All types of circulatory disorders in the human body also affect the substance of the brain, which ultimately affects its integrity and the ability to function normally.
And “starvation” of cells, which is provoked by a violation or complete cessation of blood supply (in medicine, this process is called ischemia), causes a change in the brain substance of a dystrophic nature. That is, degeneration, and sometimes, although very rarely, even the disappearance of tissues and a significant deterioration in their function.
We will talk more about this pathological condition in the article.
At-risk groups
Typically, focal changes in the white matter of the brain of a dystrophic nature most often occur in old age. Most lesions appear during life and as a result of hypoxia and ischemia. People who lead a sedentary and unhealthy lifestyle are also susceptible to the disease. Genetic predisposition also plays a role. The risk group includes people suffering from high or low blood pressure, diabetes, rheumatism, obesity and atherosclerosis. In addition, emotional individuals prone to stress are at risk of developing pathology.
You may be interested: Inhalations with Miramistin in a nebulizer
The white matter of the brain coordinates all human activity. It is what connects different parts of the nervous system. White matter is necessary for the two hemispheres to work together.
Prevention
Prevention of multiple focal changes in the brain substance includes:
- Maintaining an active lifestyle. After all, movement stimulates improved blood circulation throughout the human body and in the brain, in particular, and thereby reduces the risk of lesions in the brain.
- Proper and rational nutrition.
- Avoiding stress and other nervous situations. After all, constant nervous tension can be the cause of more than one disease. There is no need to overwork often, you should rest and relax more.
- Healthy and sound sleep is always the key to health. You need to spend at least 7-8 hours sleeping per day. If you experience insomnia or any other sleep pathologies, then your sleep time should be increased to 10 hours a day.
- It is necessary to conduct an examination in the hospital every year to identify hidden pathologies and diseases. If symptoms are detected that may indicate changes in the brain matter, then an MRI is required 2 times a year, as well as all necessary tests.
Everyone knows that it is always easier to prevent a problem in advance than to look for a right and proper solution later. The same goes for health. It is easier to carry out the necessary prevention than to treat the disease later.
Source: glmozg.ru
Causes
You may be interested in: The act of defecation: mechanism, regularity, causes of violations
Focal changes in the brain substance of a dystrophic nature occur in a number of diseases of different origins:
- Changes in vascular origin: atherosclerosis, migraine, hypertension, etc.
- Inflammatory diseases. Multiple sclerosis, Behcet's disease, Sjögren's disease, inflammatory bowel disease (Crohn's disease).
- Infectious diseases. HIV, syphilis, borreliosis.
- Intoxication and metabolic disorders, carbon monoxide poisoning, B12 deficiency.
- Traumatic processes associated with radiation therapy.
- Congenital diseases caused by metabolic disorders.
The occurrence of pathology is caused by impaired blood supply in any part of the brain. It is fraught with loss of function of brain tissue. The more blood flow has decreased, the more noticeable the consequences. An example is damage to the spinal or cerebral blood flow. Such violations progress slowly, but entail serious consequences.
Diseases of vascular origin
Here it should be clarified: vascular genesis is an indication of the origin of the disease, and not the disease itself. When talking about brain diseases of vascular origin, we mean changes associated with circulatory disorders - in venules, arteries, veins, and so on.
These types of violations are divided into several main groups.
- Transient cerebral circulatory disorders are distinguished between general cerebral and focal. The first are characterized by headache, nausea, vomiting; focal ones are responsible for short-term disturbances in motor functions and sensitivity of certain parts of the body. A distinctive feature of this vascular disorder is reversibility . Treatment promises complete restoration of function.
- Blockage of the arteries - narrowing of the working channel in any case leads to deterioration of nutrition, which significantly affects the functionality of the served areas of the brain, and can cause changes of an ischemic nature. Here treatment may even include surgery.
- Rupture of a cerebral aneurysm, cerebral hemorrhage – in fact, a stroke of ischemic or hemorrhagic origin.
Signs
You may be interested in:Hot spring "Avan" in Tyumen: detailed information
The signs of focal changes in the brain substance of a dystrophic nature are also different. With focal changes, not the entire brain suffers, but only its individual parts. Tissue degeneration occurs when there is insufficient supply of nutrients necessary for the normal functioning of the body’s nervous systems. We are talking about proteins - the building material of the human body. Proteins break down into amino acids, which, in turn, stimulate the nervous system. It also requires fats and carbohydrates - the main sources of energy needed by every living creature.
Of the vitamins, the brain needs B1 (activates its work), B3 (provides energy at the intracellular level), B6 (it is difficult to imagine metabolic processes without it, in addition, it is also a kind of antidepressant), B12 (promotes memory preservation and helps to stay alert) . All these vitamins can be obtained in sufficient quantities by creating the right diet.
