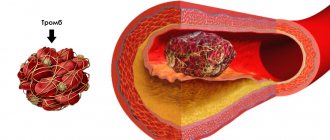
According to the World Health Organization, in most developed countries, deep vein thrombosis and pulmonary embolism have become one of the leading causes of mortality. Millions of people around the world die every year from acute blockage (embolism) of a blood vessel by a thrombus. The danger of thrombosis is that a clot can reach a size comparable to the diameter of a venous vessel and completely block the blood flow in it. Or, if it ruptures, the clot can travel with the blood into the vessels of the lungs and lead to pulmonary thromboembolism. Often with fatal outcome.
Related article Catch it if you can. How to detect and destroy a blood clot
“A blood clot has broken off,” they sometimes say in this case about the cause of death. Even fairly young people often die from detached blood clots. According to specialists from the Moscow State Medical and Dental University named after A. I. Evdokimov, more than 90% of deaths from pulmonary embolism occur in patients who were not diagnosed with embolism and who did not receive treatment.
What causes blood clots?
Thrombi, in the form of blood clots, form in blood vessels in response to damage to the vascular wall, slowing of blood flow and changes in blood composition. “Thrombosis does not occur out of nowhere; there must be some prerequisites. This is facilitated by the presence of varicose veins in the lower extremities. If it is, you should pay attention to compactions that may appear in the veins,” says phlebologist, surgeon Fedor Shpachenko .
According to the phlebologist, compactions may indicate that blood clots have already formed in the veins. “Often, these blood clots may not occur in the superficial veins that we see, but in deep veins, and it is impossible to visualize them without special research methods,” warns Shpachenko.
Causes of blood clot separation
The thrombus can be parietal, or it can be floating. If a blood clot is located near a cholesterol plaque, it is less likely to come off than a floating blood clot. The latter “sits” on a thin leg, which has a weak attachment to the vascular wall. It is floating blood clots that most often lead to the development of pulmonary embolism and strokes.
Also, wandering blood clots may be present in the body, which pose a serious threat to life.
A blood clot can break off as a result of the following influences:
- The blood flow accelerates greatly.
- A thrombus has formed in a wide vessel.
- The stem of the thrombus is weak.
After breaking off, the thrombus begins traveling with the bloodstream along the vascular bed. At this time, it often breaks up into small fractions. Once in a vessel that does not exceed its size, the thrombus clogs it. This entails stopping blood flow and disrupting the nutrition of the limb or organ. This pathological condition is called occlusion.
Who is at risk?
Those who are most likely to develop thrombosis are people who are obese and have varicose veins, women who take oral contraceptives, and those who take many long flights. But a high risk of blood clots occurs when all these factors are combined.
“Patients with obesity and varicose veins are at risk. As for medications, in particular oral contraceptives, now most of them are well balanced and we rarely see the development of thrombosis and thromboembolism in women taking these drugs. People with a sedentary lifestyle, impaired hemostasis, namely blood clotting disorders, also fall into this group. If the patient has all these provoking factors, then the risk of developing thrombosis increases. Age also makes it worse. Over the years, the vessels lose elasticity and become brittle, plus a number of concomitant diseases cause swelling of the lower extremities,” says Shpachenko.
How do blood clots occur?
If a blood clot has formed on the wall of an artery, its appearance can be described in the following stages:
- Some process damages the artery wall.
- The body notices the violation and begins to build protection against blood loss, forming a large number of special blood cells - platelets, which, attaching to the damaged area, form a kind of patch.
- In case of coagulation disorders or changes in the hematopoietic system, platelet formation does not stop on time and continues longer than expected. This causes too much growth to form on the wall. Or platelets, which are in small quantities in the blood, floating past in the bloodstream, stick to the resulting accumulation.
The causes of damage to the walls of blood vessels can be:
- mechanical disruption of the structure due to injury;
- infectious lesion;
- high levels of glucose molecules in the blood;
- immune system dysfunction.
If there are no factors that contribute to the formation of blood clots, any injury or other damage will not lead to a large accumulation of blood cells. Under the layer of platelets, the artery wall will heal and recover, and the crust will resolve over time.
There are several stages of thrombus formation:
- disruption of the structure of the inner surface of the artery;
- activation of blood clotting factors;
- platelet adhesion at the site of injury;
- the appearance of substances that trigger a chain of reactions that form fibrin threads, which contribute to thrombus formation;
- a kind of network of fibrin threads is formed, into which blood cells enter, creating a large clot;
- Over time, the clot thickens, forming a thrombus.
