- Home /
- Blog /
- Treatment
January 16, 2020
“A blood clot came off” is a mysterious phrase that leads to sad consequences. How many show business stars, of different ages and habits, have passed away for this reason. Why does the disease leave little chance of salvation? Is it possible to warn her?
We’ll talk about this in our article: where do blood clots appear in blood vessels, what to do for prevention and how to treat.
What is a thrombus in blood vessels
A thrombus is a blood clot that consists of red blood cells stuck together - platelets and the protein fibrin. Under normal conditions, these elements of the body are responsible for blood clotting and perform useful functions: stopping bleeding. But when a vessel is damaged, a blood clot forms in that location.
A blood clot is dangerous because it prevents blood from flowing freely through the vessels. Over time, it can break off and travel to the heart, lungs, brain and cut off circulation to vital organs. The result is heart attack, stroke, gangrene, paralysis and death.
A blood clot does not form just like that. Several factors decide: a person’s lifestyle, diseases.
Let's talk about those who are at risk of developing blood clots in their vessels a little later.
The Last Fireworks: What Happens to the Body When We Die
As a patient approaches death, changes occur in his body. They concern breathing, blood circulation, consciousness. We explain in detail what happens: if we understand death, perhaps we will be less afraid of it.
Author: Jacob Zimmank
The author of the article is a former employee of the palliative care service, which supervises dying people at home. He was amazed at how calmly many people faced their own death.
When does dying begin? At what point does a person begin his path to death?
Dying begins long before we are born. It is laid in the womb, in a cluster of cells from which the unborn child is formed. Some cells are redundant and need to make room for new ones. This is the only way the child’s organs can appear. It is due to this that there are only two kidneys, and only ten fingers on the hand. The genome of each cell already contains programs that act as a kind of “catapult”. It turns on at the moment when the cell becomes unnecessary or dangerous for the body. In this case, the cell voluntarily destroys itself.
Becoming a person is a process that involves both life and death. According to palliative medicine doctor Jean-Domenico Borasio, death is “a necessary condition so that we can, in principle, be born as viable organisms.”
“What we know for certain is that a person does not die suddenly, overnight” - Jean-Domenico Borasio, palliative care doctor
Death is omnipresent - but once we are born, we forget about it. And, if all is well, then death will appear in our lives again only after a few decades. Often this will be a condition that cannot be cured: cancer, heart disease, or kidney disease that means they can no longer cleanse the blood. And then the process of dying begins.
“What we know for certain is that a person does not die suddenly, overnight. The organs of the human body stop functioning gradually, not all at the same time, and then at some point their work stops,” says Dr. Borasio. As a result of the chain reaction, the liver, kidneys, lungs and heart stop working.
There are a variety of diseases, but at the end of life everything always follows the same pattern: the heart stops beating, breathing stops and, last of all, consciousness fades away. At the same time, it is very difficult to separate the work of the heart and brain. If the heart stops pumping oxygenated blood, brain cells begin to die within seconds. And after a few minutes, brain death occurs: at this moment the EEG will show a straight line instead of the usual curves and teeth. The reflexes that control the deep parts of the brain responsible for breathing, swallowing and consciousness also stop working. Thus, when the heart stops, the brain also stops working.
It also happens the other way around. The brain contains centers that regulate all vital functions: blood pressure, heart function, breathing. If these centers are damaged, breathing will stop and the heart rhythm will be disrupted. Often this damage occurs when intracranial pressure rises sharply as a result of a car accident or accident. The bones of the skull are hard, so with a strong blow, the soft tissue of the brain is squeezed into the only natural opening in the skull - the foramen magnum. Through it, the cranial cavity communicates with the spinal canal (the spinal cord passes into the brain stem). If the brain stem is pinched or damaged, the person dies.
