ANTIHYPERTENSIVE DRUGS AND PHARMACEUTICAL GROUPS FOR INTERACTION
Preferansky Nikolay Georgievich Head of the Department of Medical and Pharmaceutical Information Systems, NP MIAC RAMS, Doctor of Philology, Prof.
Part I
This percentage increases with age, and almost half of the population over 50 years of age suffers from some form of hypertension. High blood pressure increases the risk of developing severe complications such as myocardial infarction and stroke, which lead to high mortality. According to WHO, mortality from these complications ranks first in the world.
The most relevant in these conditions is the correct selection of antihypertensive drugs (drugs), taking into account concomitant diseases and gender and age characteristics of patients. There are 17 groups of drugs that lower blood pressure. Medicines used for various forms of hypertension affect various parts of the endogenous regulation of blood pressure and are usually classified:
I. Drugs affecting the autonomic nervous system (neurotropic). II. Drugs affecting the humoral system (renin-angiotensinotropic). III. Drugs that change the muscle tone of the vascular wall (myotropic) IV. Medicines that change the volume of circulating blood (diuretics). V. Fixed-dose combination antihypertensive drugs.
Currently, 5 main groups are most often recommended for the treatment of hypertension:
- First: angiotensin-converting enzyme inhibitors.
- Second: diuretics.
- Three: beta blockers
- Fourth: calcium antagonists.
- Fifth: angiotensin type I receptor blockers.
When prescribing drugs from different pharmacological groups in combination, it is extremely important to consider the interaction of antihypertensive drugs both with each other and with other groups of drugs that patients may use. Most often, drugs from the following pharmacological groups are used with antihypertensive drugs: Antiplatelet agents, Anticoagulants, Antiatherosclerotic agents, Antibiotics, NSAIDs, Antidiabetic agents, Antiviral agents. When predicting the results of interactions between drugs that can be prescribed, it is important to warn the patient against adverse reactions, and in some cases, plan the correct dosage regimen in order to reduce side effects and reduce the risk of toxicity.
Timely reduction of blood pressure and maintaining it at a constant normal level with the help of antihypertensive drugs allows you to:
- slow down the process of maladaptive remodeling of the left ventricle;
- reduce the risk of damage to target organs (heart, brain, vascular wall, kidneys);
- reduce the risk of developing severe complications (stroke, myocardial infarction);
- prevent the risk of sudden death;
- delay disability.
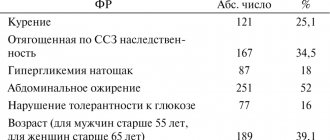
Table Antihypertensive drugs and their interactions with other drug groups of drugs
| Antihypertensive drugs | Interacting drug group | Result of interaction |
| Neurotropic, α2-adrenergic receptor agonists | CNS depressants | Increased depressive effect |
| Tricyclic antidepressants | Reducing the hypotensive effect | |
| NSAIDs | Weakening the hypotensive effect | |
| Neurotropic, β-blockers | Antianginal, nitrates | Increased hypotensive effect |
| Antiarrhythmic drugs (Class III and IV) | Increased cardiodepressive effect, bradycardia with severe hemodynamic effects | |
| Cardiotonic, glycosides | Increased likelihood of AV block and bradycardia | |
| Alcohol, alcohol-containing medications | Increased hypotensive effect | |
| Oral antidiabetic agents | Dysregulation of glucose levels, masking symptoms of hypoglycemia, increased heart rate and blood pressure | |
| Diuretics: thiazides | In type 2 diabetes mellitus hyperglycemia | |
| NSAIDs | Weakening the hypotensive effect | |
| Sleeping pills | The hypotensive effect increases | |
| Ketoconazole, cimetidine, erythromycin | Decreased first-pass metabolism Increased bioavailability of beta blockers | |
| ACE inhibitors | Alcohol, alcohol-containing medications | Increased hypotensive effect |
| Antiplatelet agent – Acetylsalicylic acid in small doses (Aspirin cardio, CardiASK, Thrombo ACC) | Conflicting evidence for reduced benefit on 30-day mortality after myocardial infarction (moderate certainty) | |
