Pressing headaches in the eyes and temples are a common companion for office workers. During the next attack, it is difficult for them to read, especially if the text is written in small print, and in general any attempts to focus their vision on the flickering monitor screen seem unbearable. The easiest way to explain this condition is by banal fatigue, but not everything is as simple as it seems at first glance. The cause may be increased intraocular pressure, and if this diagnosis is confirmed at an appointment with an ophthalmologist, then neither rest nor eye exercises will solve the problem. You need to take measures and drops, and do it as soon as possible - the risk of developing glaucoma at this stage is already very high.
What's pressing on your eye?
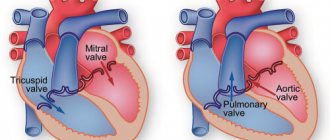
The structure of the eye has a complex structure, but it is not necessary to study it all in detail to understand what intraocular pressure is and why it suddenly deviates from the norm. It is enough to imagine the eye as a liquid surrounded by multiple membranes. The outer one is the sclera, behind it is a network of blood vessels, and even deeper is the ciliary body. When the muscles contract, the shape of the lens changes and the person can see something up close. But this is not the only function of the ciliary body.
Another important task assigned to it is the secretion of intraocular fluid. By circulating between the various chambers of the eye, it ensures normal metabolism and maintains a certain level of intraocular pressure (IOP). In other words, the fluid secreted by the ciliary body constantly puts pressure on the eye, setting the parameters of its normal size and shape. As soon as the amount of this fluid increases excessively or there are problems with its outflow, the pressure will jump. This will entail distortion of the shape, and, consequently, of the entire optical system of the eye.
Important! Intraocular pressure directly affects the quality and acuity of vision. When it deviates from the norm, the shape of the eyeball changes and the mechanisms of accommodation that allow close vision are disrupted.
How to determine IOP at home?
Patients diagnosed with late-stage glaucoma should have their intraocular pressure measured throughout the day. For home measurements, special portable devices are used.
Determination of ophthalmotonus using a home ICare One meter
The device for home determination of IOP is called ICare. The measurements are based on the application of replaceable sensors to the cornea of the eye.
The advantages of this method are:
- High accuracy of results.
- Instant product of measurements.
- Absence of corneal reflex.
- No discomfort during the study.
- Eliminating the possibility of infection.
The device has a built-in memory, so the last ten measurements are always saved.
Normal blood pressure and pathology
Intraocular pressure may fluctuate slightly depending on what time of day the test is performed, but in general it is a constant value. In the morning, intraocular pressure may jump by 2-3 marks. Most likely, the reason lies in the horizontal position of the body, slowing of the pulse and breathing, as well as the predominance of the parasympathetic nervous system during sleep. By evening the pressure gradually drops.
Normal intraocular pressure ranges between 10 and 21 mm. Hg column, although much depends on how the measurement is carried out. These numbers are the limit of true pressure, but if you try to determine it using a tonometric method, the norm will be different - from 12 to 25 mm. Hg Art. That is, it is simply not correct to compare indicators obtained by different methods.
Important! In domestic ophthalmological clinics, the method of the Russian researcher Maklakov is used to measure intraocular pressure. According to it, normal intraocular pressure is that which is below 26 mm Hg, from 27 to 32 mm Hg. Art. – moderately elevated, more than 33 mm Hg. - a reason to take action.
How to measure correctly
To know how to determine eye pressure yourself, you should follow certain recommendations:
- You need to constantly monitor your blood pressure when you feel unwell. For timely detection of deviations in intraocular pressure, measurements are required 4-5 times a week.
- Patients who suffer from hypertension should measure their blood pressure daily.
- When doubt arises about the correctness of the results, the procedure is repeated after 5 minutes.
- During manipulation, you need to ensure that the device lies flat and its tubes are not twisted.
Before the procedure, it is prohibited:
- Drink coffee or smoke.
- Exercise.
- Take a hot bath or visit a sauna.
- Be exposed to ultraviolet radiation for a long time.
- Eat a lot of food.
To know how to determine eye pressure, you need to consult a specialist, since incorrect actions will affect the indicators.
Measurement according to Maklakov
- The patient lies down on the couch, and the doctor administers anesthesia by instilling several drops of dicaine into each eye in turn.
- Then the head is fixed and asked to look at one point.