When a blood clot breaks off under the influence of any factors, it begins to move through the bloodstream. Once it hits the nearest bottleneck, the blood flow will be blocked. If a similar situation happens outside a medical facility, it is impossible to save the person.
How to diagnose thrombosis at an early stage?
Thrombosis at an early stage can be detected with timely diagnosis of the veins of the lower extremities. To confirm or refute the diagnosis, phlebologists often recommend laboratory and ultrasound duplex scanning (USD) of the veins. This diagnostic method allows you to see the walls and lumen of the veins, the presence of a blood clot in them, its size, and even roughly judge how long ago the process is. You can also do angiography: a contrast study of blood vessels. And the predisposition to the appearance of blood clots can be identified using a coagulogram: a comprehensive analysis of blood clotting indicators.
If a blood clot comes off, what should you do?
If a person has a blood clot, then you cannot hesitate to call an ambulance. Moreover, even a doctor will not be able to make an accurate diagnosis without special equipment. Therefore, the victim must be urgently hospitalized.
There can be two treatment regimens for thrombosis: either the patient is prescribed medication correction or he is referred for surgery.
Drug therapy includes:
- Prescription of anticoagulants. These drugs help thin the blood (Heparin, Warfarin).
- Course treatment with statins.
- Prescription of fibrinolytics.
- Prescribing thrombolytics, which are necessary to dissolve the blood clot.
If the problem cannot be solved with the help of medications, or the person develops complications of thrombosis, he is indicated for an operation called thrombectomy. It is also possible to install special vena cava filters that will “catch” blood clots, preventing them from clogging vital vessels.
How to determine deep vein thrombosis?
Thrombosis often occurs asymptomatically or with mild symptoms. The nature of patient complaints may vary depending on the location of the blood clot, the duration of the disease and the nature of the lesion. The main symptom of deep vein thrombosis is pain in the leg, namely in the calf muscle. Swelling may also be a concern. When a blood clot forms in the deep veins of the lower extremities, the skin may take on a reddish or blue tint.
Article on the topic
Dissolve the clot. What foods improve blood quality
“Signs of thrombosis can manifest themselves as swelling and pain in the lower extremities, and the location of this pain can be very diverse. Sometimes you can’t guess what the pain is due to: either osteochondrosis, or blood clots, or other diseases. Therefore, if your legs swell, or there are varicose veins in your legs, then you should pay attention to the possible development of blood clots,” says Shpachenko. An ultrasound duplex scan or angiography will help you understand the exact picture.
Antithrombotic nutrition
To prevent thrombosis, the diet should be designed in such a way as to normalize the balance of lipids and carbohydrates, adjust the amount of salt and introduce bioflavonoids into the daily diet, which improve metabolism, strengthen and restore the walls of blood vessels.
Recommended products: lean meat, fatty sea fish, vegetable oil, fresh low-fat milk, low-fat fermented milk products, cereals (except wheat and pearl barley), durum pasta, whole grain bran bread, vegetables (except potatoes and sugar beets), legumes, fruits (except bananas and grapes), nuts, freshly squeezed juices, dark chocolate.
Products that need to be reduced to a minimum: fatty meat and offal, hard and soft fatty cheeses, full-fat dairy products, butter and combined fats, smoked meats, sausages, dried and salted fish, chips, fast food, alcohol, lemonade, candy , milk chocolate, baked goods, potatoes, fatty sauces.
The daily amount of salt should be no more than 6 grams. 1/3 animal protein should account for at least 2/3 vegetable protein and fiber. To prevent thrombosis, you need to add vitamins: C, E, A (retinol), B3 (rutin), bioflavonoids (quercetin, hesperidin).
Be sure to follow the drinking regime: the daily norm for an adult is from 1.5 to 2.5 liters of water per day (soups, tea and coffee are not included here). These simple tips are relevant not only for patients with thrombosis, but also for people with risk factors for this disease. Always be hematologically healthy, and if you identify symptoms of thrombosis, do not self-medicate - contact an experienced specialist, a hematologist-hemostasiologist!
How is pulmonary embolism diagnosed?
As a result of pulmonary embolism, cardiac function, pulmonary blood flow and gas exchange are disrupted. This condition is accompanied by characteristic symptoms, primarily a rapid heartbeat. There may also be a stabbing pain in the chest that gets worse while breathing. Patients may experience severe shortness of breath, and the respiratory rate may increase to 30-40 per minute. In addition, cyanosis or pallor of the skin, decreased blood pressure, cough, and hemoptysis may be observed.