The main signs of the presence of focal disorders
One of the main symptoms is hypertension. After all, if blood circulation in the brain is impaired, then it will suffer from a lack of oxygen, and this, in turn, will immediately lead to an acceleration of signals about the supply of blood to the brain, thereby increasing blood pressure. In addition, epileptic seizures may be observed in a sick person. A variety of mental disorders are also the main sign of focal brain damage. Indeed, with pathological phenomena in the subarachnoid spaces, hemorrhages often occur. This can also lead to formations in the fundus, darkening and other symptoms that appear in the fundus. Here, dark spots form very quickly, blood vessels around the eye burst and the retina can rupture. Using these signs, you can determine exactly where multiple foci are located.
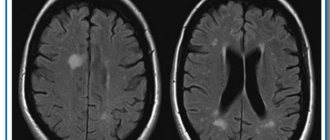
A possible stroke or micro-stroke is also the main sign. Focal changes in the brain are usually clearly visible on MRI, which makes it possible to determine the pre-stroke condition. This will allow the doctor to immediately prescribe the necessary treatment. The most obvious signs of damage can be considered single and multiple, small and large involuntary muscle contractions.
And, of course, pain is no exception. Migraines, frequent and severe headaches clearly indicate disorders of a multifocal nature.
Pathologies
Focal changes in the substance of the brain of a dystrophic nature most often take the form of pathologies such as:
- A cyst is a small cavity that is filled with fluid. It often interferes with the normal functioning of neighboring areas of the brain, as it compresses blood vessels. Cysts are divided into intracerebral (cerebral) and arachnoid. The latter appears in the meninges. Its occurrence is promoted by the accumulation of cerebrospinal fluid and inflammatory processes. Cerebral occurs in place of dead brain tissue.
- Necrotic state of tissue - appears when the supply of important nutrients to areas of the brain for any reason deteriorates. Dead cells form so-called dead zones and are not regenerated.
- Hematomas and brain scars occur after severe trauma or concussion. Foci of this type lead to structural damage.
Characteristics of the pathology
h21,0,0,0,0–> p, blockquote3,0,0,0,0–>
When talking about vascular genesis, experts mean not one specific disease, but the nature of the occurrence of a certain pathology caused by damage to the blood supply system to the brain. Depending on the nature of the violation, there are:
p, blockquote4,0,0,0,0–>
- General or organic disorders, accompanied by frequent headaches, nausea, dizziness, vomiting.
- Focal changes characterized by the formation of a pathological focus that causes a disorder of certain functions.
The focus of inflammation of the white matter can manifest itself in the development of multiple sclerosis, encephalomyelitis, sclerosing panencephalitis, and neurosarcoidosis. Small foci of vascular origin are provoked by arterial hypertension, necrosis of brain tissue, cysts, intracerebral scars that remain after injuries to the neck and head.
- Cerebral ischemia: what is it and how to treat it?
p, blockquote5,0,0,0,0–>
Several main vessels are responsible for feeding the brain. If blood circulation in them is impaired, various vascular diseases develop. The main types of pathology include:
p, blockquote6,0,0,0,0–>
- A transistor disorder in the circulatory system, in which motor functions are affected, and numbness of the limbs and other parts of the body is observed. With timely treatment, the pathological process can be stopped and damaged functions can be completely restored.
- Narrowing and blocking of vascular lumens, leading to disruption of neuron nutrition, which leads to ischemia of certain parts of the brain.
- Aneurysm of the cerebral arteries. As a result of its rupture, hemorrhage occurs in the brain.
- Ischemic stroke can develop as a separate pathology or as a result of organic changes.
Diagnostics
The complete picture of focal changes in the brain substance of a dystrophic nature is determined using an MRI study. This procedure allows you to see even small areas of transformation in the white matter. And they, in turn, lead to cancer and stroke.
Focal dystrophic lesions come in different sizes and differ in location. Based on this, the examination may show some types of disorders.
In the cerebral hemisphere, blockage of vital arteries is usually diagnosed due to abnormal development of the embryo or acquired atherosclerotic plaques. A herniated cervical spine is also detected.
Changes in the white matter of the brain indicate hypertension and congenital developmental anomalies. In other cases, numerous areas of brain pathology may indicate a pre-stroke condition, senile dementia, or epilepsy.
Sometimes doctors perform tests on a patient to detect the presence of cognitive impairment. That is, cognitive dysfunction. Such as orientation in space and time, understanding of external processes, the ability to remember information, drawing, writing, reading, etc.
Focal changes in the brain substance of a dystrophic nature can develop in three ways:
- In the first case, the disease is remitting in nature. Symptoms increase gradually, the condition worsens, and brain productivity decreases. But from time to time, remissions occur—temporary improvements in health, after which the patient becomes worse again.
- Progressive focal changes in the brain substance of a dyscirculatory dystrophic nature develop very quickly. Each stage of the disease takes no more than two years, which is considered a short period for organic brain lesions.
- Typically, the deterioration of a person suffering from focal changes lasts for many years, eventually leading to dementia.
It should be remembered that single focal changes in the brain substance of a dystrophic nature often appear in young people, and single damage to the white matter in an elderly person is considered normal. Structural disorders of the cerebral arteries of the atherosclerotic type appear in 50% of patients over 50 years of age. For the most part, hypertensive patients suffer from this. Therefore, you need to show the MRI result to a neurologist so that he can determine the severity of the disorders in the brain by comparing the MRI result and the clinical picture of the disease.