- A small weight treated with special marking paint is carefully lowered onto the open eye, under the pressure of which the eyeball should be slightly deformed.
- Now the weight is lowered onto a sheet of paper to see how much paint is left on it. Intraocular pressure is determined by the intensity of the imprint.
- The procedure is repeated again in both eyes to avoid the possibility of misinterpretation.
Naturally, some amount of paint from the load will remain on the surface of the eyeball, but it will quickly be washed away with tears. Instead of weights, ophthalmologists sometimes use a portable device that looks like a ballpoint pen. They also apply pressure on the eye, having previously treated the eyeball with an anesthetic.
This method also has an alternative – non-contact tonometry. No weights are placed on the eye, but instead a controlled air flow is used. Many patients find this method more acceptable, but in reality it is rarely used - it is not as accurate.
Important! In patients with glaucoma, eye pressure fluctuates much more noticeably throughout the day than in healthy people. Having such suspicions, the doctor may ask the patient to come to the clinic several times throughout the day. To ensure the accuracy of the diagnosis, you need to measure your blood pressure at least three times before lunch, and the same number in the evening.
How to measure the pressure inside the eye yourself?
Without the help of a doctor and special equipment, it is impossible to determine with what force the fluid secreted by the ciliary body presses on the eye. Nevertheless, it is possible to understand that blood pressure is greatly increased, and ophthalmologists recommend that everyone master this simple technique.
Close your eyes and relax. Now gently press your index finger on the eyeball. You should feel an elastic ball that gives in to your pressure - this is normal. If the eye is very hard and practically does not deform, most likely the IOP level is elevated and it is better to consult a specialist to make sure that its value is not critical.
Indications for diagnostics
In ophthalmology, intraocular pressure is measured according to indications, that is, symptoms that patients complain about. These include:
How to get rid of eye pressure
- Visual dysfunction.
- Formation of a film before the eyes.
- Headache radiating to the temporal and ocular areas.
- Rapid eye fatigue.
- Twilight vision disorder.
- Redness of the outer shell of the eye.
- Concentration on an object is accompanied by painful sensations.
- Pain when blinking eyelids.
- Dry mucous membrane.
- Changing the shape of the pupil.
- Narrowing of visual fields.
For persons over 40 years of age, this procedure is mandatory during a preventive examination and is carried out once a year, regardless of the complaints detected.
In patients diagnosed with glaucoma, examination is carried out once every trimester. If you have a genetic predisposition to glaucoma, for preventive purposes, experts recommend taking measurements once every 2 years, provided there are no pathological symptoms.
Patients suffering from hypertension also require constant monitoring of IOP levels, since a persistent increase in blood pressure leads to irreversible changes in the retinal vessels. Regular examination by an ophthalmologist allows you to assess the degree of damage to the optic nerves and prevent the development of complications.
Why does intraocular pressure increase?
Two parts are responsible for the regulation of intraocular pressure - the nervous system and some hormones. That is why most often a temporary increase in IOP is associated with increased mental work, stress and the experience of violent emotions. In women, the risk of glaucoma can develop during menopause, when large-scale hormonal changes occur in the body.
So, the true cause of IOP most often needs to be looked for in one of the following directions.
- Chronic stressful situations, prolonged mental or physical stress.
- Problems with the cardiovascular system that provoke surges in blood pressure.
- Some kidney diseases, due to which a lot of fluid is retained in the body.
- Endocrine pathologies, in particular increased levels of adrenal hormones in the blood, hypothyroidism.
- Anatomical pathology in the structure of the eyeball. People suffering from atherosclerosis should be especially careful in this regard.
In any case, it is important to understand that intraocular pressure does not suddenly increase on its own, it is always a consequence. Sometimes - hidden pathological processes occurring in the body, and sometimes - diseases associated directly with the eyes. So, a jump in IOP can be provoked by:
- an eye tumor that puts pressure on the inner membranes and chambers of the eye, thereby interfering with the normal outflow of fluid;
- inflammatory disease of the iris (iritis), ciliary body (cyclitis), choroid (uveitis);
- severe eye injury, after which inflammation, swelling and stagnation of blood in the vessels inevitably appears.