| Immunosuppressants, cytostatics, drugs that inhibit bone marrow function | Increase the risk of developing neutropenia and/or fatal agranulocytosis | |
| Potassium-sparing diuretics | Risk of developing hyperkalemia (especially in patients with renal failure) due to a decrease in aldosterone secretion by ACE inhibitors | |
| NSAIDs | Weakening the hypotensive effect | |
| Oral antidiabetic drugs, sulfonylureas | Increased hypoglycemic effect | |
| Antibiotics of the “Tetracycline” group | Reduce the speed and completeness of absorption of ACE inhibitors from the gastrointestinal tract | |
| Estrogen-progestin contraceptives | Weakening the hypotensive effect | |
| Angiotensin receptor type I blockers | Indirect anticoagulants (Warfarin) | Risk of bleeding |
| Antisecretory, reducing the synthesis of hydrochloric acid (omeprazole, cimetidine) | A sharp decrease in blood pressure. Should not be administered to patients due to inhibition of cytochrome P-450 isoenzymes |
To be continued…
Cardioprotective properties of antihypertensive drugs
In modern recommendations for the diagnosis and treatment of arterial hypertension (AH), the main goal of treatment is defined as achieving a maximum reduction in the long-term risk of cardiovascular complications (CVC). This goal can be achieved both by reducing high blood pressure (BP) and by correcting associated risk factors. In all patients with hypertension, blood pressure should be reduced to at least 140/90 mmHg. Art. and lower if well tolerated.
Currently, the main concept of antihypertensive therapy is organ protection, which involves, on the one hand, protecting target organs from damage, and on the other, restoring structural and functional changes that already exist in them.
If we talk about the heart as a target organ, then the consequences of the negative impact of increased blood pressure on it are hypertrophy of the left ventricular (LV) myocardium, the development of fibrosis, various types of remodeling, apoptosis, which ultimately increases the risk of developing cardiovascular disease.
In the early stages of arterial hypertension, the development of myocardial hypertrophy is the result of structural adaptation of the LV to increased pressure load. According to the results of the Framingham study, echocardiographic signs of LV myocardial hypertrophy were noted in 5–49% of women and 8–33% of men aged 30 to 70 years. The degree of LV hypertrophy is determined by hereditary and constitutional factors (gender, age), nutritional factors (excess weight, salt sensitivity), as well as the state of the sympathetic nervous and renin-angiotensin-aldosterone (RAAS) systems. The results of numerous clinical studies have shown that myocardial hypertrophy is an independent risk factor for the development of cardiovascular events, such as angina pectoris, arrhythmia, myocardial infarction and heart failure.
Left ventricular myocardial hypertrophy (LVMH) leads to disruption of the functional properties of the myocardium, and first of all, its diastolic filling is impaired, and then its systolic function. With LVMH, coronary circulation is impaired, which is manifested by a decrease in coronary reserve and insufficient perfusion of the subendocardial layers of the myocardium. In the presence of LVMH, the frequency of ventricular arrhythmias also increases.
The risk of developing coronary insufficiency and ventricular arrhythmias with an increase in the mass of the left ventricular myocardium by 50% increases at least twice.
It was noted that in the group with severe LV hypertrophy, the risk of heart failure increases 5 times. In 30–40% of patients with signs of heart failure, a normal state of systolic function is observed, since in the early stages of hypertrophic remodeling, disturbances in LV diastolic filling and signs of diastolic dysfunction occur primarily. Thus, in patients with hypertension, diastolic dysfunction is an independent factor in the development of heart failure. Speaking about the cardioprotective properties of drugs, we first of all evaluate their effect on LVMH.
A retrospective analysis of clinical studies showed that antihypertensive therapy that reduces LVMH can reduce the risk of cardiovascular events.