Diagnosis of the disease
This disease is extremely difficult to diagnose in the early stages, especially with single changes in the brain. Quite often, during examination, doctors do not find any significant deviations from the norm. But if there are obvious disturbances in your well-being, you should not calm down. It is necessary to continue further, more detailed examination.
Survey forms:
- computed tomography makes it possible to examine vessels for the presence of congenital or acquired vascular pathologies;
- Magnetic resonance imaging makes it possible to get a complete picture of the condition of blood vessels;
- magnetic resonance angiography is performed to determine the state of the gray matter and the presence of small focal changes in the brain of vascular origin;
- Dopplerography is carried out to clarify the speed of blood flow;
- electroencephalography diagnoses the structure of the brain of a sick person;
- spectroscopy allows you to analyze processes (biochemical) in brain tissue.
If the patient has obvious functional disorders of other organs, he is referred to other specialists for consultation. For example, if vision deteriorates, the patient is referred to an ophthalmologist.
When conducting any type of examination, if there is a suspicion of this disease, the patient is also prescribed a detailed examination of cardiac activity.
Diet
In the early stages of this disease, it is enough to reconsider your lifestyle and diet, choosing a more gentle regimen and diet. In the diet, it is advised to reduce the consumption of animal fats, and it is better to completely replace them with vegetable ones. You should eat fish and seafood instead of fatty meat, and reduce the amount of salt in your diet. Fresh vegetables and fruits will be of great benefit.
Focal changes in the brain substance of a dystrophic nature
Sooner or later, all people grow old, and the body ages along with them. It primarily affects the heart, brain and spinal cord. If the heart ceases to properly cope with its task - pumping blood - then over time this will affect the condition of the brain, the cells of which will not receive enough nutrients to maintain vital functions.
According to various sources, from 50 to 70% of elderly people (over 60 years old) suffer from a similar disease.
Treatment
There are a huge number of focal anomalies, so each has its own cause. Treatment of brain pathologies is based on the destruction of those factors that led to the appearance of lesions in brain tissue. In addition to eliminating the underlying disease, the doctor may also prescribe vitamins and medications to help combat the deterioration of cerebral blood flow.
The treatment process depends directly on what somatic problems in the body led to the occurrence of lesions in the brain. For infections, for example, antibiotics are taken; for injuries, diuretics, decongestants, and anticonvulsants are taken. If the damage to the brain tissue was caused by a circulatory disorder, then nootropics and coagulants are prescribed.
Source
Methods of combating pathology
Irreversible consequences of brain damage require an integrated approach to treatment and fundamental changes in the usual lifestyle:
- Rejection of bad habits;
- Physical activity - walking and swimming to strengthen the heart muscle;
- Dieting - table number 10 - limiting salt, fatty and spicy foods. Mostly boiled or steamed food;
- Maintaining a rest regime - in case of brain pathologies, it is necessary to increase sleep by several hours;
- Avoidance of stress – an unstable emotional state directly affects the causes of many diseases.
Drug therapy is aimed at eliminating cognitive disorders and treating the underlying disease, which causes changes in brain tissue:
- Drugs to improve blood supply (help replenish oxygen deficiency in tissues);
- Analgesics (pain relief);
- Antiepileptic drugs (relief of convulsive syndrome);
- Beta-blockers (blood pressure control to exclude hypertensive crises);
- Non-steroidal anti-inflammatory drugs;
- B vitamins (restoration of the nervous system);
- Antidepressants (for anxiety disorders);
- Nootropic drugs (restoration of cognitive abilities).
For minor lesions, it is possible to slow down the progressive process by following the neurologist’s instructions and undergoing an annual re-examination of the cerebral vessels.
Preventive measures aimed at maintaining a healthy lifestyle and annual scheduled examinations with a neurologist can minimize the risk for people predisposed to vascular pathologies.
Dysfunctional brain disorders affect the quality of life and the course of the disease, leading to death in cases of extensive damage to brain tissue. Timely treatment does not eliminate the pathology, but it is possible to slow down the atrophic processes and improve fading vital functions.
Symptoms of dystrophy of the brain substance
It is better to prevent any disease than to treat it later, and for this you need to know its external manifestations (signs) and symptoms.
- First stage. In the first couple of days, a person feels a little tired, lethargic, dizzy and sleeps poorly. This occurs due to decreased blood circulation in the brain. The degree of significance increases with the development of vascular diseases: cholesterol deposition, hypotension, etc.
- Second stage. At the second stage, a so-called “disease focus” appears in the brain; damage to the brain substance deepens due to poor blood circulation. The cells do not receive enough nutrition and gradually die. The beginning of this stage is indicated by memory impairment, loss of coordination, noise or “shooting” in the ears and severe headaches.
- Third stage. Due to the discircular nature of the last stage, the focus of the disease moves even deeper, the affected vessels bring too little blood to the brain. The patient exhibits signs of dementia, lack of coordination of movements (not always), dysfunction of the sensory organs is possible: loss of vision, hearing, shaking hands, etc.
The exact changes in the brain substance can be determined using MRI.