Important! Under any of the above circumstances, IOP cannot be critically high all the time. It increases periodically, in jumps, which depend on the characteristics of the course of the disease that provokes it. But if the pathology is not found and treated, then with age, increased IOP can transform into glaucoma. Gradually, due to strong pressure, the retinal cells will be destroyed, the optic nerve will atrophy, and eventually the person will completely lose vision.
Low eye pressure
Low fundus pressure is dangerous because it does not have pronounced symptoms. The patient experiences a gradual decrease in vision, so often the problem can be detected at an advanced stage. Symptoms such as dizziness, pain in the temples, as well as pain and burning in the eyes are absent.
With a long course of the disease, you can see a visual decrease in the size of the eyes - they lose their shine and become “dry”.
In the most severe cases, the eyeballs become sunken and emergency medical attention is required.
A decrease in eye pressure can be caused by a number of reasons, one of which is a decrease in blood pressure. This is due to the fact that with hypotension, the pressure in the capillaries of the eye drops significantly, which negatively affects the state of the visual system. The problem is also often associated with dehydration, purulent-inflammatory processes of the eyeball (uveitis, iritis, etc.) and infections. In this case, there is a sharp deterioration in vision.
Retinal detachment leads to a decrease in fundus pressure, since this disease is accompanied by a violation of the mechanism of formation of intraocular fluid. Serious injuries and foreign bodies in the eye can also cause this problem.
With severe mechanical damage to the organs of vision, a progressive decrease in IOP indicates the initial stage of atrophy of the eyeball. Less common causes of the disease include ketoacidosis, an acute condition that occurs in patients with diabetes, as well as severe liver disease.
Low eye pressure: symptoms
- Gradual deterioration of vision;
- Visual reduction in eye size with a long course of the disease;
- Recession of the eyeballs (in the most severe cases);
- A sharp deterioration in vision (at the initial stage of optic nerve atrophy caused by severe mechanical damage).
How to relieve intraocular pressure?
Trying to deal with the consequences without eliminating the cause is useless. That is why, if you notice that your eyes are constantly tired, red and very tense, you need to look for a reason that provokes periodic jumps in intraocular pressure. Further, the method of eye restoration will depend on how neglected everything is.
If we are talking about the initial stages and barely noticeable symptoms, then, most likely, preventive measures alone will be sufficient:
- master a set of eye exercises and devote a few minutes a day to it;
- choose safety glasses for reading and standing in front of a monitor;
- As far as possible, limit any eye strain - TV, computer, working with small parts;
- give up contact and strength sports;
- Spend free time outdoors, giving your eyes a chance to rest and look into the distance.
Treatment of intraocular pressure with drops
When high IOP ceases to be episodic and develops into ocular hypertension or hypotension, preventive measures alone are not enough - timely local treatment is needed. With such diagnoses, the easiest way to regulate the pressure in the eye is with eye drops. They come in several types.
- Those that act directly on the ciliary body and reduce fluid production are carbonic anhydrase inhibitors. The most popular of this group are Azopt and Trusopt. By reducing the amount of intraocular fluid, the pressure also decreases, but this process can be accompanied by burning, severe redness of the eyes and even a bitter taste in the mouth.
- The second category is prostaglandins. They operate on a different principle: they affect not the amount of fluid, but its intensive outflow. If this is the problem, Travatan, Taflotan and Xalatan are most often prescribed. But they also have side effects - the iris of the eye may darken.
- Beta blockers - for example, Timolol, Okumol, Okupress, Arutimol, Okumed and the more modern Betoptik. They also reduce the amount of fluid formed in the eye, but have one significant nuance - together with eye pressure, they reduce the heart rate, which is strictly contraindicated for heart patients.
There are also combination drugs that act in two directions: on the one hand, they inhibit the process of fluid production, and on the other, they increase its outflow. This category includes “Xalacom”, “Fotil”, “Kosopt”.
Important! On average, drops are used twice a day, but the exact dosage and frequency of instillation can only be determined by a doctor, having an accurate description of the clinical picture. By self-medicating, you can not only further damage your vision, but also damage your cardiovascular system, lungs and kidneys.
Relieving intraocular pressure at home
If you feel pressure in your eyes, but cannot immediately get an appointment with an ophthalmologist, then instead of drops you can try to relieve painful symptoms using traditional methods. Helps normalize eye pressure:
- meadow clover decoction (brew with boiling water, leave for 2 hours and drink 100 g before bedtime);
- tincture of golden mustache (pour about 20 purple inflorescences with 500 grams of vodka and leave in a dark place for 12 days, then take one teaspoon before breakfast);
- a glass of kefir with cinnamon.
