12 deficiency anemia, cancer anemia, helminthic anemia; anemia that occurs during infections. Anemia may occur when exposed to chemical reagents, radiation, medications, as well as due to immune disorders, gastritis, and enteropathies. 3. Anemia that occurs with increased blood destruction (hemolytic).
With this type of anemia, the lifespan of red blood cells is significantly shortened.
Hemolytic anemia can be either hereditary or acquired. In the hereditary form, the problem lies in genetic abnormalities in the structure or function of red blood cells. Acquired hemolytic anemia develops due to excessive destruction of red blood cells due to exposure to antibodies, toxins and other factors. 4. Anemia that occurs during acute or chronic blood loss.
Severe acute or chronic bleeding depletes the body's iron stores, leading to anemia.
Different forms of the disease differ in symptoms and complications. Without adequate treatment, anemia can be complicated by pathology of the cardiovascular system, premature birth, or even death.
What is the danger of long-term anemia?
As we said above, anemia leads to hypoxia - oxygen starvation of tissues. Therefore, even with a mild course, long-term anemia can cause serious harm to health. Prolonged hypoxia leads to metabolic disorders, accumulation of toxic metabolic products, and excessive load on the life-support organs - heart, lungs, liver, kidneys, brain. Against the background of chronic anemia, any acute disease - sore throat, viral infection, etc. – are much more severe and more difficult to treat.
Symptoms of anemia
Each type of anemia has its own manifestations, but a number of general signs of anemia can still be identified:
- weakness;
- noise in ears;
- dizziness;
- dyspnea;
- darkening of the eyes;
- heartbeat;
- decreased appetite;
- difficulty swallowing;
- pallor and dryness of the skin, as well as visible mucous membranes;
- hair loss;
- fragility, “striations” of the nails, sometimes their spoon-shaped concavity;
- cracks in the corners of the mouth;
- decreased blood pressure;
- from the gastrointestinal tract, glossitis (inflammation of the tissues of the tongue), atrophy of the mucous membranes of the esophagus, atrophic gastritis, pain in the left hypochondrium are noted.
Iron deficiency anemia is characterized by a perversion of taste (addiction to chalk, lime, coal, earth, tooth powder, ice). Hemolytic anemia can be manifested by yellowness of the skin and sclera, enlargement of the liver and spleen, dark urine and feces.
As we can see, the manifestations of anemia can be completely diverse. Therefore, if your health worsens or if the symptoms described above or any other symptoms appear, we recommend that you immediately consult a doctor.
How to diagnose anemia?
Laboratory tests help diagnose the disease, because it is impossible to determine the disease by eye.
Only correct diagnosis will help choose the right tactics for further treatment and, accordingly, guarantee a successful outcome for the patient. If you suspect one or another type of anemia, your doctor will definitely prescribe blood tests: general and biochemical. Changes in indicators (hemoglobin, iron, red blood cells, ESR, vitamin B12, etc.) will not only answer the question: is there anemia, but will also help the doctor choose the appropriate treatment path.
In some cases, laboratory blood tests alone are not enough, so the patient is prescribed a myelogram - a bone marrow test. A myelogram helps in the differential diagnosis of blood diseases.
Also, the doctor will definitely advise you to conduct a stool test for occult blood, stool for worm eggs and protozoa, caprogram, and, if necessary, stool for calprotectin (a specific marker of intestinal inflammation).
To exclude acute and chronic blood loss, fibrogastroduodenoscopy (FGDS) and colonoscopy are performed; if these procedures are impossible, irrigoscopy is prescribed. Consultation with a proctologist, ultrasound of the abdominal organs and kidneys are also indicated. Women are recommended to consult a gynecologist.
At the initial stages, anemia is treated by a general practitioner. Then, if necessary, the patient can be referred to a hematologist - a specialist who deals with the prevention, diagnosis and treatment of blood and hematopoietic organs.
Treatment of anemia
There are a huge number of types of anemia.
And they are all treated differently. That is why when treating an illness it is so important to take into account the cause that caused it. In case of bleeding, this is, first of all, the fight against bleeding; for inflammatory diseases - antibiotics, hormones; for chronic renal failure - hemodialysis; for iron deficiency anemia - iron supplements, sometimes even blood transfusions; for B12-deficiency anemia - injections of vitamin B12; if there is a lack of vitamin B9 (folic acid), use folic acid supplements. Treatment of any anemia can only be prescribed by a qualified doctor after a thorough examination!
Otherwise, all attempts to independently increase hemoglobin will be ineffective, in vain, or even dangerous.
Is it possible to treat anemia with folk remedies?
To treat anemia, first of all, you need to contact a specialist and receive a course of drug therapy.
Folk remedies can be used as auxiliaries when undergoing the main course of treatment prescribed by the doctor. For example, rose hips contain a huge amount of vitamins and other useful substances - iron, copper, magnesium. Rosehip decoctions and infusions are useful for iron deficiency anemia. Garlic is also an effective aid for anemia, and if you don’t want to eat it because of the smell, you can take garlic infusion.
Folk remedies cannot be the main treatment for anemia! If you suspect a disease, be sure to consult a doctor!
Nutrition for anemia
Pay close attention to the foods in your daily diet.