There are no clear signs, but there are general patterns
Dying people live the last years, months and days of their lives in different ways. “The dying process is very individual,” says Lukas Radbruch, president of the German Society for Palliative Medicine and professor at the University Hospital Bonn. It often lasts for months or even years. Doctors divide dying into three stages: at the beginning comes the “terminal” stage, which lasts one to two years. At this time, the functioning of individual internal organs gradually decreases, and the dying person increasingly experiences fatigue. This is followed by the “pre-final” stage, which can last several weeks or months. At this time, symptoms such as shortness of breath and pain appear. And finally, the “final” stage - the last days. The patient stops eating and drinking and slowly fades away. “It is important to remember that this division of dying into stages is nothing more than a convention,” notes Radbruch. It is important for providing treatment and care, but does not provide an accurate picture and “does not help determine when the patient will die.”
“It used to be believed that the approach of death was indicated by pale skin in the nasolabial triangle,” says Radbruch. But this is also an unreliable sign. Currently, research that allows us to accurately determine the time of death is at an early stage. Some scientists are testing blood samples for markers that can be used to calculate remaining life expectancy. Radbruch says the best thing to do is ask the attending physician: Would she be surprised if she learned that the patient died that night or next weekend? If the doctor says that she is not surprised, then it is time to prepare for death.
Part 2. Death rattle
Although dying is a highly individual process, there are certain physical changes that are common to most patients (Palliative Care Review: Plonk & Arnold, 2005). As we approach death, there are more and more similar features, although the cause of death may be different. The dying are exhausted, have difficulty breathing and experience pain. Breathing changes: at first it becomes shallow, then intermittent, but after a while the dying person can again take a deep breath.
Doctors suggest that by this time the centers of the brain responsible for breathing have already been affected. They react late to the presence of carbon dioxide in the blood, allowing it to accumulate in large quantities. In some cases, breathing noises occur, one of which used to be called the “death rattle.” Due to the inability to expectorate and clear the throat, secretions accumulate in the pharynx and bronchi, which affects the passage of air flow during breathing.
The death rattle is often a terrible sound, but there is no evidence that the dying person is suffering at this moment. The same applies to an increase in the level of carbon dioxide in the blood - it is assumed that this has a rather calming and soporific effect. The death rattle (as the name suggests) indicates that death is imminent (American Journal of Hospice and Palliative Medicine: Morita et al, 1998). With very little time left, wheezing may become uncontrollable.
In addition, in the last days and hours before death, changes in blood circulation are observed. The body tries to deliver the small amount of oxygen that the heart is still able to pump through the blood to vital organs. “The pulse weakens and is often barely palpable, the hands become cold and the lips may turn blue,” explains Lukas Radbruch. “It’s a stress reaction.” In some cases, the heart begins to beat faster, the blood pressure drops, and a slight fever may even appear.
When consciousness fades
Radbruch says: “Someone remains conscious until his last breath. Another may experience anxiety and even hallucinations. And the third one just quietly fades away.”
There are enough reasons for such changes. On the one hand, due to uneven flow of blood and oxygen, brain metabolism is disrupted. On the other hand, some organs stop working, and because of this, toxic substances accumulate in the blood. For example, urea, which is excreted through the kidneys, can damage nerve cells in high concentrations. (But the dying person does not suffer from this either. Oblivion caused by a high concentration of urea in the blood is similar to anesthesia - it does not hurt the person, it is even pleasant.)
In addition to urea, ketone bodies accumulate in the blood of a dying person in large quantities, which also affect a person’s consciousness. They are produced from fat and, in conditions of energy deficiency, are used by the body as a substitute for glucose, which is necessary to nourish the brain and muscles. This is exactly what happens when dying: a person stops eating, but does not experience hunger (JAMA: McCann et al., 1994).
When dying, many patients quietly fade away or, on the contrary, become excited and whisper something excitedly. It may seem that they have already left this world, but despite this, “we must treat the dying as if they understood everything,” emphasizes Lukas Radbruch. “We don’t know exactly how much they can take in.”
Many patients continued to perceive what was happening even after cardiac arrest. This is evidenced by the results of a large study. Scientists interviewed 140 people from the UK, Austria and the US who had experienced cardiac arrest. Nine percent of those surveyed reported having had a near-death experience such as feeling fear, seeing a light or seeing family members.