“In the case of pulmonary embolism, difficulty breathing and chest pain may occur. In people with a disease of the vascular-cardiac system, for example, atrial fibrillation, pulmonary embolism can occur quite often,” says Shpachenko.
If thromboembolism is suspected, urgent hospitalization is required. To confirm the diagnosis, the hospital will order electrocardiography, chest x-ray and echocardiography. A radionuclide scan of the lungs, probing of the right side of the heart, and computed tomography with contrast of the pulmonary arteries can also be performed.
What is thrombosis?
Thrombosis can be venous or arterial. Venous is considered an acute disease; it appears due to disruption of the structure of the venous wall during injury, surgery, radiation or chemotherapy, due to increased blood clotting, due to a slowdown in the speed of blood flow.
Arterial thrombosis is a pathological condition. Patients have atherosclerotic plaques - cholesterol deposits that narrow the lumen of the artery and provoke circulatory deficiency. Over time, the plaques become clotted.
There is also pulmonary embolism (PE), a fatal disease when the lumen of the pulmonary artery is completely or partially blocked by a blood clot. According to statistics, almost 50% of patients with massive pulmonary embolism die within 30 minutes after its occurrence.
Symptoms
Clinical manifestations of a stationary thrombus are much less pronounced. The patient is rarely bothered by:
- tachycardia;
- shortness of breath when sitting.
In case of mobility in the left atrium, the following are observed:
- excruciating attacks of palpitations, when heart tremors shake the entire chest (what clinicians call “frantic”);
- release of cold sticky sweat;
- sharp pallor with cyanosis of lips and fingers;
- fainting states.
During an attack, the pulse in the radial artery is not detected or is sharply weakened. During auscultation, previously heard noises may disappear. A spherical thrombus or one attached to a “leg” is characterized by symptoms of deterioration in a sitting position, when it descends and clogs the venous opening.
Bringing the patient into a supine state significantly improves well-being.
The duration of attacks of loss of consciousness varies individually: from a few seconds to two hours.
Cardiac surgeons pay attention to the role of irritation of the atrial appendage zone in the reflex spasm of cerebral vessels, since subsequent removal of the blood clot shows that due to its size it could not block the blood flow.
Signs of thrombosis in a patient with heart disease may include:
- persistent heart failure that responds poorly to treatment;
- severe shortness of breath, cyanosis of the arms and legs, tachycardia, yellowing of the skin;
- formation of pulmonary hypertension.
Features of intracardiac localization
Blood clots differ in structure and appearance. In vessels it is customary to distinguish:
- in the arteries - “white” blood clots formed by platelets, leukocytes, fibrin;
- in the veins - “red”, consisting of the same cells + red blood cells;
- hyaline - formed in the capillary bed, do not contain fibrin, it is replaced by proteins.
Cardiac thrombi are mixed, have a motley pattern, a characteristic appearance, and therefore are also called layered. According to their structure, they can be distinguished:
- head (more similar to a “white” blood clot);
- body;
- tail (looks like a “red” blood clot).
The head of the thrombus is attached to the inner wall (endocardial epithelium).
Some properties of intracardiac clots are important in the manifestation of symptoms.
Depending on the ability to move inside the cavity, blood clots can be:
- mobile - move freely in the atria or ventricles, most often formed in the left atrium;
- motionless - one end is attached to the wall, sometimes a “leg” is formed, like in polyps.
In addition, in relation to the cardiac cavity, there are:
- parietal thrombi - more often occurs during an inflammatory process in the endocardium with a transition to the valves, attached to the atrial appendages in case of chronic heart failure, ischemia, to the wall of the aneurysm, leaving a passage for blood flow;
- obstructive - completely block the lumen of the cavity, causing death.
As wall formations grow, they become capable of blocking blood flow
Comparative diagnostics allows us to classify this type as progressive and assume the imminent possibility of complete obturation. Thrombi of the left atrium gradually take on a complete volumetric shape and are called spherical.
With aneurysms, thrombus formation contributes to an increase in volume and expansion. Such a thrombus is called dilatational; it accelerates the thinning of the wall and its rupture.
Could there be a blood clot in the arm?