Without treatment, diseases such as:
- Alzheimer's disease. The most common form of nervous system degeneration.
- Pick's disease. A rare progressive disease of the nervous system, manifesting itself from 50-60 years of age.
- Huntington's disease. Genetic disease of the nervous system. developing from 30-50 years.
- Arterial hypertension.
- Cardiocerebral syndrome (impairment of basic brain functions due to cardiac pathology).
Chronic cerebral ischemia
Cerebrovascular diseases are one of the main problems of modern medicine. It is known that in recent years the structure of vascular diseases of the brain has changed due to the increase in ischemic forms. This is due to an increase in the proportion of arterial hypertension and atherosclerosis as the main cause of cerebrovascular pathology. When studying individual forms of cerebral circulatory disorders, chronic ischemia ranks first in prevalence.
Chronic cerebral ischemia (CHI) is a special type of vascular cerebral pathology caused by a slowly progressive diffuse disorder of the blood supply to the brain with gradually increasing various defects in its functioning. The term “chronic cerebral ischemia” is used in accordance with the International Classification of Diseases, 10th revision, instead of the previously used term “dyscirculatory encephalopathy”.
The development of chronic cerebral ischemia is promoted by a number of reasons, which are commonly called risk factors. Risk factors are divided into correctable and non-correctable. Uncorrectable factors include old age, gender, and hereditary predisposition. It is known, for example, that a stroke or encephalopathy in parents increases the likelihood of vascular diseases in children. These factors cannot be influenced, but they help to identify in advance those at increased risk of developing vascular pathology and help prevent the development of the disease. The main correctable factors in the development of chronic ischemia are atherosclerosis and hypertension. Diabetes mellitus, smoking, alcohol, obesity, insufficient physical activity, poor nutrition are the reasons that lead to the progression of atherosclerosis and the deterioration of the patient’s condition. In these cases, the blood coagulation and anticoagulation system is disrupted, and the development of atherosclerotic plaques is accelerated. Due to this, the lumen of the artery decreases or is completely blocked (Fig.). At the same time, the crisis course of hypertension is especially dangerous: it leads to an increase in the load on the blood vessels of the brain. Arteries modified by atherosclerosis are unable to maintain normal cerebral blood flow. The walls of the vessel gradually become thinner, which can ultimately lead to the development of a stroke.
| Drawing. MR angiogram: occlusion of the right middle cerebral artery |
The etiology of CCI is associated with occlusive atherosclerotic stenosis, thrombosis, and embolism. A certain role is played by post-traumatic dissection of the vertebral arteries, extravasal compression due to pathology of the spine or neck muscles, deformation of the arteries with permanent or periodic disturbances in their patency, hemorheological changes in the blood (increased hematocrit, viscosity, fibrinogen, platelet aggregation and adhesion). It must be borne in mind that symptoms similar to those that occur with chronic ischemia can be caused not only by vascular, but also by other factors - chronic infection, neuroses, allergic conditions, malignant tumors and other reasons with which a differential diagnosis should be made . If the described disorders are supposed to have a vascular origin, instrumental and laboratory confirmation of damage to the cardiovascular system is necessary (ECG, Doppler ultrasound of the main arteries of the head, MRA, MRI, CT, biochemical blood tests, etc.).
To make a diagnosis, one must adhere to strict diagnostic criteria: the presence of cause-and-effect relationships (clinical, anamnestic, instrumental) of brain lesions with hemodynamic disturbances with the development of clinical, neuropsychological, psychiatric symptoms; signs of progression of cerebrovascular insufficiency. The possibility of subclinical acute cerebral dyscirculatory disorders, including small-focal, lacunar infarctions, which form symptoms characteristic of encephalopathy, should be taken into account. For the main etiological reasons, atherosclerotic, hypertensive, mixed, and venous encephalopathies are distinguished, although other causes leading to chronic cerebral vascular insufficiency (rheumatism, vasculitis of other etiologies, blood diseases, etc.) are also possible.
The pathomorphological picture of CCI is characterized by areas of ischemically altered neurons or their loss with the development of gliosis. Small cavities (lacunae) and larger lesions develop. With multiple lacunae, the so-called “lacunary state” is formed. These changes are predominantly observed in the area of the basal ganglia and have a typical clinical expression in the form of amyostatic and pseudobulbar syndromes, dementia, described at the beginning of the twentieth century. French neurologist P. Marie. The development of status lacunaris is most characteristic of arterial hypertension. In this case, changes in blood vessels are observed in the form of fibrinoid necrosis of the walls, their plasmatic impregnation, the formation of miliary aneurysms, and stenoses.
The so-called criblures, which are dilated perivascular spaces, are distinguished as changes characteristic of hypertensive encephalopathy. Thus, the chronic nature of the process is pathomorphologically confirmed by multiple zones of brain ischemia, especially its subcortical regions and cortex, accompanied by atrophic changes developing against the background of corresponding changes in the cerebral vessels. Using CT and MRI, in typical cases, multiple microfocal changes are detected, mainly in the subcortical zones, periventricularly, often accompanied by cortical atrophy, dilation of the cerebral ventricles, and the phenomenon of leukoaraiosis (“periventricular glow”), which is a reflection of the demyelination process. However, similar changes can be observed during normal aging and primary degenerative-atrophic processes of the brain.
