Why do an ECG for a child?
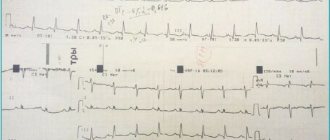
Electrocardiography (ECG) is a diagnostic method based on recording and studying electrical impulses generated during the work of the heart. Special sensors are connected to the patient's body, which record electrical impulses and record the received data in the form of teeth on paper film. The resulting cardiogram allows the specialist to obtain information about the electrical activity of the heart and the structure of the myocardium. This, in turn, allows us to identify malfunctions in the cardiovascular system, make an accurate diagnosis and prescribe the correct treatment, taking into account the individual characteristics of the patient.
ECG is one of the simplest, most accessible and informative methods for diagnosing heart disease. The method is absolutely safe, so it can be used in both adults and children. An ECG is prescribed to a child both if there is a suspicion of heart pathologies and as a preventive examination.
An ECG can reveal:
- disturbance of the rhythm of heart rate (arrhythmia);
- tachycardia;
- organic changes in the heart muscle;
- heart disease;
- metabolic disease;
- the presence of blockades that disrupt the conductivity of the electrical impulse;
- acute and chronic lung diseases;
- electrolyte and other changes in the myocardium;
- lack of potassium and magnesium;
- inflammatory processes in the myocardium;
- enlargement of individual parts of the organ.
Diseases of the cardiovascular system in children are not uncommon, so diagnosis should not be neglected. Detection of these diseases at an early age makes it possible to start treatment on time and minimize the risk of developing serious complications and prevent their negative impact on the growth and development of the child.
Archives
Short Wiklad
David F Dickinson Heart 2005;91:1626–1630.
Electrocardiogram (ECG) registration is an important element in the treatment of patients with various childhood illnesses, including those without clinical signs of heart disease. The basic principles of ECG interpretation in children and adults do not vary. Therefore, the progressive changes in anatomy and physiology that occur during the period from the time of birth to the subadult age, represent the specific features of the ECG that lie during the child’s age. Therefore, the correct interpretation of the ECG relies on the knowledge of changes that have been around for a long time, in order to identify errors that are detected in medicines and in the computer interpretation of the ECG.
Normal ranges of clinically variable 12-channel ECG changes at rest
P wave
The amplitude of the P wave in the child does not change at all. If anyone has an increased reading above 0.025 mV in II, the given trace can be seen as a shift between the norms. Voltage criteria for anterior hypertrophy need to stagnate only when sinus rhythm is preserved, if the entire P wave at the frontal plane lies at the intervals of 0–90°.
Q wave
The majority of the Q wave (II, III, aVF, V5, V6) tends to increase in amplitude over the first few months of life, with a maximum of approximately 3–5 years of age. and further changes to the output value. In the study by Rijnbeek (2001), the upper limit of the amplitude of the normal Q wave is substantially larger, compared to the lower limit in the earlier study by Davignon (1979) (Table 1). Also, the amplitude of the Q wave up to 0.6–0.8 mV lies in the normal range in children aged 6 months to 3 years.
The values in the Rijnbeek table are only for human patients, while those in the Davignon table are for both articles.
Table 1. Q wave amplitude in leads III and V6 according to the tables of Rijnbeek (2001) and Davignon (1979)
| Median for Rijnbeek (98% centile) | Median for Davignon (98% centile) | |||
| III | V6 | III | V6 | |
| 0–1 month | 0,15 (0,26) | 0,11 (0,22) | – | – |
| 1–3 months | 0,29 (0,50) | 0,16 (0,31) | 0,12 (0,55) | 0,03 (0,26) |
| 3–6 months | 0,31 (0,71) | 0,17 (0,35) | 0,13 (0,65) | 0,04 (0,26) |
| 6–12 months | 0,35 (0,79) | 0,20( 0,60) | 0,17 (0,6) | 0,04 (0,3) |
| 1–3 rocks | 0,30 (0,74) | 0,20 (0,56) | 0,13 (0,52) | 0,05 (0,3) |
| 3–5 rocks | 0,19 (0,46) | 0,15 (0,42) | 0,09 (0,40) | 0,07 (0,33) |
| 5–8 rocks | 0,15 (0,36) | 0,12 (0,39) | 0,09 (0,31) | 0,07 (0,45) |
| 8–12 rocks | 0,10 (0,28) | 0,12 (0,43) | 0,05 (0,28) | 0,06 (0,28) |
| 12–16 rocks | 0,10 (0,29) | 0,11 (0,43) | 0,04 (0,3) | 0,04 (0,28) |
QRS complex
The obvious hypertrophy of the right sac in newborns undergoes regression over the first few months of life. This is to change the QRS complex on the ECG. The entire QRS complex at the frontal plane in newborns at the middle becomes 60 to 160°. Over the course of the first years of life, you will need to change the axis, and from this point on, it will inevitably become around 65–70°, although you can vary from 0 to 110°. The amplitude of the R waves in the right thoracic abductors in healthy children changes with age, and in the left thoracic abductors it increases. Change the amplitude of the S wave to a similar or similar extent. The fluidity that comes with changes varies in different ways. In the average case, the R/S of the withdrawn V1 is lost >1 until the age of 3 years, and in healthy individuals - up to the age of 8–12 years. The absolute values of the amplitude of the R and S waves are larger in the studies of Macfarlane (1989) and Rijnbeek (2001) compared with Davignon (1979) (Table 2). For example, the upper boundary of the R wave in advanced V6 in the age group 12–16 years of age became 3.05 mV (Rijnbeek) compared to 2.3 mV (Davignon). However, in some regions, especially V4, the amplitude of the R wave was greater in the previous study.