Do they have enough iron? To prevent a deficiency of this important element in the body, it is necessary to eat foods rich in iron. Both animal and plant products are rich in iron. Animal iron is found in meat, organ meats, poultry and fish. Moreover, the darker the meat, the more iron it contains. This type is absorbed most efficiently (from 15 to 30%). Among plant products, the richest in iron are legumes, spinach, apples, cereals, nuts, and dried fruits. Iron from plant foods is absorbed less efficiently by the body. To improve the absorption of iron from plant foods, they should be taken with foods rich in vitamin C (citrus fruits, greens, tomatoes, bell peppers, rose hips, cabbage). Folic acid also goes well with iron. It can be found in grain bread, corn, avocado, rice, oatmeal, barley, and pearl barley. It is not recommended to simultaneously consume foods rich in iron and calcium (for example, buckwheat with milk), since these two elements make it difficult to absorb each other. In addition, it is not recommended to drink tea and coffee with foods rich in iron. The tannin contained in drinks prevents iron from being absorbed.
When trying to boost your iron levels through food, don't overdo it! Large amounts of iron-rich foods can lead to an increase in iron levels, which can lead to new problems.
Anemia is a common and serious disease that should not be left to chance. In order to avoid the development of anemia and other diseases, it is necessary to undergo an annual preventive examination: take a general blood and urine test, feces for occult blood, undergo fluorography, visit a therapist, urologist, dentist for women - a gynecologist.
If there are signs of chronic bleeding and inflammation, as well as any symptoms of anemia, consult a doctor immediately! The therapist will prescribe the necessary examination and, based on its results, adequate treatment, which will help you return to a healthy, fulfilling life as soon as possible!
Be healthy!
The material was prepared with the participation of the physician-therapist of the SMITRA Clinic, Svetlana Aleksandrovna Marchenko.
© 2010-2021 SMITRA. All rights reserved. No material on this site may be copied or used without written permission except for private, non-commercial viewing.
Differences between anemia in adults and children
According to WHO, about 2 billion people in the world suffer from anemia. The majority are children of different ages. Almost half of them are preschoolers, and a little more than a quarter are young school-age patients. And in adults, the disease occurs quite often. This syndrome is dangerous for both children and adults, and in adults the treatment period is somewhat longer.
Anemia in children may be associated with a specific cause: periods of rapid growth. The mechanisms of hematopoiesis are still imperfect, and the growth spurt requires an increased amount of nutrients. This may be associated with a temporary decrease in hemoglobin levels in the blood. However, this is still not a variant of the norm, but a syndrome that deserves close attention from a doctor. Anemia can lead to decreased defenses, poor weight gain, loss of appetite, weakness, and tearfulness. Timely methods of diagnosing and treating anemia will allow you to correct the condition and prevent complications.
The most dangerous complication of iron deficiency anemia (IDA) in adults is hypoxic coma. With high blood loss, it can cause death. Therefore, it is important to consult a doctor in time.
Prevention to be
Of course, with a diagnosis of iron deficiency anemia, a person must adhere to a rational diet, but, according to medical research, no diet can completely compensate for the microelement deficiency. This is possible with drugs containing a high content of ferric iron (Fe III).
Iron supplements are prescribed only by a doctor, focusing on the individual characteristics of the course of anemia. The medicine is prescribed for a fairly long period, since the hemoglobin level increases only at the end of the third week of such therapy, so it is extremely important to be patient and persistently complete the course of treatment.
After all, this is the only way to get rid of the oppressive state of iron deficiency, avoid the development of dangerous complications and maintain your newly acquired “iron” health for many years.
As an advertisement
Why does anemia occur?
Anemia can be caused by many factors. There is often a combination of causes that quickly lead to blood disorders. The most common factors for the development of anemia:
- diet features. This is the most insidious reason. The lack of food rich in iron and B vitamins may not be taken seriously by a person. This is observed with a meager diet in women trying to lose extra pounds, the need to follow a certain table for gastrointestinal diseases, etc.;
- dysfunction of the digestive system. Even a complete diet does not guarantee the absence of anemia if iron cannot be absorbed in full due to gastrointestinal diseases. Iron absorption occurs in the stomach and upper small intestine. Diseases of these organs can lead to disruption of the process and the development of IDA;
- diseases leading to disruption of red blood cell production in the bone marrow. Such diseases include pathologies of the kidneys and endocrine system, protein depletion, chronic infections, cancerous tumors;
- hemolysis. This is a condition in which red blood cells are destroyed prematurely. Normally, physiological hemolysis occurs no earlier than after 120 days—that’s how long the red blood cell “lives.” In pathological conditions, the lifespan of red blood cells decreases, causing anemia. This may be due to long-term drug therapy, infectious diseases, rheumatism, systemic diseases (scleroderma, etc.), kidney diseases, etc.;
- chronic blood loss. Blood loss is a common cause of anemia. These include heavy menstruation in women or a short (21 days or less) menstrual cycle, frequent nosebleeds or bleeding gums, gastrointestinal bleeding, non-healing wounds in people with diabetes, previous surgeries, childbirth, etc.
Anemia is always the result of an underlying disorder, so it is important to get accurate information about the causes. It is not recommended to engage in self-diagnosis and self-medication. Taking iron supplements can correct the condition, but will not get rid of the underlying disease, so it will not be fully effective and there is a high probability of relapse.