No matter how tempting such treatment may seem, ophthalmologists do not recommend relying too much on it. Such recipes can be used only if the pressure jumps rarely and not greatly. Trying to get rid of serious symptoms that indicate progressive blindness in this way is simply dangerous.
Most of these arrogant patients, when they finally get to the ophthalmologist’s office, hear one thing: “an operation is necessary.” A laser is used to relieve high intraocular pressure. Depending on where the problem is located, they can either excise the iris or stretch the trabecula to increase the flow of fluid.
If you don't want to end up in the operating room, take the advice of ophthalmologists seriously and constantly engage in prevention. A five-minute break every hour of working near the computer, a simple set of gymnastic exercises for the eyes, a dinner of sea fish and blueberry-carrot snacks - and you will maintain sharp vision for many years!
Sources used:
- Volkov, V.V. Glaucoma at pseudonormal pressure / V.V. Volkov. - M.: Medicine, 2001.
- Lusine, Levonovna Harutyunyan Determination of target pressure in primary open-angle glaucoma: monograph. / Lusine Levonovna Harutyunyan. - M.: LAP Lambert Academic Publishing, 2013.
- D. Hubel. Eye, brain, vision. — ed. A. L. Byzova. - M.: Mir, 1990.
- American Optometric Association - Ocular Hypertension
Basic methods of determination
In ophthalmological diagnostics, tonometric and tonographic research methods make it possible to determine a rational method of treating glaucoma, as well as the dynamics and complications of the disease.
The measurement of ophthalmotonus differs in technique, including:
- Palpation (finger).
- Instrumental (contact, non-contact).
During the procedure, the ophthalmologist determines the degree of elasticity of the eyeball, based on identifying the level of deformation during external exposure.
Finger technique
Palpation is the simplest technique for determining the degree of ophthalmotonus. The technique is used in cases where there are contraindications to direct contact of the instrument with the eyeball or when there is a likelihood of obtaining inaccurate results as a result of injury to the cornea after eye surgery. There are two options for carrying out the technique:
- Direct palpation of the eyeball after anesthesia is used during the operation.
- Transpalepebral palpation is carried out through the eyelids by pressing the fingers of both hands above the upper ocular cartilage, and the degree of eye hardness is assessed.
Iphthalmotonus can be determined by scleral compliance. So, at a normal level of pressure, shocks are felt during squeezing, an increased level requires more pressure, and the shock becomes weaker.
The study determines the difference in pressure between both eyes. To interpret the results obtained, there is a system for assessing ophthalmotonus, where:
- T-pressure is normal.
- T+1 – some compaction compared to the norm.
- T+2 is a significant excess of the norm, but indentation of the fibrous membranes is observed.
- T+3 – excessive increase in density, inability to press in the eyeballs.
Measurement by this method is inaccurate and is not acceptable for clinical research. Due to the ease of implementation and the absence of the need for devices, the method can be used in emergency situations.
Contact methods of ocular tonometry
There are several types of contact devices for determining the level of intraocular pressure. Their main advantage is the high accuracy of the results obtained, where the error is 1 mm Hg. Art. The disadvantage of this method is the high probability of infection and the need for preliminary anesthesia before manipulation. These devices are used to measure ophthalmotonus in adults, since children offer resistance, which leads to injury to the visual apparatus.
The principle of tonometry according to Maklakov
Maklakov’s device is widely used throughout Russia due to its ease of use, low cost of the procedure and high accuracy of the data obtained.
Tonometry according to Maklakov
Algorithm for tonometry:
- The patient takes a comfortable body position on the couch. Special anesthetic drops are dripped onto the mucous membrane of the eyes.
- Before starting the study, the tonometer, with two weights on the base, is moistened in a dye solution.
- One weight is located in the central part of the cornea of the right eye, and the other in the left.
- The meters are removed and placed on ink-based fingerprint paper.
- The patient is additionally instilled with anesthetic drops to reduce the risk of infection.
You can measure prints using a measuring ruler, the numbers on which indicate the amount of eye pressure in mm. Hg Art.
Goldman tonometry
Recently, Goldmann tonometry has been most often used in comparison with the Maklakov technique. The study takes into account the thickness and stiffness of the cornea, the tension of the tear film and other factors.