Table 2. Amplitude of the R wave (mV) at leads V1 and V6, taken from the table of Rijnbeek and Davignon
| Median for Rijnbeek (98% centile) | Median for Davignon (98% centile) | |||
| V1 | V6 | V1 | V6 | |
| 0–1 month | 1,1 (2,05) | 1,0 (1,78) | – | – |
| 1–3 months | 1,23 (2,07) | 1,55 (2,23) | 0,9 (1,8) | 1,2 (2,15) |
| 3–6 months | 1,32 (2,20) | 1,65 (2,73) | 1,0 (2,0) | 1,3 (2,25) |
| 6–12 months | 1,12 (2,14) | 1,7 (2,79) | 0,9 (2,0) | 1,25 (2,25) |
| 1–3 rocks | 1,08 (2,11) | 1,79 (2,96) | 0,85 (1,75) | 1,3 (2,25) |
| 3–5 rocks | 0,95 (1,78) | 1,98 (3,14) | 0,8 (1,75) | 1,5 (2,5) |
| 5–8 rocks | 0,63 (1,48) | 1,97 (2,98) | 0,7 (1,4) | 1,65 (2,8) |
| 8–12 rocks | 0,54 (1,14) | 2,18 (3,24) | 0,5 (1,25) | 1,6 (2,5) |
| 12–16 rocks | 0,48 (1,18) | 2,02 (3,05) | 0,4 (1,0) | 1,5 (2,3) |
Compared with the gold standard - ECG ultrasound in children is a clearly uninformative method for diagnosing left sac hypertrophy, with low specificity and sensitivity. In a recently completed ECG study, criteria for left sac hypertrophy were evident in 15% of children with normal left sac mass on ultrasound follow-up (specificity 85%), while only 12 In 62 children with pathologically increased mass of the left sac, ECG criteria for hypertrophy were detected ( sensitivity 19.4%). Whose investigation has vikoristani normal standards for Davignon. There were no similar differences with normal values for Macfarlane or Rinjbeek. All this allows us to assume that the traditional amplitude criteria for myocardial hypertrophy in children will probably be revised and, if necessary, changed.
The values in the Rijnbeek table are only for human patients, while those in the Davignon table are for both articles.
T wave
In children, the configuration of the T wave is even more pronounced than in adults, especially in the chest. Beware of progressive changes in the axis of the tooth from the time of birth to early adulthood. The fluidity required for these changes may vary in some ways, otherwise it is possible to create customized songs.
In the first 2–3 days of life, positive T waves in the right thoracic abductors (V1 and V3R) are considered normal. During the first part of life, the T waves in these types of teeth are less likely to invert. Looking at the fact that progressive changes in the T wave in the neonatal period occurred in a small number of patients, it is impossible to indicate the exact age in which positive T wave can be seen as a pathology; However, in the Davignon study, the amplitude of the T wave at the 98% centile was positive in the period 0–7 days and negative in the period 7–30 days. Therefore, if a positive T wave persists in leads V1 or V3R after the first life of life, it is necessary to suspect the presence of pathology. The T wave becomes inverted in most children before they reach 12–16 years of age.
In the intermediate adductions V2 and V3, the T wave often inverts in early childhood and progresses to a positive T wave in the successive adductions V3, V2, V1. It was found that in 50% of healthy children in the 3-5 age group there are inverted T waves in the V2 lead, while in the 8-12 age group there are inverted T waves in the V2 lead higher in 5–10% quilting.
The T wave in V5 and V6 is responsible for being positive in all age groups; In a very small number of newborns, the T wave in these cases may be flattened or inverted for 1–3 days.