The approach to treating anemia depends on what causes the disease. Thus, secondary causes of the development of the syndrome include:
- refusal of protein foods, fasting due to life circumstances or beliefs. If a person is forced or prefers to give up food of animal origin and does not find a replacement for it in terms of iron content, deficiency and associated anemia develop;
- pregnancy. Hormonal changes, an increased need for vitamins and microelements can cause deficiency, including iron; anemia in pregnant women develops quite often. It is important to regularly visit an obstetrician-gynecologist and get tested on time so as not to miss possible violations;
- blood donation. Although blood donation is carried out taking into account safe blood loss, the risks of developing anemia increase. You should consult your doctor if you are acting as a donor;
- professional sports or increased physical activity. This is due to the fact that muscles require increased amounts of iron. The peculiarity of this cause is that anemia occurs in an erased form, because usually an athlete leads an active and healthy lifestyle. It is important to pay attention to fatigue, intolerance to previously habitual stress, and shortness of breath.
Prevalence of IDA
Iron deficiency anemia in women is a common pathological condition. Thus, according to WHO (2015), severe iron deficiency is observed in every third woman of reproductive age and in every second pregnant woman, being an important cause of chronic fatigue and poor health, and the third most common cause of temporary disability in women aged 15– 44 years old [12, 19]. In the Russian Federation, despite active preventive and therapeutic measures, the prevalence of IDA remains very high. For example, in Moscow, anemia occurs in almost 38% of gynecological patients [20, 21] and is the most common concomitant pathological process and the first manifestation of the underlying disease, determining the severity of its course and treatment tactics. The main reasons for the development of IDA in women are heavy menstrual bleeding, pregnancy, childbirth (especially repeated ones) and lactation. Anemia often accompanies uterine fibroids, adenomyosis, hyperplastic processes in the endometrium, and ovarian dysfunction. During normal menstruation, 30–40 ml of blood is lost (which is equivalent to 15–20 mg of iron). The critical level corresponds to a blood loss of 40–60 ml, and with a blood loss of more than 60 ml, iron deficiency develops. In women suffering from abnormal uterine bleeding of various origins, the amount of blood lost during one menstruation can reach 200 ml (100 mg of iron) or more. In such situations, the loss of iron exceeds its intake and IDA gradually forms [20].
The most important medical and social problem is anemia in pregnant women, which, according to WHO, is detected in 24–30% of women in economically developed countries and in more than 50% of women in countries with low economic levels [3, 22].
A survey of pregnant women conducted as part of clinical studies in the 2000s showed a high incidence of anemia even among residents of prosperous European countries. Thus, in Belgium (n=1311), Switzerland (n=381) and Germany (n=378) iron deficiency was diagnosed in 6% and 23% (serum ferritin (SF) <15 μg/l) in the first and third trimesters, respectively, of Belgian women; in 19% (SF<12 µg/l) - in Switzerland and Germany. The prevalence of IDA (Hb <110 g/L, SF <15 μg/L) was 16% in Belgium and 3% in Switzerland, although 65–66% of Belgian and Swiss women received dietary iron supplementation during pregnancy. In Germany, IDA was diagnosed in 12% of women [23].
In Russia, according to the Ministry of Health, the incidence of anemia in pregnant women varies from 39% to 44%, in postpartum women - from 24% to 27% [24]. A 2021 systematic review and meta-analysis found that in low- and middle-income countries, pregnancy anemia increases the likelihood of preterm birth by 63%, low birth weight by 31%, perinatal mortality by 51%, and neonatal loss by 2 ,7 times [25].
During pregnancy, there is a significant physiological increase in the need for iron for the normal functioning of the placenta and fetal growth. The total amount of iron required for a normal pregnancy is 1000–1200 mg. To complete a normal pregnancy without developing iron deficiency, a woman must have iron stores in the body at conception of ≥500 mg, which corresponds to an SF concentration of 70–80 μg/L [20, 23].
Classification of anemia
Anemia is classified according to the color index, which shows the level of saturation of the red blood cell with hemoglobin. The following types of syndrome are distinguished:
- hypochromic (iron deficiency, thalassemia, anemia associated with a lack of vitamin B6, etc.);
- normochromic (hemolytic, posthemorrhagic, i.e. resulting from blood loss/surgery, aplastic, etc.);
- hyperchromic (vitamin B12 deficiency, folate deficiency, etc.).
We see that anemia is not always synonymous with iron deficiency. Deficiency of B vitamins can also cause the development of the syndrome, and quite often it is associated with diet or absorption of nutrients in the intestines. And in this regard, independent diagnosis is impossible: only a doctor can determine the type of anemia, identify the causes and correctly correct the condition.
Treatment also depends on the severity of the anemia. It is determined by the severity of the decrease in hemoglobin levels. There are three degrees of severity:
- light. Hemoglobin level from 90 g/l;
- average. Hemoglobin level 70–90 g/l;
- heavy. Hemoglobin level is less than 70 g/l.
About the disease
What is this? Anemia (anemia) is a decrease in hemoglobin content and/or a decrease in the number of red blood cells per unit volume of blood, leading to a decrease in the supply of oxygen to tissues.
What caused it? The causes of anemia are varied and may be closely related to the following factors:
- Somatic diseases - liver and kidney diseases, autoimmune, infectious and inflammatory processes.
