Rheumatoid arthritis is a chronic systemic disease of connective tissue with predominant damage to peripheral (synovial) joints of the type destructive-erosive polyarthritis. Seronegative rheumatoid arthritis has ICD code No. M05.8, seronegative rheumatoid arthritis – M06.0. Probable rheumatoid arthritis in the ICD is defined with codes M05.9, M06.4, M06.9. Rheumatologists at the Yusupov Hospital, using the latest research methods, establish an accurate diagnosis and promptly prescribe adequate treatment.
To avoid unnecessary examinations, adhere to the following tactics:
- The true localization of the lesion is clarified (joint or periarticular structures);
- The nature of the lesion is determined (the predominance of the inflammatory or degenerative process);
- Determine the extent of the lesion (local, limited or generalized);
- Carry out differential diagnosis.
Doctors solve these diagnostic problems before settling on a diagnosis of rheumatoid arthritis. During treatment, patients are kept in rooms with a European level of comfort. They are provided with dietary food and individual personal hygiene products. Severe cases of rheumatoid arthritis are discussed at a meeting of the Expert Council. Candidates and doctors of medical sciences, doctors of the highest category take part in its work. Leading specialists collectively develop patient management tactics.
I34 Non-rheumatic lesions of the mitral valve
Excludes: mitral (valve): disease (I05.9), insufficiency (I05.8), stenosis (I05.0), lesions specified as rheumatic (I05.), with an unknown cause, but with mention of: aortic valve disease (I08.0), mitral stenosis or obstruction (I05.0)
I34.0 Mitral (valve) insufficiency
I34.1 Prolapse (prolapse) of the mitral valve
Excludes: Marfan syndrome (Q87.4)
I34.2 Non-rheumatic mitral valve stenosis
I34.8 Other non-rheumatic lesions of the mitral valve
I34.9 Non-rheumatic disease of the mitral valve, unspecified
I08 Lesions of several valves
Included: cases specified or unspecified as rheumatic
Excluded:
rheumatic diseases of the endocardium, valve unspecified (I09.1)
endocarditis, valve unspecified (I38)
I08.0 Combined lesions of the mitral and aortic valves
I08.1 Combined lesions of the mitral and tricuspid valves -
new
I08.2 Combined lesions of the aortic and tricuspid valves
new
I08.3 Combined lesions of the mitral, aortic and tricuspid
chat valves
I08.8 Other multiple valve diseases
I08.9 Multiple valve lesions, unspecified
Classification
According to this international classification, ICD 10 code lists all existing heart defects.
There are quite a few of them. Conventionally, all defects can be divided into two groups, each of which has its own subgroups:
- White. Heart diseases in which mixing of venous and arterial blood does not occur.
- defect of the interatrial and interventricular septum;
- pathologies caused by depletion of the pulmonary circulation;
- defects associated with depletion of the systemic circulation;
- pathologies not associated with hemodynamic disorders.
- Blue. Venous and arterial blood mix.
- defects caused by enrichment of the small circle;
- pathologies caused by depletion of the small circle.
Each of the above groups and subgroups has its own specific code, which helps to determine the type of disease as accurately as possible.
Symptoms
When diagnosing congenital heart disease, the pediatrician and cardiologist must first conduct a conversation with the child’s parents.
In this conversation, it is necessary to establish how the child developed, when the first signs of the defect began to appear, etc. A congenital defect leaves its mark not only on the functioning of the heart, but also on many other signs:
- Body type. Few defects can cause changes in physique. For example, if the functioning of the aorta of the heart is impaired, the child experiences accelerated development of the shoulder girdle. As a rule, such children do not gain weight well, and this is reflected in their physique.
- Covers of the skin. If a patient is diagnosed with a white type defect, his skin is too pale. With a blue defect, cyanosis of the integument is clearly manifested.
- Respiratory system. Due to increased blood flow in the lungs, patients with congenital heart disease often suffer from shortness of breath and have difficulty breathing.
- Digestive organs. The disease also affects the digestive system. For example, there is an increase in the size of the liver. Often, such patients experience vomiting with increased physical activity, which is accompanied by severe pain in the abdominal area.
All these symptoms can appear from an early age, or they can begin to remind themselves at the age of 5–6 years.
Instrumental diagnosis of rheumatoid arthritis
Instrumental research methods are not included in the criteria for the diagnosis of rheumatoid arthritis, but are widely used for the following purposes:
- To identify early structural damage, which allows you to clarify the diagnosis in cases where the assessment according to the criteria does not give clear results;
- To verify the diagnosis at a late stage of the disease, when the activity of the inflammatory process may spontaneously decrease and the phenomena of destruction of osteochondral tissue predominate;
- To monitor response to therapy;
- To assess the rate of progression of structural damage;
- To verify structural disorders before orthopedic surgical treatment and orthosis.