Clinical manifestations of CCI are not always detected by CT and MRI studies. Therefore, the diagnostic significance of neuroimaging methods cannot be overestimated. Making a correct diagnosis for a patient requires an objective analysis of the clinical picture and instrumental examination data from the doctor.
The pathogenesis of cerebral ischemia is caused by insufficiency of cerebral circulation in its relatively stable form or in the form of repeated short-term episodes of discirculation.
As a result of pathological changes in the vascular wall, developing as a result of arterial hypertension, atherosclerosis, vasculitis, etc., autoregulation of cerebral circulation is disrupted, and there is an increasing dependence on the state of systemic hemodynamics, which also turns out to be unstable due to the same diseases of the cardiovascular system. Added to this are disturbances in the neurogenic regulation of systemic and cerebral hemodynamics. Brain hypoxia itself leads to further damage to the mechanisms of autoregulation of cerebral circulation. The pathogenetic mechanisms of acute and chronic cerebral ischemia have much in common. The main pathogenetic mechanisms of cerebral ischemia constitute the “ischemic cascade” (V.I. Skvortsova, 2000), which includes:
- decreased cerebral blood flow;
- increase in glutamate excitotoxicity;
- calcium accumulation and lactic acidosis;
- activation of intracellular enzymes;
- activation of local and systemic proteolysis;
- emergence and progression of antioxidant stress;
- expression of early response genes with the development of depression of plastic proteins and a decrease in energy processes;
- long-term consequences of ischemia (local inflammatory reaction, microcirculatory disorders, damage to the BBB).
A condition called “oxidative stress” plays a major role in damage to brain neurons. Oxidative stress is an excessive intracellular accumulation of free radicals, activation of lipid peroxidation (LPO) processes and excessive accumulation of lipid peroxidation products, aggravating overexcitation of glutamate receptors and enhancing glutamate excitoxic effects. Glutamate excitotoxicity is understood as hyperstimulation by mediators of excitation of NDMA receptors of N-methyl-D-aspartate, provoking dilatation of calcium channels and, as a consequence, massive influx of calcium into cells, with subsequent activation of proteases and phospholipases. This leads to a gradual decrease in neuronal activity, a change in the neuron-glia ratio, which causes a deterioration in brain metabolism. Understanding the pathogenesis of CCI is necessary for an adequate, optimally selected treatment strategy.
As the severity of the clinical picture increases, pathological changes in the vascular system of the brain intensify. If at the beginning of the process stenotic changes in one or two main vessels are detected, then most or even all of the main arteries of the head turn out to be significantly changed. Moreover, the clinical picture is not identical to damage to the great vessels, due to the presence in patients of compensatory mechanisms of autoregulation of cerebral blood flow. The condition of intracranial vessels plays an important role in the mechanisms of compensation for cerebral circulatory disorders. With well-developed and preserved collateral circulation pathways, satisfactory compensation is possible, even with significant damage to several great vessels. On the contrary, individual structural features of the cerebral vascular system may be the cause of decompensation (clinical or subclinical), aggravating the clinical picture. This may explain the more severe clinical course of cerebral ischemia in middle-aged patients.
Based on the main clinical syndrome, several forms of CCI are distinguished: with diffuse cerebrovascular insufficiency; predominant pathology of the vessels of the carotid or vertebrobasilar systems; vegetative-vascular paroxysms; predominant mental disorders. All forms have similar clinical manifestations. In the initial stages of the disease, all patients complain of headache, non-systemic dizziness, noise in the head, memory impairment, and decreased mental performance. As a rule, these symptoms occur during a period of significant emotional and mental stress, requiring a significant increase in cerebral circulation. If two or more of these symptoms are often repeated or exist for a long time (at least the last 3 months) and there are no signs of an organic nature, instability when walking, or damage to the nervous system, a presumptive diagnosis is made.
The clinical picture of CCI has a progressive development and, according to the severity of symptoms, is divided into three stages: initial manifestations, subcompensation and decompensation.
Stage 1 is dominated by subjective disorders in the form of headaches and a feeling of heaviness in the head, general weakness, increased fatigue, emotional lability, dizziness, decreased memory and attention, and sleep disturbances. These phenomena are accompanied, although mild, but quite persistent objective disorders in the form of anisoreflexia, discoordination phenomena, oculomotor insufficiency, symptoms of oral automatism, memory loss and asthenia. At this stage, as a rule, the formation of distinct neurological syndromes (except for asthenic) has not yet occurred, and with adequate therapy, it is possible to reduce the severity or eliminate both individual symptoms and the disease as a whole.
The complaints of patients with the 2nd stage of CCI more often include memory impairment, loss of ability to work, dizziness, instability when walking, and manifestations of an asthenic symptom complex are less often present. At the same time, focal symptoms become more distinct: revival of reflexes of oral automatism, central insufficiency of the facial and hypoglossal nerves, coordination and oculomotor disorders, pyramidal insufficiency, amyostatic syndrome, increased mnestic-intellectual disorders. At this stage, it is possible to identify certain dominant neurological syndromes - discoordination, pyramidal, amyostatic, dysmnestic, etc., which can help in prescribing symptomatic treatment.