- Acute and chronic blood loss. Acute is considered blood loss with a blood volume of more than 500-700 ml (in adults), which occurs within a short period of time. It can be visible (bleeding from a wound, bloody vomiting, uterine and nasal bleeding) and initially hidden (bleeding into the intestines, into the abdominal cavity and/or pleura, extensive hematomas). Chronic blood loss develops against the background of minor but prolonged blood loss (heavy and prolonged menstruation, stomach ulcers, cancer, hemorrhoids, hemodialysis procedures). Over time, even minor losses deplete the body's iron stores when the amount of iron the body loses exceeds its intake from food. As a result of iron deficiency, hemoglobin synthesis is impaired
- Poor nutrition, lack of vitamins and microelements. Anemia develops against a background of deficiency of iron, vitamin B12 and folic acid. This may be due to both a lack of substances necessary for the body in the diet (for example, with strict diets or vegetarians), and with a decrease in iron absorption as a result of various diseases of the duodenum and the initial parts of the small intestine (enteritis, tumors, conditions after operations on the small intestine). intestines). In conditions that cause a decrease in the level of blood proteins that carry iron (nephrotic syndrome, impaired protein-synthetic function of the liver, malabsorption syndrome, nutritional deficiency), a decrease in the amount of iron and, as a consequence, anemia may also be observed.
- Hematopoietic disorder. Anemia occurs when there is insufficient formation of red blood cells in the bone marrow (for example, when the bone marrow is depleted or damaged by toxic substances, ionizing radiation), against the background of premature and excessive destruction of red blood cells in the bloodstream (for example, during hemolysis). Anemia can also occur with the formation of secondary foci (metastases) of tumor cells in the bone marrow, disruption of the production of the non-protein part of hemoglobin (heme) and the accumulation of its toxic products, as well as disruption of the regulation of red blood cell synthesis (decreased production of the hormone that stimulates the growth and reproduction of red blood cells - erythropoietin ).
Depending on the causes, anemia is classified as iron deficiency, caused by blood loss or insufficient iron intake or absorption; B12 deficiency and folate deficiency, caused by insufficient intake or absorption of cyanocobalamin and folic acid, respectively; aplastic, caused by a violation of the formation of red blood cells in the bone marrow; and hemolytic, in which the red blood cells in the body are destroyed too quickly. The most common form of anemia is iron deficiency - it is diagnosed in 80-90% of patients who have a reduced number of red blood cells and/or hemoglobin in the blood. Iron deficiency conditions develop gradually. Initially, a negative iron balance is created, in which the body's needs for it and its losses exceed the amount it receives from food. This may be due to blood loss, pregnancy, breastfeeding, growth spurts during puberty, impaired absorption of micronutrients in the gastrointestinal tract, or insufficient consumption of foods containing iron, as with vegetarianism.
Normally, iron is absorbed in the small intestine, but in some chronic gastrointestinal diseases, malabsorption syndrome occurs - impaired absorption of vitamins, microelements and other beneficial substances from food. In the blood, iron is transported by the protein transferrin to places where it is consumed or accumulated. In iron deficiency conditions, the amount of free transferrin in the blood increases, and the level of serum iron decreases. The production of hemoglobin in the bone marrow is not so active, as a result of which iron deficiency anemia develops with all the clinical manifestations of anemia.
Features and diagnostic methods
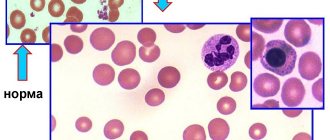
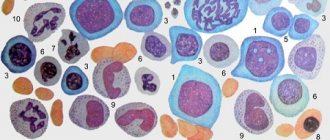
Diagnosis of anemia includes not only determining the fact of a decrease in hemoglobin levels. The doctor must understand the causes, assess the general state of health, and exclude severe pathologies that occur in a latent form, if they were not detected earlier. For this purpose, laboratory tests may be involved: a detailed clinical blood test is required. It will help assess the size, structural and other characteristics of blood cells.
The content of hemoglobin, erythrocytes, platelets, leukocytes, and several calculated erythrocyte indices are assessed. These indicators allow you to obtain data on the size, hemoglobin saturation, and uniformity of red blood cells. Determination of reticulocytes (young red blood cells) helps to understand the nature of anemia, as well as assess the reactivity of the hematopoietic system to the pathological condition. This is also important for monitoring treatment - the doctor can evaluate the response to the course of therapy.
Determination of erythrocyte parameters includes assessment of the following indicators:
- red blood cell count;
- hemoglobin concentration;
- average erythrocyte volume;
- hematocrit;
- width of distribution of red blood cells by volume;
- normoblasts.
The average volume and diameter of red blood cells are also assessed. An increase in these parameters may indicate a vitamin B12 deficiency. A decrease indicates a lack of iron.
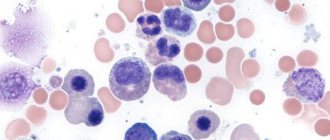
Reticulocytosis or quantitative indicators of immature red blood cells may indicate certain features of bone marrow activity. In aplastic anemia associated with bone marrow suppression, the indicator may drop to zero. Reticulocytosis increases with blood loss and hemolytic anemia.
The doctor will also pay attention to those blood parameters that are not directly related to red blood cells. For example, an increase in platelet levels may be a consequence of IDA due to chronic blood loss. If leukocytes and platelets are reduced, we can talk about aplastic anemia. Detection of blast cells requires special attention; there is a high probability of acute leukemia.
Although laboratory diagnosis is critical, it is important to resort to other research methods. An examination is mandatory - the doctor evaluates the color of the skin and mucous membranes. Palpation helps to suspect possible disorders of internal organs and tumors. A thorough survey allows you to identify lifestyle features, probable causes, and the duration of symptoms.