Rehabilitation in sinus rhythm
Carrying out ambulatory ECG monitoring in healthy children and children of all age groups showed that the correct sinus rhythm can sometimes be interrupted by various variations in the rhythm, which in the early stages can become pathological. To increase the frequency of these changes, it is important to maintain a reasonable range of normal heart rate in children and to establish a relationship between symptoms and changes in heart rate when special conditions are observed. The songs change the heart rhythm and become wider. The stench comes out of a lot of blankets, although not very often. Most types of rhythm disturbances with high composure are likely to be completely benign. However, this assumption was not confirmed by any prospective trial study.
Change the PP interval
Phase changes in the PP interval may also apply to children. If the stench is even obvious, it creates anxiety due to the presence of an irregular heart rhythm. In most episodes, the diagnosis of sinus arrhythmia is easily confirmed by establishing a connection with the phases of breathing (sooner with the hour of sight, quicker with inhalation).
Increase the width (in 50% of newborns) around the PP interval during rapt periods. In older children, the frequency of such episodes changes (in children - up to 16%). Although such sinus pauses are avoided in many cases, they occur infrequently (2–3 in 24 years) and sometimes only in isolated cardiac cycles. In both newborns and older children, the length of the longest recorded pauses did not exceed 1.8–1.9 seconds. In case of sinus arrhythmia in rich children, it is not easy to measure the disturbance of the sinus cycle at rest; in most cases, the exact mechanism of these pauses becomes unimportant. The stench may correspond to the characteristics of sinoatrial block or sinus node nodes, but without direct recording of sinus node potentials, an accurate diagnosis cannot be made. Regardless of the precise mechanism, it is clear that the indicated pauses are wider for any person. Although sickness of the sinus node disappears in small children and can lead to syncope, in the vast majority of children the sinus pause is good.
Change the morphology of the P wave and the PR interval
Changes in the morphology of the P wave, associated with changes in heart rate and changes in the PR interval, occur in 20–30% of speechless children. Such episodes of the junctional rhythm primarily occur after the step-by-step synchronization of the frequency of the sinus rhythm during the hour of sleep, and may also occur during the active period. Most episodes are short, lasting no more than a few seconds or up to about one hour. Whenever you record disturbing episodes, they last for many years. Frequently falling asleep before an hour of sleep over the course of many years, often untouched episodes are recorded.
The PR interval on a 12-channel ECG at rest varies in children, which is important to the heart rate. Therefore, the discomfort is less in young children. In humans, with a heart rate of 100–150 per month, the PR interval is in the range of 80–110 ms, in other cases – up to 150 ms. In children whose heart rate is very low, the upper limit of the norm is approximately 180 ms. Ambulatory ECG monitoring shows that in all age groups, in individuals with a normal PR interval, quiet periods are avoided when the PR interval increases to more than 200 ms. Zokrem, such features were revealed in 8–12% of children aged 10–16 years. Episodes of first-stage AV block were greater during the hour of sleep, and their duration varied from several seconds to many years. In some individuals, first-stage AV block is a great relief from calm.
| Increased changes in heart rate that can be normal: • Virase sinus arrhythmia • Short sinus pauses lasting less than 1.8 seconds • First stage AV block • AV blockade of another stage type Mobitz 1 • Woozles rhythm • Slunic or supraventricular extrasystoles |
Approximately 10% of healthy children show episodes of AV block of another stage, Mobitz type 1 (Wenckebach period). Some, but not all, individuals have obvious episodes of first-stage AV block. The number of episodes can increase from individual isolates to hundreds in 24 years. In some patients, AV block is maintained for a few seconds after the first Wenckebach sequence with a 2:1 ratio. It is very rare to detect progression of Mobitz type 1 AV block to complete AV block. This progression is even more unexpected, so it is recommended to achieve frequent blockade of Mobitz 1 in healthy asymptomatic children.
In subjects who undergo intense physical training, changes in the PR interval appear to occur more frequently during episodes of first-stage and other-stage type 1 AV blockade. 20% padded.
Extrasystoles
Isolated sulcular shortness can be recorded on the initial ECG at rest in 0.2–2.2% of healthy children. When monitored on an outpatient basis, the smell widens and disappears in 20–30% of young children and in about 40% of young boys. Extrasystoles are primarily isolated, but their new morphologies are associated with periods of higher heart rate. In some cases, there are abundant focal extrasystoles, and in some cases, paired ectopic activity. The frequency of extrasystoles does not exceed 1–5 per year. In some individuals, there is a significantly greater frequency of ectopic activity or travails during periods of scapular hemorrhage. Extrasystoles of this type, which are known at the hour of desire, may be good in the future. This is confirmed even by the combined data of extreme caution. In the meantime, some caution is required. It has recently been found that in children with benign sectopic ectopy, the dispersion of the adjusted QT interval is greater than that of the control group. Pathologically increased dispersion of the QT interval is characteristic of patients with long QT interval syndrome. These values in children with benign sectopic ectopy will require further investigation.