Blood clot in the arm
According to research and the experience of doctors, blood clots can form in various organs and in any part of the human body, including in the arm. When this happens, a person experiences the following symptoms:
- The affected hand is colder than the other. Due to impaired blood formation, the affected hand becomes colder than the other. But such a symptom is difficult to notice on your own.
- Decreased sensitivity. First, bodily sensations become weak, and then pain sensitivity decreases. A person may not even notice when he is burned by hot objects.
- Swelling of the hand. When there is a blood clot in a vein in the arm, it causes swelling. This symptom is almost impossible to ignore, as it brings severe discomfort.
- Increased body temperature. This happens if a blood clot appears in a vein. Body temperature rises slightly. Usually it is kept at 37.5 - 38.0 degrees.
The first signs of a blood clot:
- The person feels quickly exhausted and tired
- Breathing is difficult
- Dizziness and fainting may occur
- Palpitations, headache
The main danger of thrombosis is that often this disease is not traced and is not felt in any way by the human body. Only some external changes may appear in the affected area, but people often do not attach any importance to this. Therefore, it is important to prevent thrombosis: daily physical activity, do not sit in one place for a long time, monitor your weight and nutrition, drink plenty of water. Good luck!
Do people die from a blood clot: mortality statistics
Thrombus
The formation of a blood clot can occur in different parts of the body and it is very difficult to predict where exactly the blood clot is located. At a critical moment, it breaks away and begins to move, which is instantly fatal. People die from blood clots if treatment is not started in a timely manner and the person does not seek the help of doctors for a long time.
- Mortality statistics are such that more people die from thrombosis than from breast or prostate cancer.
- More than 10 million cases of thromboembolism occur worldwide each year.
Smoking, alcohol, and stress can develop this disease. If you want to be healthy, you should pay more attention to physical education, do morning exercises and worry less. It is also necessary to eat properly and drink clean water. This will guarantee your good health.
If you have blood clots in your legs, can you walk in heels, smoke and drink alcohol?
If you have thrombosis, it is forbidden to wear heels.
We are always told about the dangers of alcohol and smoking on the body. We can say with confidence that these habits provoke the development of thrombosis. For healthy people, as well as for patients with blood clots in the legs, it is harmful to smoke, drink alcohol and for women to walk in heels. Read more below.
Smoking:
- Doctors who often encounter a similar disease have concluded that tobacco plays a big role in the development of thrombosis.
- A person who smokes puts himself at great risk, as the blood thickens and a blood clot can form in the vessels.
- Accordingly, smoking is also harmful in the presence of thrombosis.
Drinking alcohol is also very dangerous for health:
- When a person is in a normal state, his blood moves through the veins at the correct speed.
- As soon as you drink a little strong alcohol, it begins to thicken and move through the veins at high speed.
- People believe that alcohol thins the blood, but this is not true. The speed of blood flow simply increases.
- At this moment, if there are blood clots in the body, they can break away from their base and death will occur instantly.
Women love to dress well and wear high heels:
- If a woman has varicose veins, then such shoes are strictly prohibited.
- The legs will be constantly under tension and this will cause stagnation of blood in the veins, which will have a detrimental effect on health.
- Also, such shoes can provoke the formation of a blood clot.
- If you already have blood clots in your legs, wearing heels is prohibited!
Sitting for long periods of time also has a negative impact on health. Therefore, for example, office workers and people who like to sit at the computer for a long time need to take breaks every hour for 10-15 minutes.
Advice: Try to move more, smoke less and do not drink alcohol, wear the right orthopedic shoes. This will help protect yourself from unwanted consequences.
Summarizing
In recent years, the complexity of the coagulation system has gradually become less mysterious. The discovery of all essential components of the system, the development of mathematical models and the use of new experimental approaches made it possible to lift the veil of secrecy. The structure of the coagulation cascade is being deciphered, and now, as we saw above, for almost every significant part of the system, the role it plays in the regulation of the entire process has been identified or proposed.
Figure 7 shows the most recent attempt to reconsider the structure of the coagulation system. This is the same diagram as in Fig. 1, where parts of the system responsible for different tasks are highlighted with multi-colored shading, as discussed above. Not everything in this scheme is securely established. For example, our theoretical prediction that activation of factor VII by factor Xa allows clotting to respond in a threshold manner to flow rate remains as yet untested experimentally.
Figure 7. Modular structure of the coagulation system: the role of individual coagulation reactions in the functioning of the system.