If you have symptoms of anemia, it is important to consult a general practitioner or hematologist. He will order the necessary tests and make suggestions as to the reasons. To clarify them, it is sometimes necessary to resort to additional diagnostic tools:
- fibrogastroduodenoscopy. Assessing the condition of the mucous membranes of the esophagus and stomach will help in identifying gastric bleeding;
- Ultrasound of the liver and kidneys;
- examination of the pelvic organs in women;
- CT or MRI if indicated;
- colonoscopy;
- X-ray of the lungs, etc.
A complete list of diagnostic methods is not required: a specialist will find out the possible causes and refer you to certain studies according to indications. If necessary, he can refer you to another doctor. So, if the cause of anemia is heavy and prolonged menstruation or a short cycle, an examination by a gynecologist will be required. Detection of gum problems (bleeding) and symptoms of periodontal disease will require a visit to a periodontist. Frequent nosebleeds are a reason to consult an otolaryngologist, assess blood pressure parameters, etc.
Diagnosis of IDA
Diagnosis of IDA is based on the characteristic clinical and hematological picture of the disease and the presence of laboratory evidence of absolute iron deficiency.
When performing a physical examination of patients with suspected IDA, it is necessary to pay attention to the characteristic signs of sideropenic and hypoxic syndromes given earlier. However, the symptoms of anemia and sideropenia have low diagnostic value and do not allow a reliable diagnosis of IDA to be established. Laboratory tests are of decisive importance in the diagnosis of IDA.
First of all, in patients with anemic syndrome, a general (clinical) blood test is performed with an assessment of hematocrit, the level of erythrocytes, reticulocytes, the average content and average concentration of hemoglobin in erythrocytes and the size of erythrocytes [17]. With IDA, there is a decrease in the level of hemoglobin, hematocrit, the average content and average concentration of hemoglobin in erythrocytes, and the average volume of erythrocytes. The red blood cell count is usually within normal limits. Reticulocytosis is uncommon but may be present in patients with bleeding. Typical morphological signs of IDA are hypochromia of erythrocytes and anisocytosis with a tendency to microcytosis [5, 6, 31, 32].
However, the listed morphological characteristics do not allow distinguishing IDA from the so-called anemia of chronic diseases, which is based on redistribution of iron deficiency associated with the presence of a focus of inflammation, infection or tumor in the body. Therefore, all patients with suspected IDA need to examine serum indicators of iron metabolism - ferritin, transferrin and iron levels, total serum iron binding capacity (TIBC), and also determine the calculated indicator - transferrin iron saturation coefficient (TIS) [6, 7, 19, 32 ].
Distinctive signs of true IDA are a low level of SF, reflecting the depletion of tissue iron reserves, and increased levels of PVSS and transferrin. Serum iron levels and the IF coefficient are in typical cases reduced, but the presence of normal and even elevated values does not exclude the diagnosis of IDA, since taking iron-containing drugs on the eve of the study, a meat diet, or a previous (10–14 days before) red blood cell transfusion can greatly distort the serum iron level and, accordingly, the NTG coefficient, which must be taken into account when assessing the results of the study [7, 9, 26].
The development of IDA is preceded by a period of latent iron deficiency, the laboratory criteria of which are low levels of serum iron and ferritin against the background of normal hemoglobin levels.
The study of serum indicators of iron metabolism must be combined with basic studies, which include: general urine analysis, biochemical blood test (total protein, albumin, total bilirubin, direct bilirubin, AST, ALT, creatinine, urea, alkaline phosphatase, γ-glutamine transpeptidase) with determining the main indicators of the functional state of the liver, kidneys, pancreas, as well as screening for viral hepatitis B and C, HIV infection, syphilis. Carrying out these studies is necessary for the correct interpretation of serum indicators of iron metabolism, since the state of iron metabolism, on the one hand, is an “endocrine function of the liver”, on the other hand, it changes significantly in the presence of inflammatory, destructive or tumor processes in the liver and other vital organs [ 7, 9, 26].
It is important to note that microcytic hypochromic anemia is a characteristic morphological sign of β-thalassemia, severe forms of which are associated with profound anemia and pronounced signs of iron overload (increased levels of serum ferritin and LTFA, decreased levels of transferrin and TBL). However, mild subclinical forms of thalassemia, occurring with mild microcytic hypochromic anemia, are often regarded as iron deficiency without studying serum indicators of iron metabolism, which entails the prescription of inadequate ferrotherapy, which can lead to the accelerated development of tissue iron overload. In this regard, IDA must be differentiated from anemias occurring with iron overload: α- and β-thalassemia, porphyria, lead intoxication [9, 32].
Treatment of anemia
Clinical recommendations for the treatment of anemia depend on many factors: gender, age and condition of the patient, type and severity of the syndrome. There are several general principles that apply in medical practice. These include the following:
- Mandatory diet correction for B12 deficiency and iron deficiency anemia. This complements the main course of treatment - taking medications that will compensate for the lack of substances;
- timely correction of deficiency of vitamins and microelements in pregnant women;
- mandatory consultation with a specialist when identifying specific causes: chronic bleeding, features of the functioning of the reproductive system in women, etc.;
- examination by a specialist in cases where anemia has caused complications in organs and systems. For example, consultation with a cardiologist for angina pectoris, low blood pressure, etc.