In older children who participate in athletic training, ectopic activity occurs in approximately 50% of cases, similar to the frequency in healthy adults. In these cases, ectopic activity is not associated with changes in heart rate. Ectopic complexes are less likely to occur during the hour of sleep and emerge at a higher heart rate than in healthy individuals of the same age in the control group.
Isolated supraventricular ventricular short circuits tend to be wider in all age groups. In newborns, they were detected in 14% of seizures, and in older children - in 15–40%. Typically isolated ectopic complexes occur with a frequency of less than one per year, and in certain cases (often in newborns) - more often, up to 10 per year. If paired ectopic tachycardia, or persistent supraventricular tachycardia, is recorded, it is true that it has not been detected in healthy children.
Trival to the QRS complex
Normal values of the QRS complex, as determined by Davignon, were found in V5. In later studies, the maximum intensity of the QRS complex was identified in all findings, and this can explain the essential significance of the data from earlier and later studies. Beware of daily changes in the QRS complex. According to the Rijnbeek tables, the normal range is from 70–85 ms in newborns to 90–110 ms in adults. In the first three years of life, there are apparently insignificant changes, and later, the disturbance to the QRS complex increases linearly until reaching the middle age.
QT interval
The detection of a prolonged QT interval is important for the evaluation of individuals with an advanced risk of life-threatening arrhythmia. Looking at the length of the QT interval in relation to the frequency of the heart rate, as well as the frequency of the heart rate, the assessment of the QT interval in the pediatric age group is associated with early heart beats. Zagal has accepted the principle of correction depending on the frequency of the heart rhythm, but there is a debate about the method of this correction. We also discuss that it is necessary to take into account other factors, as we will become. In terms of practicality, the most common way to estimate the corrected QT interval (QTc) is to use the Bazett formula: the ratio of the actual QT interval to the square root of the trival interval. They were included in the investigations of Davignon and Rijnbeek. In both studies, the average QTc in children was approximately 410 ms, and the upper range of the norm reached 450 ms.
| Expanded indications for ECG registration in children • Diagnosis and treatment of congenital heart diseases • Diagnosis and treatment of arrhythmias • Diagnosis and treatment of rheumatic fever, Kawasaki disease, pericarditis, myocarditis • Syncope, judging and ''funny turns'' • Episodes of cyanosis • Chest pain or other symptoms during exercise • Family history of rape death or unsafe life • Electrical failures • Stagnation of drugs |
UPLIVER STATI
Uploading articles to the ECG parameters, notes earlier, systematically researched by Rijnbeek and colleagues. In all age groups, changes in the amplitude of the Q, R and S teeth were obvious in boys and girls. The intensity is greatest in the subsurgical region, if the amplitude of the Q, R and S waves is greater in the human condition in most of the thoracic outlets. In the 12–16th century group, these findings were considered reliable (Table 3). We would like to note that there are many risks to the fact that this information is not often used in everyday practice. Obviously, the understanding of the article's considerations will improve the sensitivity and specificity of the diagnostic criteria for scuticular hypertrophy in children.
In the age group 12–16 years of age, 95% of the centile intervals for boys and girls do not overlap.
Table 3. R wave amplitude (mV) in boys and girls at V1 and V6 levels according to Rijnbeek tables
| Median for boys (98% centile) | Median for girls (98% centile) | |||
| V1 | V6 | V1 | V6 | |
| 0–1 month | 1,1 (2,05) | 1,0 (1,78) | 1,35 (2,2) | 0,93 (1,64) |
| 1–3 months | 1,23 (2,07) | 1,55 (2,23) | 1,17 (1,99) | 1,51 (2,67) |
| 3–6 months | 1,32 (2,20) | 1,65 (2,73) | 1,14 (2,04) | 1,6 (2,8) |
| 6–12 months | 1,12 (2,14) | 1,7 (2,79) | 1,01 (1,92) | 1,68 (2,74) |
| 1–3 rocks | 1,08 (2,11) | 1,79 (2,96) | 1,01 (1,91) | 1,68 (2,67) |
| 3–5 rocks | 0,95 (1,78) | 1,98 (3,14) | 0,77 (1,38) | 1,89 (2,91) |
| 5–8 rocks | 0,63 (1,48) | 1,97 (2,98) | 0,55 (1,24) | 2,05 (3,25) |
| 8–12 rocks | 0,54 (1,14) | 2,18 (3,24) | 0,49 (1,14) | 2,0 (3,04) |
| 12–16 rocks | 0,48 (1,18) | 2,02 (3,05) | 0,35 (1,10) | 1,65 (2,52) |
In childhood, there is no current surge at ECG intervals, although some minor activities can be increased. The Rijnbeek tables show that the disturbance of the QRS complex is greater among boys of all age groups, less so among girls. However, the absolute magnitude is insignificant—approximately 2–5 ms for median QRS velocity—and obviously not significant for everyday practice. In pre-pubescent children, the increase in weight does not significantly affect the QT interval. The sublime age group has a small, but melodious, reliable quality. In the research of Rijnbeek, the upper limits of QTc standards were slightly closer for boys and girls. It has been established that QTc levels are significantly higher in girls over 14 years of age, which is obviously due to changes in boys and not increases in girls. In girls of the age group, a QTc of 460 ms is considered to be at the upper end of the norm.