What will be the result of a decrease in LV myocardial mass as a result of taking antihypertensive drugs? It has now been proven that regression of LVMH is accompanied by an improvement in systolic function, a decrease in myocardial fibrosis and an improvement in LV diastolic function, an increase in coronary reserve, normalization of the local nervous system and a decrease in arrhythmias, which can ultimately reduce the risk of cardiovascular events and improve the prognosis (Fig. 1) .
Therefore, when we talk about “cardioprotection” in relation to antihypertensive drugs, we assume not only the ability of the drugs to reduce LVMH, but also their ability to influence hard endpoints, such as cardiovascular mortality and other indicators of cardiovascular risk.
Since the triggering factor for the development of LVH is elevated blood pressure, it should be assumed that any antihypertensive drug can cause regression of LVH.
Currently, the question of the effect of various antihypertensive drugs on the processes of hypertrophic remodeling of the LV myocardium remains the focus of attention. In the 90s, a number of reviews of clinical studies were published comparing the effectiveness of various groups of antihypertensive drugs on the degree of regression of LVMH. The authors of the four largest meta-analyses, which compared different groups of drugs in terms of their ability to cause regression of LV hypertrophy, came to a consistent conclusion - drugs that reduce RAAS activity are most effective in reducing LVH - by 11.8–15% from the initial level.
The work of Klingbeil et al. (meta-analysis of 80 double-blind clinical studies) also showed that the greatest degree of reduction in LV myocardial mass index by 13% was noted in patients receiving therapy with angiotensin receptor blockers (ARBs), by 11% - with long-acting calcium antagonists (CA), by 10 % - angiotensin-converting enzyme (ACE) inhibitors, 8% - diuretics, 6% - beta-blockers (BAB) (Fig. 2).
Thus, the leading positions in this list are also occupied by blockers of the renin-angiotensin system - ACE inhibitors and ARBs, which indicates the high role of activation of type 1 angiotensin receptors in the development of LV myocardial hypertrophy.
ACE inhibitors and angiotensin receptor blockers
The cardioprotective properties of ACE inhibitors and ARBs lie not only in their ability to cause regression of LV myocardial hypertrophy due to blockade of components of the circulating and tissue RAAS. Potential cardioprotective effects, such as anti-ischemic and antiarrhythmic effects, are associated with the ability of these drugs to restore impaired endothelial function, stimulate the release of nitric oxide and prostacyclin by reducing the degradation of bradykinin, reduce myocardial oxygen demand due to regression of myocardial hypertrophy, and reduce the activity of the sympatho-adrenal system caused by stimulation of angiotensin II.
We studied the long-term effects of various ACE inhibitors and ARBs on remodeling processes in patients with hypertension. A significant decrease in LVMH parameters was detected during long-term (up to three years) therapy with ACE inhibitors enalapril, ramipril and captopril and the ARBs irbesartan and telmisartan (
). The dynamics of the decrease in 24-hour blood pressure monitoring during the observation period was unidirectional and significantly significant when treated with all drugs. When analyzing the dynamics of the decrease in LV myocardial mass index, a more pronounced, significantly significant decrease in this indicator was noted in the group of patients receiving ARB therapy, which is consistent with the data of a number of other studies.
The anti-ischemic properties of ACE inhibitors, which have been confirmed by a number of clinical studies, deserve special attention. Thus, the HOPE (Heart Outcomes prevention evaluation study) study with ramipril (an ACE inhibitor with high affinity for tissue ACE) included 9297 patients over 55 years of age with a high risk of cardiovascular events. After 4.5 years of observation, a significant reduction in the risk of developing acute myocardial infarction, stroke and coronary events requiring revascularization was noted - that is, those complications that are the usual “companions” of the progressive atherosclerotic process. The results of this study once again confirmed the validity and validity of the concept that the prevention of cardiovascular morbidity and mortality is possible by blocking the RAAS at the tissue level.