An integrated approach allows you to cope with the cause of the syndrome, rather than mask the symptom, and also eliminate or correct the consequences of the disease.
Iron absorption
The body's daily need for iron in women is 1.5-2 mg.
In the gastrointestinal tract of a healthy person, only 10% of the total amount of iron eaten with food (1–2 mg) is absorbed. Improve iron absorption: ascorbic acid, fructose, citrates contained in fresh fruit juices, bananas, red beans, cauliflower. Reduce the absorption of iron from food: phosphates, tanning agents, complex polysaccharides, polyphenols, oxalates contained in cereals, eggs, cheese, tea. The effect of tea containing tannin is especially striking: when consumed, the absorption of iron is reduced sixfold (down to 2%). There are two types of iron in foods: heme (organic) and non-heme (inorganic). Heme iron is absorbed most completely. This iron is found in lean meats, fish, and poultry. The absorption of iron from animal products varies from 6% to 22%, while about 1% of iron is absorbed from plant foods. Fats (lard, butter and vegetable oil), soy protein, coffee, and dairy products inhibit the absorption of iron.
The human body contains about 3-4 g of iron, of which 70% is vital, active, 30% is deposited in tissues and 0.1% is transport. The bulk of iron is concentrated in hemoglobin (about 1500-3000 mg). In the depot (ferritin and hemosiderin of internal organs) there is from 500 to 1500 mg, in myoglobin and various respiratory enzymes - no more than 500 mg.
The main objectives of the treatment of anemia:
- eliminating the cause. Identification and elimination of the source of chronic blood loss, normalization of iron absorption in the intestines, reduction of blood loss during menstruation, etc.;
- replenishing the lack of important substances;
- prevention of the development of dystrophic changes in internal organs, restoration of their normal function.
It is important to remember that it is impossible to eliminate anemia with diet alone. This is explained by the fact that the absorption of iron from food is no more than 2.5 mg/day. From drugs, it is absorbed 20 times more. However, following a diet is very important as an addition to a course of drug therapy. Patients are recommended foods containing large amounts of digestible protein and iron.
Meat contains heme iron, which is absorbed by 30%. Also, liver, eggs and fish contain iron, which is absorbed by 10–15%. The microelement is also found in products of plant origin; absorption of Fe from legumes, spinach, soybeans, dill, and bread is up to 3–5%. It is advisable to include apples, pomegranates and pomegranate juice, beets, and buckwheat in your diet. But in terms of their overall benefits, the absorption of iron ions from them is limited, as demonstrated by numerous studies. That is why it is important to understand that eating apples will not help cure anemia; this is nothing more than a myth.
People who eat meat get more iron than those who are vegetarian. Strict vegetarianism can cause anemia because vegetables and grains contain substances that interfere with the absorption of iron. If you follow a normal, balanced diet, they do not entail serious consequences.
It is important to understand that a balanced diet helps cover the daily requirement, but will not eliminate iron deficiency. The basis of correction is drug therapy.
Blood transfusions (transfusions) are performed according to vital indications. They are usually carried out when hemoglobin drops below 50−40 g/l.
If the situation is not so severe, the doctor prescribes medication. IDA is corrected with oral medications; the course of treatment in adults is quite long. Interim monitoring is mandatory - detailed blood tests are performed. The principles of treatment in this case are as follows:
- prescribing iron supplements with a dose of divalent or trivalent iron sufficient for a person;
- supplementing the course of treatment with substances that enhance absorption. Succinic and ascorbic acid are used;
- refusal of antacids, oxalates and other drugs that reduce iron absorption whenever possible or recommendations for taking them at different times;
- therapy for at least 6–8 weeks until normalization and for at least another 4 weeks after improvement.
Let’s take a closer look at the recommendations about avoiding medications and foods that interfere with the absorption of iron. This can be prevented by phosphoric acid, calcium, tannin, phytin, and salts. Therefore, you should not drink tea, coffee, or Coca-Cola at the same time as taking iron.
For women suffering from long and heavy menstruation, not associated with diseases of the endocrine and reproductive systems, it is important to maintain monthly short courses of treatment: take average therapeutic doses of Fe for 3-5 days.
Clinical guidelines for the treatment of anemia dictate regular monitoring. The criterion for the effectiveness of therapy is an increase in reticulocytes at least three times 7-10 days after the start of treatment.
All iron preparations are classified into two groups: ionic (salt or polysaccharide compounds of ferrous iron) and non-ionic, consisting of a ferric iron complex.
Ferrous sulfate is included in mono- and polycomponent products and is well absorbed, and also has a relatively smaller list of side effects. Chloride compounds are absorbed less well and can also cause undesirable consequences: metallic taste in the mouth, dyspepsia, darkening of tooth enamel, etc. Modern treatment standards call for the use of ferrous or trivalent iron preparations.
Sometimes iron supplements are indicated to be administered parenterally. This is relevant for cases where there is a malabsorption in the intestine and other features. The main indications for drip infusion are the following:
- impaired intestinal absorption - malabsorption, previous surgery, etc.;
- intolerance to oral medications;
- the need for quick saturation. For example, in case of emergency surgery;
- treatment with erythropoietin: with it, the need for iron sharply increases, since it is actively consumed by red blood cells.
Important: parenteral administration requires no more than 100 mg/day. Otherwise, there is a risk of complications.
Treatment regimens for anemia associated with vitamin deficiency include additional intake of vitamin B12, folic acid and certain microelements.