VISNOVKI
The standards of normal values necessary for the interpretation of the ECG in children have been known for many years. Recently, recent research suggests that these standards will require revision through changes in the setting for ECG registration, and also, possibly, due to physiological changes in children. Changes in heart rate, which are expected in healthy children during the 24-year ECG registration, are welcome, but these changes (as they stink) were not systematically monitored.
Prepared by Oleg Zharinov
ECG for a child: features of the procedure
An ECG is performed on a child in the same way as on an adult. The only difference is that smaller sensors are used. To conduct the examination, the child is placed on his back on a couch, and sensors are connected to the chest, wrists and legs. Before connecting to the body, the sensors are treated with a degreasing agent. After connecting all the sensors, the device is turned on, which records the cardiogram, producing a tape with a graph. The duration of the procedure is about five minutes. The examination does not require special preparation; the only recommendation is to refrain from physical activity and stress 15 minutes before taking the cardiogram.
The first ECG is usually performed on a child in the first year of life as part of a mandatory medical examination. The sooner the diagnosis is carried out, the sooner pathologies can be identified and measures can be taken to eliminate them. When conducting an ECG, it is important to lie still while at rest, so in the case of a small child, it is advisable to have toys or a book with bright pictures on hand - these items will help keep the baby occupied during the examination and distract from inconvenience. A preventive ECG is also carried out in preschool age and upon entering first grade.
Indications for an unscheduled electrocardiogram include:
- developmental delay;
- high blood pressure;
- endocrine disorders;
- pain in the heart area;
- detection of murmurs when listening to the heart with a stethoscope;
- dizziness;
- dyspnea;
- fatigue and drowsiness;
- frequent ARVI;
- swelling of the limbs;
- pallor of the skin during physical activity.
Also, a reason for prescribing an examination is a hereditary predisposition to cardiovascular diseases. An ECG of the heart is a painless and absolutely safe diagnostic method, so the examination can be carried out frequently without any fear.
A cardiogram will not tell an untrained person anything - it’s just a graph with teeth, so after taking a cardiogram you need to contact a specialist. Cardiologists and functional diagnostic doctors decipher cardiograms. The decoding process involves studying the shapes and intervals of all teeth, as well as a comprehensive assessment of the cardiogram. An experienced specialist will be able to decipher the cardiogram, identify all deviations from the norm and make an accurate diagnosis.
Decoding indicators
Young children have peculiarities of heart function. It beats much faster than the heart of an adult. When conducting an ECG, indicators may differ from the accepted norm. However, small deviations are acceptable, so the doctor makes a diagnosis taking into account the size of the deviations, which have certain limits at each age.
A child’s body also has a number of features that a specialist takes into account when deciphering a cardiogram, so as not to make an erroneous diagnosis.
Experienced doctors at the Heratsi Center perform ECGs with maximum comfort for the child and parents; it is possible to conduct such functional diagnostics at home. Decoding is carried out by a doctor with an academic degree. You can find out the price of a heart cardiogram, doctors’ schedules and other information on the medical center’s website or by calling the 24-hour hotline +7-863-333-20-11.
Where to get an ECG in Volgograd
You can get an ECG for a child in Volgograd, Volzhsky and Mikhailovka at Dialine clinics. With us you can undergo the examination at a time convenient for you, without queues, by choosing the most suitable address. ECG examinations are carried out using modern high-precision equipment in comfortable conditions. Having made a cardiogram, you can immediately decipher it by contacting our specialists. High qualifications and extensive experience allow us to guarantee diagnostic accuracy. For ease of use of medical services, register in your personal account on our website.