A clinical study of the anti-ischemic properties of ACE inhibitors in patients with hypertension in combination with coronary heart disease (CHD) and stable angina pectoris was carried out at our department. Under the influence of treatment with perindopril and enalapril in patients with hypertension in combination with coronary artery disease, stable angina pectoris, good antihypertensive effectiveness was combined with an antianginal effect and positive dynamics of exercise test indicators. In patients receiving perindopril therapy, there was also a decrease in the total duration of episodes of myocardial ischemia (according to the results of Holter ECG monitoring), a decrease in the manifestations of endothelial dysfunction, an improvement in diastolic myocardial function in patients with relaxation disorders, as well as an improvement in local myocardial contractility in the form of a decrease in the number of hypokinetic segments both at rest and at the height of physical activity (under conditions of stress-ECHO-CG).
In recent years, the results of large multicenter clinical trials have become widely available, studying various aspects of cardioprotection of a relatively new class of antihypertensive drugs - angiotensin II receptor blockers. Thus, in the clinical trial LIFE (Losartan Intervention For Endpoint reduction in hypertension), the cardioprotective properties of losartan were assessed in 9193 hypertensive patients with LVMH using ECG amplitude criteria. Patients were divided into treatment groups with losartan or atenolol. In case of insufficient blood pressure control, hydrochlorothiazide was added to therapy. The duration of treatment averaged 4.8 years. There were no differences between the groups in baseline blood pressure and the degree of blood pressure reduction during active treatment. In the group of patients receiving losartan, a more pronounced decrease in quantitative signs of myocardial hypertrophy was noted than in the atenolol group. The risk of developing cardiovascular events was 13% lower in the losartan group (23.8 events per 1000 patients per year) than in the atenolol group (27.9 events per 1000 patients per year). The CV mortality rate in the losartan group was significantly lower.
The randomized, double-blind CATCH (Candesartan Assessment in the Treatment of Cardiac Hypertrophy) study compared the effectiveness of candesartan (8–16 mg/day) and enalapril (10–20 mg/day) in hypertensive patients with LVMH (according to ECHO-CG data). — LV myocardial mass index (LVMI) > 100 g/m2 in women and > 120 g/m2 in men). The duration of observation was 1 year. In both groups, there was a significant decrease in LVMI (10.9 ± 15.5% and 8.4 ± 17.4%, p < 0.001). In the group of patients receiving candesartan, positive dynamics were observed in 36% of cases, in the enalapril group - in 30%.
The effectiveness of other ARBs, in particular valsartan and irbesartan, regarding the possibility of regression of LVMH in patients with hypertension has also been confirmed in a number of long-term clinical studies.
Calcium antagonists
According to a meta-analysis of clinical studies, long-acting calcium antagonists are second only to blockers of the renin-angiotensin system in terms of the degree of reduction in LVMI - they reduce LVMI by an average of 11%. The most studied drug from the group of long-acting AKs is amlodipine. Its cardioprotective properties have been studied in large clinical studies, such as ELVERA, ALLHAT, VALUE, ASCOT, PRESERVE.
The ELVERA study (Effects of amlodipine and lisinopril on Left Ventricular mass) showed a significant significant decrease in LV myocardial mass index after 2 years of treatment with amlodipine in hypertensive patients with LVH, which was accompanied by an improvement in LV diastolic function.
Of particular note is the ALLHAT study (Antihypertensive and Lipid-lowering treatment to prevent heart attack trial) - a randomized, double-blind study in patients with hypertension at high cardiovascular risk of the effectiveness of treatment with lisinopril, amlodipine, doxazosin and chlorthalidone in reducing fatal outcomes of coronary heart disease and non-fatal myocardial infarction. The study included 33,357 patients, of which 9 thousand were treated with amlodipine. The follow-up period was 4.9 years. In the group of patients treated with doxazosin, a significantly higher risk of developing cardiovascular events was noted; therefore, the study of the effectiveness of this drug was suspended. Antihypertensive efficacy in the chlorthalidone and amlodipine treatment groups was relatively similar and was superior to that in the lisinopril treatment group.
The VALUE (Valsartan Antihypertensive Long-term Use Evaluation) study involved 15,245 hypertensive patients with a high risk of cardiovascular disease over the age of 50 years. The duration of treatment averaged 4.2 years. According to the study results, the risk of developing cardiac morbidity and mortality in patients with hypertension was comparable in the amlodipine and valsartan treatment groups. During therapy with amlodipine, a decrease in the risk of heart attacks and strokes was noted.