Treatment of anemia associated with diseases of the hematopoietic organs and bone marrow tumors is developed individually and requires special attention to the cause.
Treatment of IDA
The goal of treatment for IDA is to replenish iron stores in the amount necessary to normalize hemoglobin levels (in women 120–140 g/l) and replenish tissue iron stores (SF>40–60 μg/l). For treatment and prevention, oral preparations of iron salts are used, most often ferrous sulfate; in recent years, iron fumarate, iron gluconate, or combination preparations have also been actively used. The quantitative and qualitative composition of iron medicinal preparations varies greatly; depending on this, the preparations are divided into high- and low-dose, single-component and combined. In accordance with the WHO recommendation, the optimal dose of iron for the treatment of IDA is 120 mg/day, for the prevention of iron deficiency - 60 mg/day [7]. Approximately 20% of patients develop diarrhea or constipation during treatment, which can be relieved with symptomatic therapy. Signs of stomach irritation, such as nausea and epigastric discomfort, are minimized by taking iron supplements with meals or reducing their dose. The use of high-dose iron supplements is accompanied by an increase in the frequency of side effects from the gastrointestinal tract. The duration of treatment is determined by the depth of the initial iron deficiency and can vary from 1 month. up to 3 months [6–9, 19].
There is now accumulating evidence that low-dose iron supplements, given in short courses (2 weeks per month) or in an alternative regimen (every other day for a month), have higher effectiveness and lower incidence of side effects than previously used high-dose preparations. including in the form of repeated (2–3 times a day) doses [7, 33, 34].
It is important to emphasize that high doses of iron supplements may be associated with oxidative cytotoxic effects of unabsorbed iron on the intestinal mucosa, which is clinically manifested by side effects such as nausea, vomiting, constipation or diarrhea. Other adverse effects of unabsorbed iron include disturbances in the composition of the gut microbiome, with a decrease in lactobacilli and bifidobacteria and an increase in potential pathogens ( Enterobacteriaceae
), which entails the development of inflammation and diarrhea [31]. Modification of the iron supplementation regimen, such as switching from daily to alternative and from 2–3 times to once a day, may increase the effectiveness of treatment and improve its tolerability [33–35].
An example of a modern iron drug is the combination drug Ferretab® comp. One capsule of the drug includes 3 mini-tablets containing iron fumarate 163.56 mg (equivalent to 50 mg of iron), 1 mini-tablet of folic acid 0.54 mg (equivalent to 0.5 mg of dry matter) and auxiliary components. The folic acid mini-tablet dissolves within minutes and is rapidly absorbed in the jejunum. Iron is built into the inert matrix of the mini-tablet, which avoids high concentrations upon release and prevents irritation of the mucous membrane. Iron absorption occurs directly in the duodenum and upper jejunum. During the passage of the mini-tablet through the intestines, continuous release and absorption of iron occurs, providing a prolonged effect of the drug with a single daily dose.
The advantage of the drug is its combined composition: active divalent iron (iron fumarate) and folic acid, which is a hematopoietic cofactor vitamin necessary for the growth and differentiation of bone marrow erythroid cells. This increases the effectiveness of treatment, as demonstrated in a meta-analysis in 2015 [36]. During pregnancy, folic acid protects the fetus from the effects of teratogenic factors [37].
The drug does not have a specific taste or smell of iron, does not stain tooth enamel, is well tolerated and convenient for use: 1 tablet per day.
Treatment with parenteral iron is recommended for IDA in cases of ineffectiveness, poor tolerability, or contraindications to the use of oral iron medications [4, 6, 7, 9]. The use of intravenous iron supplements is indicated primarily for absorption disorders due to previous extensive intestinal resection, for inflammatory bowel diseases (ulcerative colitis, Crohn's disease) and malabsorption syndrome, for chronic kidney disease in the predialysis and dialysis periods, and also if necessary to obtain a quick effect in in the form of replenishing iron reserves and increasing the efficiency of erythropoiesis (for example, before major surgical interventions) [6, 7, 9, 27].
Intravenous infusions of iron preparations are associated with the danger of anaphylactic shock (in 1% of cases), the development of iron overload and toxic reactions associated with the activation of free radical reactions of biological oxidation (lipid peroxidation) by iron ions.
Intramuscular administration of iron preparations has not been used for a long time due to low efficiency, the development of local hemosiderosis and the risk of developing infiltrates, abscesses and even myosarcoma at the injection site.
Features of prevention
Prevention of anemia should be carried out in case of hidden signs of iron deficiency or the presence of risk factors for the development of the syndrome. Thus, if there are grounds for the rapid development of anemia, it is important to examine the level of hemoglobin and serum iron annually. The following patients are at risk:
- blood donors, especially females;
- pregnant women, especially those with frequent pregnancies;
- women with long (more than 5 days), heavy menstrual bleeding, short cycle (21–25 days);
- children from multiple pregnancies, premature babies;
- children during growth spurts;
- people with dietary restrictions;
- people suffering from chronic bleeding. For example, with hemorrhoids, etc.;
- patients taking non-steroidal anti-inflammatory drugs;
- professional athletes and people engaged in active physical labor.
Detect Loss
There are many reasons for iron deficiency. Most often this is associated with chronic blood loss: monthly menstruation in women, gynecological diseases that occur with blood loss (ovarian dysfunction, uterine fibroids, endometriosis). Blood loss is often observed in diseases of the gastrointestinal tract (erosion of the esophagus and stomach, gastric or duodenal ulcers, Crohn's disease), as well as in diseases of the ENT organs, dental problems (periodontal disease), helminthiasis and oncology.