At the 3rd stage of CCI, objective neurological disorders in the form of discoordination, pyramidal, pseudobulbar, amyostatic, and psychoorganic syndromes are more pronounced. Paroxysmal conditions—falls, fainting—are more common. In the stage of decompensation, cerebral circulation disorders are possible in the form of “small strokes” or prolonged reversible ischemic neurological deficit, the duration of focal disorders in which ranges from 24 hours to 2 weeks. At the same time, the clinical picture of diffuse insufficiency of blood supply to the brain corresponds to that of moderate encephalopathy. Another manifestation of decompensation may be a progressive “complete stroke” and residual effects after it. This stage of the process with diffuse damage corresponds to the clinical picture of severe encephalopathy. Focal symptoms are often combined with diffuse manifestations of brain failure.
In chronic cerebral ischemia, there is a clear correlation between the severity of neurological symptoms and the age of the patients. This must be kept in mind when assessing the significance of individual neurological signs that are considered normal for elderly and senile people. This dependence reflects age-related manifestations of dysfunction of the cardiovascular and other visceral systems, affecting the state and functions of the brain. To a lesser extent, this dependence is observed in hypertensive encephalopathy. In this case, the severity of the clinical picture is largely determined by the course of the underlying disease and its duration.
Along with the progression of neurological symptoms, as the pathological process develops in the neurons of the brain, an increase in cognitive disorders occurs. This applies not only to memory and intelligence, which are impaired in the 3rd stage to the level of dementia, but also to such neuropsychological syndromes as praxis and gnosis. Initial, essentially subclinical disorders of these functions are observed already in the 1st stage, then they intensify, change, and become distinct. The 2nd and especially the 3rd stages of the disease are characterized by pronounced impairments of higher brain functions, which sharply reduces the quality of life and social adaptation of patients.
In the picture of CIM, several main clinical syndromes are distinguished: cephalgic, vestibulo-ataxic, pyramidal, amyostatic, pseudobulbar, paroxysmal, vegetative-vascular, psychopathological. A feature of the cephalgic syndrome is its polymorphism, inconstancy, lack of connection in most cases with specific vascular and hemodynamic factors (excluding headaches during hypertensive crises with high blood pressure), and a decrease in the frequency of occurrence as the disease progresses.
The second most common syndrome is vestibulo-ataxic syndrome. The main complaints of patients are: dizziness, instability when walking, coordination disorders. Sometimes, especially in the initial stages, patients, complaining of dizziness, do not notice coordination problems. The results of otoneurological examination are also insufficiently indicative. In later stages of the disease, subjective and objective discoordination disorders are clearly interrelated. Dizziness and unsteadiness when walking may be partly due to age-related changes in the vestibular apparatus, motor system and ischemic neuropathy of the vestibulocochlear nerve. Therefore, to assess the significance of subjective vestibulo-ataxic disorders, their qualitative analysis during a patient interview, neurological and otoneurological examination is important. In most cases, these disorders are caused by chronic circulatory failure in the blood supply of the vertebrobasilar arterial system, so it is necessary to rely not on the subjective sensations of patients, but to look for signs of diffuse damage to the parts of the brain that are supplied with blood from this vascular system. In some cases, in patients with stages 2–3 CCI, ataxic disorders are caused not so much by cerebellar-stem dysfunction, but rather by damage to the frontal-stem pathways. There is a phenomenon of frontal ataxia, or apraxia of walking, reminiscent of hypokinesia in patients with parkinsonism. A CT examination reveals significant hydrocephalus (along with cortical atrophy), i.e., a condition similar to normal pressure hydrocephalus occurs. In general, the syndrome of circulatory failure in the vertebrobasilar system is diagnosed with CCI more often than insufficiency of the carotid system.
A feature of the pyramidal syndrome is its moderate clinical manifestation (anisoreflexia, facial asymmetry, minimally expressed paresis, revitalization of oral automatism reflexes, hand symptoms). A clear asymmetry of reflexes indicates either a previously existing cerebral stroke or another disease occurring under the guise of CCI (for example, large intracranial processes, consequences of traumatic brain injury). Diffuse and fairly symmetrical revival of deep reflexes, as well as pathological pyramidal reflexes, often combined with a significant revival of oral automatism reflexes and the development of pseudobulbar syndrome, especially in old age, indicates multifocal vascular damage to the brain (subject to the exclusion of other possible causes).
In patients with clinical manifestations of circulatory failure in the vertebrobasilar system, paroxysmal conditions are often observed. These conditions may be caused by a combined or isolated effect on the vertebral arteries of vertebrogenic factors (compression, reflex), which is associated with changes in the cervical spine (dorsopathies, osteoarthritis, deformities).
Mental disorders are quite characteristic and varied in form at different stages of CCI. If in the initial stages they are of the nature of asthenic, asthenodepressive and anxiety-depressive disorders, then in the 2nd and especially in the 3rd stage they are joined by pronounced dysmnestic and intellectual disorders, forming the syndrome of vascular dementia, which often comes first in the clinical picture .