Two of the respondents remembered the process of their own resuscitation. One of them talked about watching the doctors’ actions from above, from the corner of the room. He remembers that the doctors turned on the defibrillator and tried to “start” the heart, make it beat at the right rhythm again. And this coincided with what was happening in reality. It is interesting that the patient regained consciousness only a few minutes after cardiac arrest.
Last fireworks
When the heart stops and stops supplying the brain with oxygen, nerve cells do not die immediately. On the contrary, their activity increases sharply. This was reported by scientists who studied the electrical activity of the brain in laboratory rats (the rat’s brain is in many ways similar to the human brain). A few minutes after the rodents' hearts stopped beating, a burst of electrical activity could be observed—exceptionally strong. “This may explain why the memories of patients who have experienced clinical death are so real and accurate,” writes one of the study authors, anesthesiologist George Mashour of the University of Michigan Medical School.
When the heart stops, a real fireworks display occurs in the brain. Nerve cells release enormous amounts of norepinephrine, which affects the frontal lobes of the brain and sharpens attention. There is also a release of serotonin, so hallucinations and mystical insights are possible. And at the very last moment, dopamine arrives from the midbrain. It is responsible for the feeling of satisfaction, gives a feeling of warmth and joy. Perhaps even happiness.
The original interview is on ZEIT ONLINE.
We thank Vera Foundation volunteer Veniamin Sapozhnikov for translating this article.
How to support hospice patients?
It is very easy to support hospice patients. You can sign up for monthly donations (by checking the box next to “I want to donate monthly”) or make a one-time donation :
Thank you always.
Share
Tweet
Share
Share
SIMILAR
How do blood clots occur in blood vessels?
In a healthy body, blood circulates freely between organs, delivering nutrients and oxygen. A blood clot appears when the wall of a vessel is damaged, for example due to excess sugar in the blood. The fabric becomes rough. Platelets cling to irregularities and plaques form.
At this point, the vessel narrows and the speed of blood flow changes. Turbulence arises - a vortex, chaotic flow of blood. Platelets and fibrins stick together to form a clot.
Where does it come from?
There are a lot of factors that provoke the appearance of thrombosis.
Firstly, this is damage to the vascular walls. It can occur due to injury, after surgery, infection, heavy lifting, or after childbirth.
Secondly, a blood clotting disorder. This factor also has its reasons, and most often they are associated with metabolism or hormonal imbalance. The disorder may also be associated with a genetic pathology – thrombophilia.
Thirdly, blood stagnation may be the cause. They appear with prolonged physical inactivity. For example, during sedentary work, treatment of fractures, paralysis, long journeys.
And besides, thrombosis is provoked by certain diseases. These are tumors, stroke, heart failure, systemic vasculitis, atherosclerosis, obesity. The presence of these diseases and conditions increases the likelihood of thrombosis.
What does “blood clot come off” mean?
Blood clots occur in blood vessels, veins, arteries or the atrium. After some time, the clot or part of it breaks off and is carried by the blood stream from the site of formation to the brain, lung or heart.
A detached blood clot causes:
- pulmonary thromboembolism;
- stroke;
- heart attack.
Venous thromboembolism is when a blood clot forms in the deep veins of the lower extremities and travels to the lungs. There it blocks blood vessels and blocks the flow of blood to a certain area of the organ, thereby posing a threat to human life.
During a stroke, a blood clot breaks off and is carried by the blood to the brain. The larger the clot, the larger the area of brain damage.
During a heart attack, a blood clot blocks a coronary artery and the heart does not receive oxygen.
A detached blood clot leads to death or disability.
Possible consequences
They depend on where the blood clot clogged the vessel:
- if in the brain, then a stroke occurs;
- if in the coronary arteries - myocardial infarction;
- if in the intestines, then - necrosis, peritonitis of this organ;
- if in the legs, then gangrene is possible.
Stagnant blood is a favorable environment for microorganisms. An infected embolus can cause sepsis.