The ASCOT (Anglo-Scandinavian Cardiac Outcomes Trial) study included 19,257 patients (mean age 63 years). The duration of observation was more than 5 years. The risk of myocardial infarction and fatal coronary diseases was lower in the group of patients receiving amlodipine (4.5%) compared to the group of patients (4.9%) receiving atenolol.
The PRESERVE study (Prospective Randomized Enalapril Study Evaluating Regression of Ventricular Enlargement) found that with a comparable degree of blood pressure reduction in patients receiving a long-acting form of nifedipine for 1 year, the degree of reduction in LV myocardial mass was higher than in patients receiving enalapril .
Beta blockers (BAB)
In terms of their effect on the severity of LVMH and the ability to cause its regression, beta blockers are inferior to other groups of antihypertensive drugs. The average reduction in LVMI is 5%. At the same time, the significance and effectiveness of beta blockers in reducing the risk of cardiovascular complications in cardiac patients is obvious and beyond doubt. This is largely explained by the main mechanism of action of beta blockers, which is caused by a decrease in increased sympathetic tone. The most readily available marker of increased sympathetic activity is a high resting heart rate. According to epidemiological studies, it has been shown that a frequent heart rate in patients with hypertension is an independent risk factor for the development of cardiovascular complications.
A significant reduction in the risk of developing cardiovascular complications and an improved prognosis in cardiac patients while taking various beta blockers have been shown in a number of clinical studies, such as MAPHY (Metoprolol Atherosclerosis Prevention in Hypertensives study), MRC (Medical Research Council study), CIBIS II (Cardiac Insufficiency Bisoprolol Study).
Diuretics
According to a meta-analysis by Klingbeil et al. Thiazide diuretics, as well as beta blockers, are inferior to other groups of drugs in terms of the degree of reduction in patients with hypertension with LVMH - on average, the reduction in LVMI is 5%.
The situation is different with respect to the thiazide-like diuretic indapamide. Experimental studies have shown that indapamide, a diuretic with calcium antagonist properties, reduces LV myocardial mass by affecting cardiomyocyte volume and pericellular fibrosis at the level of protein synthesis. Indapamide in low doses reduces ACE activity in plasma and myocardium, the induction of cardiac ACE mRNA, and plasma aldosterone levels.
Experimental data have been confirmed in clinical practice. According to the LIVE study (Left ventricular hypertrophy: Indapamide Versus Enalapril), during long-term treatment with indapamide 1.5 mg/day, a significant decrease in LV myocardial mass index was noted compared with therapy with enalapril (20 mg/day).
We also studied indapamide in hypertensive patients with LVMH. On average, regression of myocardial hypertrophy by 8.5% was noted during monotherapy with indapamide for 1 year.
Combination therapy
The current priority in the treatment of patients with hypertension is the use of combination antihypertensive therapy, which allows controlling target blood pressure in most patients.
One of the most rational and widely used is the combination of ACE inhibitors and diuretics. Clinical data confirming the possibility of reducing myocardial hypertrophy during combination therapy were noted in the study by De Luca N et al.: according to ECHO-CG, after 12 months, during combination therapy with an ACE inhibitor and a diuretic, a more pronounced decrease in LVMH was noted compared with the treatment group BAB atenolol.
In a study conducted at our department, a combination therapy regimen (perindopril 4–8 mg + indapamide 2.5 mg) in hypertensive patients with LVMH over the course of a year allowed achieving a more pronounced effect in terms of regression of LVMH (decrease in LVMI by 16.6%, p < 0.001) (
).
Data on the cardioprotective effect of the combination of perindopril with indapamide were confirmed by the results of the PICXEL study (Perindopril Indapamide combination in Controlled study Versus Enalapril). The study included 556 hypertensive patients with LVMH. LVMI significantly decreased by 13.6 ± 23.9 g/m2 in patients receiving combination therapy. In patients receiving monotherapy with enalapril, the decrease in this indicator was 3.9 ± 23.9 g/m2 (p < 0.0001).