Electroencephalographic changes are nonspecific for CCI. They consist of a progressive decrease in the β-rhythm, an increase in the proportion of slow θ- and δ-activity, accentuation of interhemispheric asymmetry, and a decrease in EEG reactivity to external stimulation.
CT characteristics undergo dynamics from normal indicators or minimal atrophic signs in the 1st stage to more pronounced small-focal changes in the brain substance and atrophic (external and internal) manifestations in the 2nd stage to sharply defined cortical atrophy and hydrocephalus with multiple hypodense foci in the hemispheres - in the 3rd stage.
A comparison of clinical and instrumental characteristics in patients with atherosclerotic, hypertensive and mixed forms of CCI does not reveal any clear differences. In severe cases of hypertension, a faster rate of increase in psychoneurological disorders, early manifestation of cerebral disorders, and a greater likelihood of developing lacunar stroke are possible.
Treatment of CCI should be based on certain criteria, including the concepts of pathogenetic and symptomatic therapy. To correctly determine the pathogenetic treatment strategy, one should take into account: the stage of the disease; identified mechanisms of pathogenesis; the presence of concomitant diseases and somatic complications; age and gender of patients; the need to restore quantitative and qualitative indicators of cerebral blood flow, normalize impaired brain functions; the possibility of preventing recurrent cerebral dysgemia.
The most important direction of CCI therapy is the impact on existing risk factors, such as arterial hypertension and atherosclerosis. Treatment of atherosclerosis is carried out according to generally accepted regimens using statins, in combination with correction of the diet and lifestyle of patients. The selection of antihypertensive drugs and the order of their prescription is carried out by a general practitioner, taking into account the individual characteristics of patients. Complex therapy for CCI includes the prescription of antioxidants, antiplatelet agents, drugs that optimize brain metabolism, and vasoactive drugs. Antidepressants are prescribed for severe asthenodepressive manifestations of the disease. Antiasthenic drugs are prescribed in the same way.
An important component of the treatment of CCI is the administration of drugs with antioxidant activity. Currently, the following drugs of this series are used in clinical practice: Actovegin, Mexidol, Mildronate.
Actovegin is a modern antioxidant, which is a deproteinized extract of the blood of young calves. Its main effect is to improve the utilization of oxygen and glucose. Under the influence of the drug, the diffusion of oxygen in neuronal structures significantly improves, which makes it possible to reduce the severity of secondary trophic disorders. There is also a significant improvement in cerebral and peripheral microcirculation against the background of improved aerobic energy exchange of vascular walls and the release of prostacyclin and nitric oxide. The resulting vasodilation and decrease in peripheral resistance are secondary to the activation of oxygen metabolism of the vascular walls (A. I. Fedin, S. A. Rumyantseva, 2002).
In case of CCI, it is advisable to use Actovegin, especially in the absence of effect from other treatment methods (E. G. Dubenko, 2002). The method of application consists of drip administration of 600–800 mg of the drug for 10 days, followed by switching to oral administration.
A constant in the treatment regimen for CCI is the use of drugs that optimize cerebral circulation. The most commonly used drugs are: Cavinton, Halidor, Trental, Instenon.
Halidor (bencyclane) is a drug that has a multidirectional mechanism of action due to phosphodiesterase blockade, antiserotonin action, and calcium antagonism. It inhibits the aggregation and adhesion of platelets, prevents the aggregation and adhesion of erythrocytes, increasing the elasticity and osmotic resistance of the latter. Halidor reduces blood viscosity, normalizes intracellular metabolism of glucose and ATP, affects phosphokinase and lactate dehydrogenase, and enhances tissue oxygenation. It has been proven that the use of this drug for 8 weeks eliminates the clinical manifestations of chronic cerebral vascular insufficiency in 86% of patients. The drug has a positive effect on a person’s emotional environment, reduces forgetfulness and absent-mindedness. Halidor is prescribed in a daily dose of 400 mg for 6–8 weeks.
Instenon is a combined drug with neuroprotective action, including a vasoactive agent from the group of purine derivatives, a substance that affects the state of the ascending reticular formation and cortical-subcortical relationships, and, finally, an activator of tissue respiration processes under hypoxic conditions (S. A. Rumyantseva, 2002; B V. Kovalchuk, 2002).
The three components of instenon (etophylline, etamivan, hexobendine) jointly act on various parts of the pathogenesis of ischemic brain damage.
Etophylline, a vasoactive component of the purine series, activates myocardial metabolism with an increase in stroke volume. The transition from a hypokinetic type of blood circulation to a normokinetic one is accompanied by an increase in cerebral blood flow. An important effect of the component is an increase in renal blood flow and, as a consequence, dehydration and diuretic effects.
Etamivan has a nootropic effect in the form of a direct effect on the processes of memory, attention, mental and physical performance as a result of increased activity of the reticular formation of the brain.
