Polycythemia vera
(IP) is a clonal myeloproliferative disease of a chronic nature with a relatively benign course, affecting hematopoietic stem cells and accompanied by the proliferation of three hematopoietic lineages. It is characterized by an increase in the number of red blood cells, an increase in the concentration of hemoglobin, blood cells (leukocytes, erythrocytes, platelets) and total blood volume.
Polycythemia vera is also known as Vaquez's disease, true, or red, erythremia. Belongs to orphan (rare) diseases. It mainly affects people over 60 years of age, more often men. In young people, the disease is less common but has a more unfavorable course.
According to ICD-11, IP is assigned code 2A20.4.
Causes
The exact causes of the disease are still unknown. Scientists suggest that hereditary predisposition, exposure to ionizing radiation and toxic substances play a significant role in the development of pathological changes.
In 20-30% of patients with erythremia, chromosomal abnormalities are detected ( https://cyberleninka.ru/article/n/klinicheskie-rekomendatsii-po-diagnostike-i-terapii-ph-negativnyh-mieloproliferativnyh-zabolevaniy-istinnaya-politsitemiya-1/viewer ).
The likelihood of developing erythremia increases in funeral home employees who embalm bodies, in people who are forced to frequently come into contact with gasoline and other petroleum products, and in those exposed to low doses of radiation. In people who survived the atomic bombing of Nagasaki and Hiroshima, a high risk of developing IP was not observed.
Materials and methods
The study included 81 patients who applied to the outpatient department of the Federal State Budgetary Institution Hematology Research Center of the Ministry of Health of the Russian Federation from 2014 to October 2015. The group consisted of 50 patients with overt IP and 31 patients with latent IP. The diagnosis was established in accordance with the WHO classification criteria of 2008. In the analyzed groups of patients, the gender distribution was statistically comparable. Patients with overt IP are slightly older than those with latent IP: median age 56 and 44 years, respectively.
Symptoms of the disease
Clinical manifestations of IP are divided into 2 groups:
- Plethoric (“plethora” - plethora) syndrome - the mass of red blood cells increases, due to which:
- headaches and dizziness occur;
- pressure increases;
- the skin and mucous membranes acquire a bluish or red-cherry tint;
- disturbing skin itching;
- the conjunctiva turns red;
- vision deteriorates, spots appear before the eyes;
- erythromelalgia develops - small vessels periodically dilate, which provokes redness of the fingers and toes, unbearable burning pain and burning;
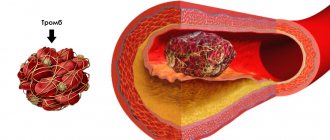
- thrombosis and cerebrovascular insufficiency occur;
- angina attacks are observed.
2. Myeloproliferative syndrome is caused by hyperplasia of three hematopoietic lineages: erythroid, granulocytic, megakaryocyte
With polycythemia vera, myeloid metaplasia of the spleen and splenomegaly often develop (the size of the spleen increases). The most common complications are thrombosis (occurring in 39% of patients), thromboembolism and bleeding (gingival, nasal, gastrointestinal, menorrhagia).
The risk of transformation of polycythemia vera into acute myeloid leukemia is 5%, and into myelofibrosis - less than 10% ( https://cyberleninka.ru/article/n/istinnaya-politsitemiya-sovremennye-predstavleniya-o-pathogeneze-diagnostike-lechenii/viewer ) .
With polycythemia vera symptoms
depend on the stage:
- Stage I (asymptomatic). The main signs (plethora, erythrocytosis, skin hyperemia) are moderate, the number of leukocytes and platelets, the size of the spleen is normal, there are no vascular complications or manifestations of fibrosis. Blood pressure increases and blood circulation is disrupted. Duration – 5 years or more.
- Stage IIA (erythraemic). There is no myeloid metaplasia of the spleen. Skin hyperemia, hepatosplenomegaly, and scleral injection are evident. A general blood test shows thrombocytosis, erythrocytosis, neutrophilia, and bone marrow examination shows focal myelofibrosis, total three-line hyperplasia, and often reticulin fibrosis. Thromboembolic complications are common.
- Stage IIB (erythraemic). Myeloid metaplasia is present. Hepatosplenomegaly develops - the liver and spleen simultaneously increase in size. A general blood test reveals leukocytosis, shifted to myelocytes, and a possible decrease in the number of platelets and red blood cells. When diagnosing bone marrow, focal myelofibrosis and panmyelosis are noticeable.
- Stage III (posterythremic, anemic) – terminal. The concentration of blood cells and hemoglobin sharply decreases. Symptoms of tumor intoxication become noticeable, and hemorrhagic complications occur. Myelofibrosis develops and blast crisis occurs.
How do we treat polycythemia?
With polycythemia, damage to the bone marrow occurs: too many red blood cells are produced (hemoglobin levels increase greatly), platelets, leukocytes, the amount of blood in the body increases significantly, its viscosity increases, blood flow becomes slower, small capillaries become clogged.
All this significantly increases the risk of blood clots. Our doctors effectively diagnose and treat polycythemia. To identify and treat pathologies, the clinic is equipped with premium equipment.
You can find out how much diagnosis and treatment of polycythemia costs in the price list on our website. Our prices are favorable for patients.
Diagnosis of the disease
At the initial appointment, the doctor listens to complaints and examines the medical history. He also conducts a physical examination, during which he examines the skin and mucous membranes, assessing their pigmentation, the presence of hemorrhages, edema, and trophic disorders.