To confirm the diagnosis, establish the stage and assess the progression of destruction, plain radiographs of the hands and distal feet are performed at the Yusupov Hospital. X-rays of large joints are not used as a routine method and are performed only if there are specific indications (suspicion of avascular necrosis). Chest X-ray is done in all patients to identify rheumatoid lesions of the respiratory system and concomitant lesions of the lungs. Computed tomography of the lungs is prescribed if there is a clinical suspicion of diffuse or focal lung damage associated with rheumatoid arthritis, a disease of the chest organs that may cause joint damage, or concomitant pathology that may affect the choice of therapy.
Magnetic resonance imaging is a more sensitive method for detecting synovitis at the onset of rheumatoid arthritis than standard joint radiography. An ultrasound examination of the hand joints and large joints is performed. Based on its results, doctors evaluate the following indicators:
- Thickening of the synovium;
- Presence of effusion in the joint;
- Violation of the contour of the articular surface (corresponds to erosion);
- Changes in periarticular tissues (tenosynovitis).
With a power Doppler study, the localization, extent and intensity of the signal make it possible to judge the severity of proliferative inflammation.
Diagnostics
The more methods were used to diagnose congenital heart disease code according to ICD 10, the more accurate and detailed the picture of the disease will be visible.
The following methods are used for diagnosis:
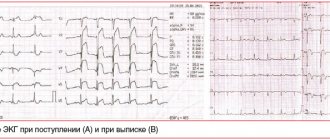
- Electrocardiogram. This method gives excellent results, even in the initial stages of pathology development. Based on the interpretation of the cardiogram results, the cardiologist can accurately determine the intensity of the development of the disease and its danger to the child’s life.
- X-ray. When conducting an X-ray examination in 3 projections, the condition of the lungs and the entire respiratory system can be determined.
- Echocardiography. Allows the cardiologist to obtain the most accurate picture of the patient’s condition.
- Angiography or catheterization. These techniques are more difficult to perform, but they allow you to determine the pressure in the lungs, as well as accurately determine in which direction the blood flow is directed (from the right atrium to the left or vice versa).
All of the above diagnostic methods are used in combination.
Only in this case can an accurate diagnosis be established and an effective course of treatment be chosen. Regardless of whether the defect is congenital or acquired, you must be attentive to your health and the health of your loved ones; if one or more signs appear, immediately contact a pediatrician and cardiologist. Be healthy!
Reasons for development
Factors that can provoke the birth of a child with a congenital pathology of the development and functioning of the heart can be divided into two large groups:
- Genetic. In this case, we are talking about point gene changes or specific chromosome mutations.
- Ecological. This group includes quite a few factors. Among the main ones are the influence of ion radiation on a pregnant woman and her contact with pesticides. Smoking and drinking alcoholic beverages also fall into this group. If a woman has suffered any infectious or viral diseases during pregnancy, they can also provoke the development of congenital heart disease in the child.
Often the factors that lead to heart pathology can be combined.
Causes and mechanisms of development of rheumatoid arthritis
For what reasons rheumatoid arthritis develops, scientists have not yet established. The disease is so common that it was given a separate chapter in the ICD. The following factors are believed to cause rheumatoid arthritis:
- Compounded heredity – a tendency to autoimmune diseases in the family, the presence of a certain class of histocompatibility antibodies;
- Past infectious diseases (measles, mumps, respiratory syncytial infection, hepatitis B, herpes viruses of all types (cytomegalovirus), retroviruses, Epstein-Barr);
- Hypothermia, intoxication, stress, hormonal imbalances, some medications.
The vessels of the synovial membrane react to the appearance of an unknown antigen and its processing by macrophages. Vascular permeability increases, activated formed elements (T-lymphocytes) leave the vascular bed. This is accompanied by an increase in cytokinins - substances of intercellular interaction. In rheumatoid arthritis, many cytokines with pro-inflammatory, destructive effects are produced:
- Tumor necrosis factor-a (TNF-a;
- Interleukin-1 (IL-1);
- Interleukin-6 (IL-6);
- Interferon-g (IF-g).
The production of cytokines ensures the directed movement and attraction of new formed elements into the subsynovial tissue, which form mixed T-B-cell lymphocytic infiltrates. B lymphocytes, through transformation into plasma cells, provide the synthesis of antibodies to their own aggregated g-globulin. Neutrophils phagocytize rheumatoid arthritis factors that have entered the synovial fluid. They can be absorbed by macrophages.