Article on the topic
Cold blood. Why we get chills The second most important factor in anemia is iron deficiency in food, which is facilitated by vegetarianism or an unbalanced diet with a predominance of refined foods.
Anemia also develops when iron absorption in the digestive tract is impaired due to gastroduodenitis, enteritis, enterocolitis, resection of the stomach or part of the small intestine, malabsorption syndrome.
Even high iron requirements at certain periods of life can lead to the development of anemia. For example, a period of intensive growth and puberty in children and adolescents, and in women - pregnancy and breastfeeding.
According to the World Health Organization, 25% of the world's population suffers from iron deficiency anemia. Women and children are at main risk for developing this disease.
Causes of anemia: what causes the disease
It should immediately be noted that anemia is not an independent disease. This is a symptom indicating some other diseases - infectious, inflammatory, oncological, helminthic infestations, pathological childbirth and menstruation, etc.
Anemia is also often a consequence of an external cause. This may be an incorrect diet or irregular nutrition, massive blood loss due to injury, injury, or surgery. No less dangerous are long-term, low-intensity bleeding that goes unnoticed for a long time. This happens with gastrointestinal diseases and cancer.
Most often, anemia is caused by diseases and conditions such as:
- haemorrhoids,
- menses,
- injuries,
- stomach ulcer and gastritis.
Anemia is also possible due to a lack of certain substances in the body, for example, vitamin B12 and folic acid, and in children - vitamin C and pyridoxine (vitamin B6). All these substances are necessary for the formation of hemoglobin and red blood cells. Vitamin B12 and folic acid may either be insufficient in food or poorly absorbed from food. The latter can occur with alcoholism and drug addiction, chronic liver and stomach diseases, and taking anticonvulsant medications.
Anemia can occur in conditions when the body requires an increased amount of iron, but not enough iron is supplied from the outside:
- lactation,
- adolescence (the body requires a lot of iron for growth),
- chronic diseases (pulmonary diseases, heart defects, abscesses, sepsis).
The following infectious diseases most often lead to anemia:
- tuberculosis,
- Chronical bronchitis,
- bacterial endocarditis,
- bronchiectasis,
- brucellosis,
- lung abscess,
- various mycoses,
- pyelonephritis,
- osteomyelitis.
Anemia also develops with collagenosis of various types:
- systemic lupus erythematosus,
- polyarteritis nodosa,
- rheumatoid arthritis.
Anemia can often develop during pregnancy. After all, the mother’s body requires an increased amount of iron to form the fetus, which most likely leads to a deficiency of the element. If a woman’s body usually consumes 0.6 mg of iron per day, then during pregnancy this figure increases to 3.5 mg.
The development of anemia can also be caused by taking drugs that suppress hematopoiesis, for example, some antibiotics or cytostatics.
Degrees
With mild anemia, symptoms are usually subtle. In order for the blood to be better saturated with iron, it is enough to improve nutrition and use iron-containing drugs. With moderate severity, symptoms become more pronounced. Weakness, frequent headaches, and dizziness appear. The severe stage is life-threatening. Signs of tissue hypoxia and cardiac dysfunction appear.
Dependence of the degree of anemia on hemoglobin content
| Degree of anemia | Hemoglobin content in blood, g/l |
| light | less than normal, but more than 90 |
| average | 70-90 |
| heavy | less than 70 |
It is also customary to distinguish between relative and absolute anemia. With relative, the relative content of plasma increases, but the number of red blood cells remains unchanged. With absolute, a decrease in the number of red blood cells is observed.
Hemoglobin levels vary depending on age and gender. For children under 12 years of age, the hemoglobin norm is the same for both sexes. Then, men have a slightly higher hemoglobin concentration than women.
Hemoglobin standards for children
| child's age | hemoglobin content, lower limit of normal, g/l | hemoglobin content, upper limit of normal, g/l |
| 0-2 weeks | 135 | 200 |
| 2-4 weeks | 115 | 180 |
| 4-8 weeks | 90 | 180 |
| 2-6 months | 95 | 140 |
| 6-12 months | 105 | 145 |
| 1-5 years | 100 | 140 |
| 5-12 years | 115 | 145 |
Hemoglobin norms for women
| age, years | lower limit of normal, g/l | upper limit of normal, g/l |
| 12-15 | 112 | 152 |
| 15-18 | 115 | 153 |
| 18-65 | 120 | 155 |
| over 65 | 120 | 157 |
Hemoglobin norms for men
| age, years | lower limit of normal, g/l | upper limit of normal, g/l |
| 12-15 | 120 | 160 |
| 15-18 | 117 | 160 |
| 18-65 | 130 | 160 |
| over 65 | 125 | 165 |
What is anemia in simple words?
Anemia is a lack of blood in the body (from the Greek prefix “an”, meaning negation, and “eima” - “blood”. Medicine sometimes calls this condition anemia. In a narrower sense, anemia often means an insufficient amount of oxygen in the blood, which In practice, it is expressed in a decrease in the concentration of red blood cells or hemoglobin.
Pseudoanemia (hydremia) should be distinguished from anemia. With hydremia, which can be observed, for example, during pregnancy, the total number of red blood cells remains unchanged, only the volume of the liquid component of the blood - plasma - increases.