[1]
It is quite possible that this picture is not yet completely complete. However, progress in this field in recent years gives hope that in the foreseeable future, the remaining unsolved regions of the coagulation circuitry will gain meaningful physiological function. And then it will be possible to talk about the birth of a new concept of blood coagulation, which replaced the old cascade model, which faithfully served medicine for many decades.
The article was written with the participation of A.N. Balandina and F.I. Ataullakhanova and was originally published in Priroda [10].
Regulation of the coagulation system
Figure 6. Contribution of extrinsic and intrinsic tenase to fibrin clot formation in space. We used a mathematical model to investigate how far the influence of a clotting activator (tissue factor) could extend in space. To do this, we calculated the distribution of factor Xa (which determines the distribution of thrombin, which determines the distribution of fibrin). The animation shows the distributions of factor Xa produced by extrinsic tenase (VIIa–TF complex) or intrinsic tenase (IXa–VIIIa complex), as well as the total amount of factor Xa (shaded area). (The inset shows the same thing on a larger concentration scale.) It can be seen that activator-produced factor Xa cannot travel far from the activator due to the high rate of inhibition in the plasma. On the contrary, the IXa–VIIIa complex works far from the activator (since factor IXa is inhibited more slowly and therefore has a greater effective diffusion distance from the activator), and ensures the distribution of factor Xa in space.
[9]
Let's take the next logical step and try to answer the question - how does the system described above work?
Cascade device of the coagulation system
Let's start with the cascade - a chain of enzymes that activate each other. A single enzyme operating at a constant speed produces a linear dependence of product concentration on time. For a cascade of N enzymes, this dependence will have the form tN, where t is time. For the effective operation of the system, it is important that the response is of precisely this “explosive” nature, since this minimizes the period when the fibrin clot is still fragile.
Triggering of coagulation and the role of positive feedbacks
As mentioned in the first part of the article, many clotting reactions are slow. Thus, factors IXa and Xa themselves are very poor enzymes and require cofactors (factors VIIIa and Va, respectively) to function effectively. These cofactors are activated by thrombin, a device where the enzyme activates its own production is called a positive feedback loop.
As we have shown experimentally and theoretically, the positive feedback of factor V activation by thrombin forms the activation threshold - the property of the system not to respond to small activation, but to quickly respond when a large one appears. This ability to switch seems to be very valuable for folding: it helps prevent “false positives” of the system.
The role of the intrinsic pathway in the spatial dynamics of folding
One of the intriguing mysteries that haunted biochemists for many years after the discovery of the essential coagulation proteins was the role of factor XII in hemostasis. Its deficiency was detected in simple clotting tests, increasing the time required for clot formation, but, unlike factor XI deficiency, was not accompanied by coagulation disorders.
One of the most plausible options for unraveling the role of the internal pathway was proposed by us using spatially inhomogeneous experimental systems. Positive feedbacks have been found to be important specifically for the propagation of coagulation. Effective activation of factor X by external tenase on the activator will not help form a clot away from the activator, since factor Xa is rapidly inhibited in the plasma and cannot move far from the activator. But factor IXa, which is inhibited an order of magnitude slower, is quite capable of this (and is helped by factor VIIIa, which is activated by thrombin). And where it is difficult for him to reach, factor XI, also activated by thrombin, begins to work. Thus, the presence of positive feedback loops helps create the three-dimensional structure of the clot.
Protein C pathway as a possible localization mechanism for thrombus formation
Activation of protein C by thrombin itself is slow, but accelerates sharply when thrombin binds to the transmembrane protein thrombomodulin, synthesized by endothelial cells. Activated protein C is capable of destroying factors Va and VIIIa, slowing down the coagulation system by orders of magnitude. The key to understanding the role of this reaction was spatially inhomogeneous experimental approaches. Our experiments suggested that it stops the spatial growth of the thrombus, limiting its size.
So, what is next?
At the first suspicion of thrombosis, you should consult a doctor. In acute cases, the patient is immediately sent to the operating table for vein ligation, installation of a vena cava filter, or surgical removal of a blood clot. But more often thrombosis is treated on an outpatient basis. The doctor will conduct an initial diagnosis, confirm the conclusion with an ultrasound examination (duplex scanning of veins) and prescribe anticoagulants - blood thinners, the task of which is to clear the lumen of the vessel. Be patient! The duration of taking anticoagulants can range from 3 months to conditionally lifelong use. And all this time you will need to visit the clinic so that the doctor evaluates the effectiveness (lack of relapse), safety (lack of bleeding) of therapy and determines the required duration of treatment.