The processes of cellular interaction and phagocytosis in adjacent structures and synovial fluid are accompanied by cell destruction. There is a release of a large number of biologically active substances - cytokines, prostaglandins, metalloproteinases. They support inflammation and destruction of joint tissue.
Ultimately, the proliferation of synovial tissue, capillary network and collagen formation occurs. The joint cavity decreases. The resulting granulation tissue destroys the cartilage and “grows” into the subchondral bone, destroying it. This is radiologically manifested by bone erosions. Replacement of the normal components of the joint with a newly formed connective tissue structure leads to its deformation and dysfunction.
Symptoms
When diagnosing congenital heart disease, the pediatrician and cardiologist must first conduct a conversation with the child’s parents.
In this conversation, it is necessary to establish how the child developed, when the first signs of the defect began to appear, etc. A congenital defect leaves its mark not only on the functioning of the heart, but also on many other signs:
- Body type. Few defects can cause changes in physique. For example, if the functioning of the aorta of the heart is impaired, the child experiences accelerated development of the shoulder girdle. As a rule, such children do not gain weight well, and this is reflected in their physique.
- Covers of the skin. If a patient is diagnosed with a white type defect, his skin is too pale. With a blue defect, cyanosis of the integument is clearly manifested.
- Respiratory system. Due to increased blood flow in the lungs, patients with congenital heart disease often suffer from shortness of breath and have difficulty breathing.
- Digestive organs. The disease also affects the digestive system. For example, there is an increase in the size of the liver. Often, such patients experience vomiting with increased physical activity, which is accompanied by severe pain in the abdominal area.
All these symptoms can appear from an early age, or they can begin to remind themselves at the age of 5–6 years.
Diagnostics
The more methods were used to diagnose congenital heart disease code according to ICD 10, the more accurate and detailed the picture of the disease will be visible.
The following methods are used for diagnosis:
- Electrocardiogram. This method gives excellent results, even in the initial stages of pathology development. Based on the interpretation of the cardiogram results, the cardiologist can accurately determine the intensity of the development of the disease and its danger to the child’s life.
- X-ray. When conducting an X-ray examination in 3 projections, the condition of the lungs and the entire respiratory system can be determined.
- Echocardiography. Allows the cardiologist to obtain the most accurate picture of the patient’s condition.
- Angiography or catheterization. These techniques are more difficult to perform, but they allow you to determine the pressure in the lungs, as well as accurately determine in which direction the blood flow is directed (from the right atrium to the left or vice versa).
All of the above diagnostic methods are used in combination.
Only in this case can an accurate diagnosis be established and an effective course of treatment be chosen. Regardless of whether the defect is congenital or acquired, you must be attentive to your health and the health of your loved ones; if one or more signs appear, immediately contact a pediatrician and cardiologist. Be healthy!
Diagnosis of rheumatoid arthritis
The American College of Rheumatology has adopted the following diagnostic criteria for rheumatoid arthritis:
- Morning joint stiffness that lasts an hour before disappearing or significantly improving;
- Arthritis of three or more joint areas. The doctor must note the presence of swelling in three of the seven joint zones - the proximal interphalangeal joints of the hands, metacarpophalangeal, wrist, elbow, knee, ankle, metatarsophalangeal joints;
- Arthritis of the joints of the hand, which manifests itself as swelling in one of the three articular zones of the hands (proximal interphalangeal, metacarpophalangeal, wrist joints);
- Symmetrical arthritis (absolute symmetry in the interphalangeal joints is not required);
- Rheumatoid nodules located under the skin on the extensor surface of the elbow and interphalangeal joints of the hands. They have a densely elastic consistency, are sometimes fused to the periosteum, can increase or decrease and even disappear during the course of the disease, depending on the activity of the pathological process;
- Detection of rheumatoid factor in blood serum;
- The presence of radiological signs in the form of obvious bone decalcification - bone erosions on direct radiographs of the wrist joints and hands.
In order to make a diagnosis of rheumatoid arthritis, four criteria must be met. If the first 4 criteria are used, their duration must be at least six weeks. It is not easy to diagnose rheumatoid arthritis at an early stage. For several months, doctors only suspected the presence of the disease, actually dealing with “undifferentiated arthritis” (ICD10 code No. M13.1). The term “early rheumatoid arthritis” means that the duration of the process does not exceed 12 months.
In a patient who complains of joint pain, the following symptoms can be suspected of rheumatoid arthritis, according to the criteria of the European League Against Rheumatism:
- The presence of three or more swollen joints;
- Symmetrical damage to the metatarsophalangeal and metacarpophalangeal joints (determined by a positive “lateral compression” test);
- Morning stiffness that lasts more than 30 minutes.
These clinical signs are more significant if they occur against the background of an increase in erythrocyte sedimentation rate.