Goldmann ophthalmotonus is measured using a slit lamp. Anesthetic drops and a fluorescent substance are instilled into the conjunctival sac. A prism is placed opposite the apex of the cornea, and then the beam is directed through a filter in an oblique projection. When examined by a specialist through a slit lamp, two half rings are observed above and below the horizontal line. The scale is installed at the point where the inner edges of the half rings touch.
Non-contact tonometry
The non-contact method is a screening method without the use of local anesthetics. The ophthalmological method is based on the effect of a short-term air pulse on the cornea. The air gun contains optical sensors that record the movement of the cornea. During the study, the measuring device increases the force of the air flow. Reflecting from the cornea, the light beam enters the receiver. If there are seals on the cornea, the reflected signal will be as bright as possible. Since the technique is applanation, differences in the properties of the cornea of the person being measured leads to an error.
Schiotz technique
The technique involves the use of a weight on a metal rod, which is used to press on the cornea. The patient is given local anesthesia, but no dye is applied. The weight is applied to the eyeball, which is affected by internal ocular pressure. It counteracts the pressure of the load, as a result of which the arrow of the device deviates to the side. The deflection of the needle is measured using a special scale, and the obtained values are entered into the calibration table.
Transpalpebral tonometry
The method is based on recording the free stem in the area where the eyelid is completely compressed. Thus, a study of the biochemical properties of the eyelids for ophthalmotonus is taking place. The technique allows you to determine intraocular pressure without direct impact on the cornea, which is necessary in the presence of pathological changes in the organ.
IOP measurement is carried out as follows:
- The patient takes a position in which the head is in a horizontal position without tilting.
- The patient's gaze is fixed so that the line of sight is at an angle of 45 degrees.
- The tip of the tonometer is located near the anterior edge of the upper eyelid.
- While lowering the tonometer body, its vertical position must be maintained.
- When the rod falls on the eyelid, the device produces a sound signal.
Dynamic contour tonometry (Pascal)
Measurement with a Pascal tonometer is a modern automatic method, during which the results are reflected on the monitor with high accuracy down to tenths of mm. Hg Art. The principle of the technique is based on recording pulse waves for 5–7 minutes, after which the final data is calculated as the average diastolic value.
Important! Using a parting, you can measure the amplitude of the ocular pulse, which serves as an important diagnostic criterion for glaucoma and other vascular pathologies in the early stages.
Coherence optical tomography
The non-contact method allows the assessment of eye tissue using an infrared beam that is projected onto the retinal membrane. As a result of diagnostics, interference data appears. During the study, the ophthalmologist receives several pictures, from which he selects the one with the most complete overview. Based on the selected picture, the specialist draws up maps, protocols, tables that allow you to determine the value of IOP.
Daily measurement method
The specialist must write a prescription for 24-hour intraocular pressure monitoring. Using this method, glaucoma can be detected at an early stage. The technique is carried out using a Maklakov, Goldman tonometer and non-contact devices. Data is measured several times a day at certain times for 7 days or more.
Daily tonometry allows you to establish average IOP values in the morning, evening and night, as well as calculate the amplitude of fluctuations between them. Values exceeding 5 mmHg. Art., are a sign of the development of a pathological condition.
Portable blood pressure monitors
The non-contact method of examination is the most preferable for many patients. However, some people have to use contact tonometers. This is a portable type of device. People who have severe glaucoma should measure their eye pressure daily, even several times a day. To do this, they have to purchase portable blood pressure monitors. They are usually equipped with replaceable sensors that are applied to the cornea. Disposable attachments help avoid infection of the organs of vision. The pressure in the eyes with glaucoma can change very dramatically. Physical activity, overwork, and stressful situations lead to an increase in ophthalmotonus. Therefore, you have to keep the tonometer with you almost always.
Glaucoma can be open-angle or closed-angle. The second type of pathology is dangerous because it progresses very quickly. The patient may lose almost all visual functions in a few hours, which will subsequently be impossible to restore. In this regard, at the first signs of glaucoma, which include pain in the eyes, rainbow circles, narrowing of the visual fields, you should immediately sign up for tonometry. You can also undergo this procedure at our CDC. We measure intraocular pressure using a non-contact method using a pneumotonometer.