Who's at risk
Please note if you:
- over 40 years old;
- are obese;
- varicose veins;
- coronary heart disease;
- oncology;
- lead a sedentary lifestyle;
- experienced lower extremity injuries;
- often travel long distances;
- suffered a stroke, lung disease;
- are taking oral contraceptives or hormone therapy
there is a high probability of thrombus formation in the vessels. The risk of thrombosis during pregnancy increases significantly, because the mother’s body changes greatly, it begins to work for two, and the level of female hormones increases.
Who is predisposed to pathology?
Experts have identified conditions that affect susceptibility to pathogenic thrombus formation. The risk group includes:
- Men over 40 years old
. The functioning of the cardiovascular system worsens and blood clotting increases. - Women over 50 years old
. Before menopause, women's blood is regularly renewed. - Overweight people
. Cholesterol, which is deposited on the walls of capillaries, becomes a threat. - Alcohol abusers
. Excess alcohol in the blood removes water from the body and causes platelets to stick together. - People with low physical activity
. Exercising prevents the formation of stagnation in the blood. - Pregnant women and new mothers
. During this period, hormones are produced that help increase blood clotting. - For the same reason - taking hormonal contraceptives.
- People after surgery
. Blood clots often form after operations on the heart and joints. - Lovers of coffee and strong tea
. Caffeine constricts blood vessels, which leads to poor blood flow. - Smoking
. Nicotine also leads to a decrease in the lumen of blood vessels.
The appearance of thrombosis is associated with diagnoses of oncology and inflammation, varicose veins and diabetes, atherosclerosis and heart disease.
How to recognize
- swelling of the legs;
- venous networks;
- causeless dry cough, or with blood;
- heart rhythm is disturbed;
- chest pain;
- redness with changes in body temperature in this place;
- fatigue.
Blood clots in blood vessels are dangerous because they may not show signs, so death occurs suddenly and quickly, so that doctors do not have time to intervene. But if you have a predisposition, then timely examination will help save your life.
Where to go for treatment
— Who usually suffers from thrombophilia?
— Thrombophilia is a separate condition that is associated with a blood clotting disorder. It can be acquired or congenital - and there are quite a few such cases. These people have an increased risk of thrombosis, mainly venous, due to genetic abnormalities.
— In what cases should you see a doctor and which one?
— If we talk about varicose veins, then the following reasons will be the reason to consult a doctor:
- dilated bulging veins on the legs are visible,
- there are spider veins. Spider veins are mainly a cosmetic problem, but it is better to see a vascular surgeon or phlebologist.
- if your legs swell in the evening,
- for cramps, severe leg fatigue.
All these are planned moments.
There are emergency situations associated with thrombosis, if a person notices that one leg is suddenly swollen, if there is bursting pain in the leg, some kind of change in the skin - redness, blueness. In this case, acute thrombosis can be suspected, and this is already a reason to call an ambulance and emergency hospitalization in the department of cardiovascular surgery. This is a dangerous situation - thrombosis.
How to treat blood clots in blood vessels
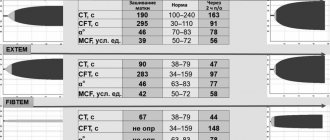
Any treatment begins with visiting a doctor. He will prescribe a treatment regimen based on the reasons and after examination: ultrasound of the lower extremities, ECG, coagulograms - examines the clotting ability of the blood.
If you have atrial fibrillation, that is, an abnormal heart rhythm, your doctor will prescribe coagulants—blood thinners—and cardiac aspirin, which prevents platelets from sticking together.
In the case of blood clots in the deep veins of the lower extremities, it is proposed to be treated with a laser or remove damaged veins through punctures.
Surgery under general anesthesia is possible if the situation is critical.
Prevention in the sanatorium
To avoid blood clots in the vessels, take time for examination. You can go through it at the Mashuk Aqua-Term sanatorium complex during your vacation, combining relaxation with healing your body. Here you will find special programs to prevent blood clots and prevent strokes and heart attacks.
We advise you to be attentive to your health, undergo annual examinations and consult a doctor.
Subscribe to our blog to learn even more about how to stay healthy - treatment methods, disease prevention, as well as relaxation in the Caucasian Mineral Waters.
January 16, 2021 | vessels