Then the specialist refers the patient for laboratory and instrumental diagnostics, which may include:
* clinical, biochemical and molecular genetic blood analysis;
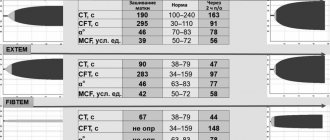
* coagulogram;
* study of iron metabolism;
* blood test for HIV infection and hepatitis;
* trephine biopsy of the bone marrow followed by cytological, histological and histochemical analysis of the biopsy;
* Dopplerography of cerebral arteries;
* Ultrasound of the abdominal organs.
The main marker for diagnosis is the Jak-2 gene mutation, which occurs in 95% of patients. Also, in patients with PV, the level of erythropoietin should be reduced or at the lower limit of normal and never elevated, which is initially used for differential diagnosis.
Once diagnosis is made, treatment for polycythemia may include:
- bloodletting, which reduces the number of red blood cells and hemoglobin levels. It is this ancient method that copes well with the main medical goal: normalizing the amount of blood. The procedure is performed at certain intervals to achieve the desired results. Hematologists sometimes replace bloodletting with erythrocytopheresis (plasmapheresis). Also, instead of bloodletting, in some cases chemotherapy is prescribed.
- taking medications to prevent the bone marrow from producing too many red blood cells.
- the use of antiplatelet agents, which reduce blood viscosity and prevent the formation of blood clots.
- intramuscular injection of interferon.
- use of antihistamines, corticosteroid hormones.
The treatment plan is always personalized by the doctor at our medical center, but phlebotomy therapy is the first choice because it can reduce symptoms and prevent most complications of the disease. The regime of work, nutrition, and rest, which is recommended by a specialist, is very important.
Get diagnosed and treated for polycythemia with our hematologists
Diagnosis and treatment of polycythemia are aimed at reducing the risk of complications and preventing symptoms of the disease, which is still considered incurable. According to patient reviews, our hematologists have helped improve the quality of life of many patients.
Our price for diagnosing and treating polycythemia is lower than in most clinics in the city. We are equipped with expert level equipment. Our hematologists use modern approaches to therapy, which allow us to achieve good results and relieve patients from most of the negative manifestations of the disease and the risk of severe complications. If effective treatment is carried out in a timely manner, there is a real chance to extend the patient’s life by decades.
Indications for MSEC
A patient with erythremia is referred to undergo a medical and social expert commission (MSEC) by his attending physician, who is guided by the presence of a certain number of indications in a particular patient. These include:
- Stage II of the disease when there is a need to transfer the patient to a position of lower qualifications, another profession, or the need to reduce the volume of activities performed;
- terminal stage of erythremia;
- the course of the disease with vascular complications leading to significant dysfunction of the cardiovascular system.
results
Between the groups of patients with latent and overt PV, differences in the number of erythrocytes are obvious - 5.37 1012/l (4.1-6.5 1012/l) versus 6.94 1012/l (5.4-8.8 1012/l), hemoglobin concentration - 148 g/l (100-167 g/l) versus 178 g/l (136-247 g/l) and hematocrit - 45% (30-52%) versus 53% (42 -70%). The median platelet count was higher in the group of patients with latent PV compared to overt PV: median 644·109/L (179–1978·109/L) versus 636·109/L (137–2437·109/L). There were no differences in the number of leukocytes in the compared groups. Molecular genetic research (qualitative analysis) was performed in all patients. All patients are carriers of the V617 °F mutation of the JAK2
.
Determination of the JAK2V617 °F allelic load (quantitative analysis) was performed in 29 patients with latent IP and 37 with overt IP. JAK2
allelic load was significantly higher in the group of patients with overt PV compared to latent PV: median 14% (3–57%) and 55.5% (24–86%), respectively. The compared groups of patients differed in the incidence of thrombosis in history/at the time of diagnosis. In the case of latent PV, thrombosis was detected in 12 (38%) patients compared to 10 (16%) in advanced PV. In the case of latent PV, predominantly venous thrombosis was detected; thrombosis of the abdominal vessels was often diagnosed. Arterial thrombosis was detected only in 4 observations. Clinical and laboratory characteristics of patients are presented in Table. 1.
Table 1. Clinical and laboratory characteristics of patients with latent IP and full-blown IP Note.
MI - myocardial infarction; ACVA is an acute cerebrovascular accident. The morphological characteristics of BM trephine biopsy in patients with latent PV did not differ from those in patients with overt PV.
Changes in working conditions
With this disease, young patients suffering from stages I and IIA erythremia in remission are considered to be able to work. Moreover, their condition should not be complicated by vascular pathologies.
For patients with polycythemia there are certain contraindications and the following working conditions are recommended:
- Stage I. Activities that require excessive physical effort or psycho-emotional stress are prohibited. Work in an unfavorable microclimate and interaction with hemotoxic substances are also contraindicated.
- Stage II. Work associated with a forced uncomfortable body position, moderate physical activity and neuropsychic stress, vibration exposure, exposure to heights, changes in temperature, pressure, etc. is not recommended.
- Stage III does not allow patients to work under normal production conditions for a healthy person.
Symptoms of polycythemia vera
Determination of disability
When conducting a commission to determine the degree of disability, medical experts are guided by the following criteria. A patient is not entitled to disability in case of a latent, indolent (sluggish) form of erythremia without symptoms of progression with unexpressed dysfunction of organs.
Group 3 is assigned to Vaquez disease with moderately manifested blood and immune dysfunctions during the treatment provided to the patient. Group 2 is provided for severe deviations in the activity of the circulatory and immune systems during the therapy.
Group 1 is assigned to the terminal stage, accompanied by significant impairments in the functioning of the circulatory and immune systems, against the background of developing acute leukemia. The category “disabled child” is provided for polycythemia with blood and immune dysfunction, starting from a moderate degree and further on the background of treatment.