Hexobendine selectively stimulates metabolism based on increased utilization of oxygen and glucose, due to increased anaerobic glycolysis and pentose cycles. At the same time, the physiological mechanisms of autoregulation of cerebral and systemic blood flow are stabilized.
Instenon is used intramuscularly 2.0 ml, course - 5-10 procedures. Then oral administration of instenon-forte continues, 1 tablet 3 times a day for a month (S. V. Kotov, I. G. Rudakova, E. V. Isakova, 2003). A clear regression of neurological symptoms is observed by the 15th–20th day of treatment. A particularly good effect is observed with the combined use of Actovegin (drops) and instenon (intramuscular injections or oral administration). Instenon therapy has a positive effect on cognitive functions, especially on the regulation of mnestic activity and psychomotor functions.
In the complex therapy of CCI, much attention is paid to nootropic drugs that increase the resistance of brain tissue to various adverse metabolic influences (ischemia, hypoxia). The actual “nootropic” drugs include derivatives of piracetam (nootropil, lutetam), encephabol.
Piracetam increases the synthesis of high-energy phosphates (ATP), enhances aerobic metabolism under hypoxic conditions, facilitates impulse conduction, normalizes the ratio of phospholipids of cell membranes and their permeability, increases the density and sensitivity of receptors, improves interaction between the cerebral hemispheres, improves metabolic processes in the central nervous system, facilitates neuronal transfer.
Piracetam improves microcirculation due to its disaggregant properties, facilitates the conduction of nerve impulses, and improves interaction between the hemispheres of the brain. The drug normalizes the ratio of phospholipids of cell membranes and increases their permeability, prevents the adhesion of red blood cells, reduces platelet aggregation, reduces the levels of fibrinogen and factor VIII, and relieves spasm of arterioles. The drug is prescribed in a daily dose of 2.4–4.8 g for 8–12 weeks.
Encephabol is a derivative of pyritinol. The drug increases the density and sensitivity of receptors, normalizes neuroplasticity. It has a neuroprotective effect, stimulates learning processes, improves memory, memorization and concentration. Encephabol stabilizes the cell membranes of neurons by inhibiting lysosomal enzymes and preventing the formation of free radicals, improves the rheological properties of blood, increases the conformational ability of red blood cells, increasing the ATP content in their membrane. For adults, the average daily dose is 600 mg for 6–8 weeks.
Antiplatelet drugs include acetylsalicylic acid and its derivatives (cardiomagnyl, thrombo ACC). Given the presence of contraindications when prescribing acetylsalicylic acid, other drugs with antiplatelet activity (Curantil, Tiklid, Plavix) are often used.
Symptomatic therapy for CCI includes the prescription of drugs that reduce the manifestations of various symptoms of the disease. For all patients with stages 2–3 of the disease, it is advisable to prescribe anti-anxiety or antidepressant drugs. Benzodiazepine drugs are the safest for long-term use.
Grandaxin is an atypical benzodiazepine derivative, a selective anxiolytic. The drug effectively eliminates anxiety, fear, and emotional stress without sedation or muscle relaxation. The drug has a vegetative-corrective effect, which makes it possible to use it in patients with severe vegetative-vascular syndrome.
In neurological practice, a daily dose of 50–100 mg is used, the duration of use is determined individually for each patient.
The prevalence of chronic vascular pathology of the brain, the progression of its course, and the high degree of disability of patients determine the social and medical significance of the problem of CCI therapy. Currently, in clinical practice there is a trend towards increasing the use of non-drug treatment methods. This is due to the absence in patients of the phenomenon of addiction to medicinal substances with a long period of therapeutic aftereffect.
Considering the complexity of the pathogenetic mechanisms of CCI, during therapy it is necessary to achieve normalization of systemic and cerebral circulation, adjust the metabolism in the brain tissue, and the state of hemorheology. Currently, the possibilities for pharmacological correction of the manifestations of CCI are quite extensive; they allow the use of various drugs that affect all parts of the pathogenesis of post-ischemic and post-hypoxic damage to nervous tissue.
Thus, recognizing the causes, identifying risk factors and, therefore, the real possibility of effective targeted treatment and preventing the development of chronic cerebral vascular pathology requires accurate knowledge of the structural, physiological and clinical features of the manifestation of the disease. This becomes possible thanks to a systematic approach to the study of etiology, pathogenesis, clinical picture and modern methods of therapy.
M. V. Putilina , Doctor of Medical Sciences, Professor
RGMU, Moscow
Dyscirculatory-dystrophic changes in the brain
- Diffuse. The pathology affects all brain tissue evenly; specific local lesions are not formed.
- Focal. Often appear against the background of impaired blood supply. With focal changes, the brain as a whole is not damaged, but individual foci are observed affecting sections and areas of the brain.
Also, discirculatory dystrophy is of the following types:
- atherosclerotic (due to the presence of plaques obstructing blood flow);
- hypertensive;
- venous;
- mixed.
The disease leads to the following consequences:
- Rarefaction of areas of brain tissue: it seems to become loose, like a washcloth.
- Asymptomatic cerebral infarction is an acute disorder of cerebral circulation that has no clinical manifestations and does not give symptoms of neurological disorders.
- Stroke.