A reduction in cardiovascular risk as a result of long-term use of combination therapy with perindopril and indapamide in patients with hypertension in combination with diabetes mellitus was demonstrated in the ADVANCE (Action in Diabetes and Vascular Disease) study: the likelihood of cardiovascular events is reduced by 14%, overall mortality by 14 %, cardiovascular mortality - by 18%.
According to the results of the ACCOMPLISH study (Avoiding Cardiovascular events through Combination therapy in Patients Living with Systolic Hypertension), a significant reduction in the relative risk of cardiovascular mortality and complications was noted when taking the combination of “ACE inhibitor benazepril and AA amlodipine” compared with the combination of “ACE inhibitor benazepril with diuretic hydrochlorothiazide" by 20%.
Conclusion
Thus, at present, according to European and Russian recommendations, when choosing antihypertensive therapy tactics in each specific clinical situation, it is necessary to take into account the peculiarities of the action of various antihypertensive drugs, confirmed by the results of clinical studies. Based on the large evidence base regarding the cardioprotective properties of modern antihypertensive drugs in patients with hypertension and LVMH, the drugs of choice are ACE inhibitors, calcium channel antagonists and ARBs; in patients with hypertension with initial signs of diastolic dysfunction - ACE inhibitors; in patients with hypertension in combination with coronary artery disease - ACE inhibitors, ARBs and beta blockers.
T. E. Morozova, Doctor of Medical Sciences, Professor T. B. Andrushchishina MMA named after. I. M. Sechenova, Moscow
For questions regarding literature, please contact the editor.
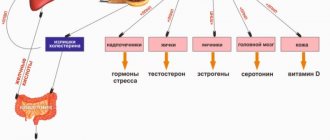
Which antihypertensive drugs protect against depression?
Relevance
Arterial hypertension (AH) is one of the most common risk factors for the development of cardiovascular diseases. Thus, up to 30-40% of the population have hypertension. At the same time, according to some experts, approximately a third of patients with cardiovascular diseases suffer from depression. However, the relationship between taking antihypertensive drugs and depression has not yet been studied, which was the subject of the study being discussed.
Methods
The study was based on Danish registers. Its participants included almost 4 million patients, whose observation lasted from January 2005 to December 2015. Patients taking antidepressants, as well as patients with a diagnosis of depression at the start of the study, were excluded.
The drugs studied were renin-angiotensin aldosterone system blockers, calcium channel blockers, beta-blockers and diuretics.
The outcome analyzed was a psychiatrist's diagnosis of depressive disorder.
results
Treatment with renin-angiotensin-aldosterone system blockers reduced the risk of depression [hazard ratio (RR) 0.97; 95% confidence interval (CI) 0.96-0.99; p<0.001], calcium channel blockers (RR 0.97; 95% CI 0.95-0.98; p<0.001), beta-blockers (RR 0.9; 95% CI 0.89-0.91; p<0.001), but not diuretics (RR 0.99; 95% CI 0.98-1.00; p=0.079).
Drugs that have been found to reduce the risk of depression include:
- from blockers of the renin-angiotensin aldosterone system: enalapril and ramipril;
- calcium channel blockers: amlodipine, verapamil, as well as combinations with verapamil;
- from beta-blockers: propranolol, atenolol, bisoprolol and carvedilol.
Conclusion
Thus, this study identified classes, as well as specific antihypertensive drugs, the use of which is accompanied by a reduction in the risk of depression in patients with hypertension.
The study authors suggest that the findings could be taken into account when prescribing antihypertensive therapy to patients suffering from depression or having a history of depressive disorder. However, we would like to remind you that this study was only an analysis of registers, which means that all hypotheses generated with its help must be tested in specially designed prospective randomized studies.
Source:
Kessing LV, et al. Hypertension. 2021. Doi: 10.1161/HYPERTENSIONAHA.120.15605.